Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.61 no.1 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3934
CASE REPORT
Borrowing from the Burrow's - using discarded tissue to improve lip reconstruction
M Paulsen; A Madaree; EA Xoagus
Department of Plastic and Reconstructive Surgery, Inkosi Albert Luthuli Central Hospital, South Africa
SUMMARY
Lip reconstruction following excision of cutaneous malignancy should be carefully planned to avoid discarding useful tissue. In this report, we describe two cases in which the usually discarded Burrow's triangles of the cheek advancement flap are used to reconstruct adjacent anatomical structures, thus improving the functional and aesthetic outcome of the reconstruction.
Keywords: lip reconstruction, Webster-Bernard, Burrow's triangle
Case report 1
A 72-year-old male presented with a fungating cutaneous squamous cell carcinoma. The mass measured 3.5 cm x 3 cm and involved approximately 80% of the upper lip, including the entire philtrum, columella base, and extended onto the edge of the nasal sill bilaterally. The majority of the vermillion was also involved. The gingival-labial sulcus and gingiva were not involved. He had no regional or distant metastases clinically, with a 7 mm left level 1b cervical lymph node on staging computed tomography (CT).
The patient underwent wide local excision of the lesion. Margins of 6 mm were used resulting in a 90% full-thickness central upper lip defect preserving both commissures.1 The columella base and bilateral nasal sills were also excised. Intraoperative frozen sections confirmed negative margins. Reconstruction was performed using bilateral cheek advancement flaps in the form of bilateral Webster-Bernard flaps. Bilateral Burrows triangles were designed along the superior lateral aspect of the nasolabial folds (NLFs) to achieve medial advancement of the flaps. Inferior Burrows triangles or Schuchardt incisions were not required as there was sufficient laxity to advance the flaps and there was no gathering of tissue medially.
Instead of excising the triangles along the NLFs, the Burrows triangles were raised as flaps with an inferior base attached to the superior lateral border of the advancement flaps. The flaps were tunnelled subcutaneously and transposed medially. The right triangular flap was used to reconstruct the right nasal sill as well as the columella base. The left triangular flap was used to reconstruct the left nasal sill. The bilateral cheek advancement flaps were advanced medially and used to reconstruct the cutaneous upper lip. The advanced cheek mucosa was everted to reconstruct the vermillion.
The patient had an uneventful postoperative course. On review six weeks post-surgery, the lip had fully healed. The patient reported good function with normal speech, good sensation and mouth opening, and no oral incontinence. Histology confirmed clear margins with no lymphovascular or perineural invasion. He was scheduled for bilateral neck dissection.
Case report 2
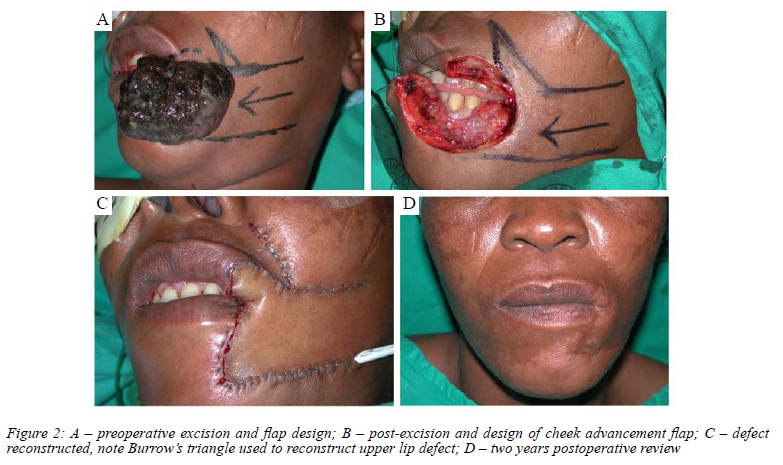
A 48-year-old female presented with a large, 7 cm x 7 cm nodular black-pigmented mass arising from the left lateral lower lip. The mass involved the labial mucosa of the lower lip, commissure and left lateral aspect of the upper lip, as well as the left upper and lower lip vermillion. Clinically the mass resembled a melanoma, confirmed with histology. No Breslow thickness was provided with the histology report. However, the report stated that the tumour invaded the subcutaneous tissue making it a Clarke level IV, with a Breslow depth of likely > 4 mm.
As recommended by guidelines, a 2 cm margin was used for excision. The post-excision full-thickness defect involved approximately 50% of the lower lip, the entire left commissure, approximately 30% of the upper lip and 2-3 cm of adjacent cheek skin.
A left cheek advancement flap in the form of a Webster-Bernard flap was designed. A superior Burrow's triangle was designed along the left nasolabial fold.
Similar to the first case, instead of excising a Burrow's triangle to achieve more medial advancement, the triangle was raised as a flap with an inferior base, attached to the cheek advancement flap, and transposed inferomedially to reconstruct the upper lip defect. The donor site was closed primarily.
The patient had a normal postoperative course. She was followed up two years postoperatively and reported good mouth opening and sensation of the left upper and lower lip, normal speech and no oral incontinence.
Discussion
The lips form a central and integral part of facial anatomy. As such, reconstruction of lip defects is an often-complex task. The causes of lip defects vary and include trauma with tissue loss, excision of cutaneous malignancy, previous surgery and congenital defects.2 In general, lip defects involving more than 30% of the lip will require reconstruction. Occasionally, excision of cutaneous malignancies of the lip may also require excision of adjacent structures, such as nasal elements, or the opposing lip.3 The reconstructive method chosen is determined by several factors, most notably the defect size and site, as well as the anatomical elements requiring reconstruction. Patient factors and surgeon preference/experience will also determine the method chosen. In reconstruction of the upper-lip, the relationships between vermillion, philtrum, ala and columella all need to be considered.3
Successful lip reconstruction is evaluated subjectively with attention to both form and function of the lip. Functional requirements of the lip are to assist in facial expression, speech and deglutition as well as the management of oral secretions. The lips play a key role in facial aesthetics with colour and texture being important considerations during reconstruction.2 Native lip tissue, when available, is preferred over distant tissue because of superior sensation, colour match and preserved orbicularis function, allowing for a dynamic reconstruction.2 Local options, which employ adjacent tissues, may be used for large defects whilst maintaining a degree of dynamism through the preservation of orbicularis function. Cheek advancement flaps are an excellent choice for such cases.
Distant tissue in the form of pedicled regional flaps or free flaps may be required in certain cases where defects totally exceed local tissue availability, however, these reconstructions are often adynamic, lack sensation, and have poor colour and texture match.2
Cheek advancement flaps have undergone multiple modifications since the initial description in 1845.4 The primary modification was made by Bernard who employed full-thickness Burrow's triangles, excised at the nasolabial groove, to achieve greater medial advancement of the cheek flaps.5 Webster and Freeman independently described partial-thickness excision, being skin and subcutaneous tissue only, of the Burrow's triangles in order to maintain orbicularis oris muscle integrity and thus function.67 A more recent modification, described by Brougham and Adams, utilises the usually discarded Burrow's triangles as V-Y advancement flaps to close the donor defect of the medially advanced cheek flap.8
In these cases, we demonstrate that the usually excised Burrow's triangles of the Webster-Bernard cheek advancement flap can be used to reconstruct adjacent structures such as nasal elements, or the opposing lip, leading to improved outcomes in terms of both form and function.
Gillies' so-called "Ten Commandments" of plastic surgery state within their number that "Thou shalt not throw away a living thing."9 Therefore, during reconstructive surgery all involved tissues are considered before excising and discarding "excess". Thoughtful and meticulous planning of excision and reconstruction allows one to make the most use of available tissues. In some cases, spare tissues may even be used to enhance the reconstruction of a certain defect to achieve a result as close as possible to pre-morbid function and aesthetics. We find the use of templates and paper diagrams to be particularly helpful in both the planning and execution phases of surgery.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
ORCID
M Paulsen https://orcid.org/0000-0001-8993-5002
A Madaree https://orcid.org/0000-0001-8661-0288
EA Xoagus https://orcid.org/0000-0001-6650-6192
REFERENCES
1. Newlands C, Currie R, Memon A, Whitaker S, Woolford T. Non-melanoma skin cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016;130(Suppl S2):S125-32. https://doi.org/10.1017/S0022215116000554. [ Links ]
2. Baumann D, Robb G. Lip reconstruction. Semin Plast Surg. 2008;22:269-80. https://doi.org/10.1055/s-0028-1095886. [ Links ]
3. Luce EA. Upper lip reconstruction. Plast Reconstr Surg. 2017;140:999-1006. https://doi.org/10.1097/PRS.0000000000003400. [ Links ]
4. Dieffenbach JF. Chirurgische Erfahrungen besonders uber die Wiederherstellung zerstorter Teile des menschlichen Korpers nach neuen Methoden. Bedim TCF Enslin. 1845:34-38. [ Links ]
5. Bernard C. Cancer de la levre infericure, restauration a l'aide de lambeaux quadrilataires lateraux. Scalpel. 1852;3:357-60. [ Links ]
6. Webster RC, Coffey RJ, Kelleher RE. Total and partial reconstruction of the lower lip with innervated muscle-bearing flaps. Plast Reconstr Surg Transplant Bull. 1960;25:360-71. https://doi.org/10.1097/00006534-196004000-00007. [ Links ]
7. Freeman BS. Myoplastic modification of the Bernard cheiloplasty. Plast Reconstr Surg Transplant Bull. 1958;21(6):453-60. https://doi.org/10.1097/00006534-195806000-00005. [ Links ]
8. Brougham ND, Adams BM. A modification of the Webster-Bernard lip reconstruction. Plast Reconstr Surg Glob Open. 2020;8:e2762. https://doi.org/10.1097/GOX.0000000000002762. [ Links ]
9. Millard DR Jr. Plastic peregrinations. Plast Reconstr Surg. 1950;5:26-53. https://doi.org/10.1097/00006534-195001000-00002. [ Links ]
 Correspondence:
Correspondence:
M Paulsen
Email: plsmur001@myuct.ac.za














