Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.1 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3907
CASE REPORT
Point-of-care ultrasound assessment of a swollen limb following snakebite envenomation - an adjunct to avoid fasciotomy
A SmitI; V LallooI; A EngelbrechtI; LD MashegoII; BI MonzonII, III
IDivision of Emergency Medicine, Department of Family Medicine, Steve Biko Academic Hospital, University of Pretoria, South Africa
IITrauma Unit, Department of Surgery, Steve Biko Academic Hospital, University of Pretoria, South Africa
IIIDepartment of Surgery, University of Pretoria, South Africa
SUMMARY
Acute limb compartment syndrome can occur with cytotoxic snake envenomation. Ultrasound (US) assessment of the affected limb has been suggested as an adjunct to the administration of snakebite polyvalent antivenom to ameliorate the systemic and local effects. US may also aid in the diagnosis of compartment syndrome and the need for fasciotomy to prevent limb loss. This report presents an adult male who had severe soft tissue swelling from a puff adder bite to the wrist and highlights the use of US in assessing and monitoring the degree of swelling in subcutaneous and fascial compartments of the arm. This US monitoring in conjunction with frequent physical examination avoided the need for a fasciotomy and its attendant morbidity, resulting in complete resolution of the swelling and full recovery of limb function.
Keywords: snakebite, envenomation, pseudo-compartment syndrome, fasciotomy, point-of-care ultrasound, POCUS, cytotoxic venom, painful progressive swelling
Case report
A 27-year-old man arrived at the emergency department approximately 2 hours after a bite on the left wrist from a puff adder (Bitis arietans), complaining of severe pain and swelling extending into the left axilla. He was fully conscious; his airway was self-maintained, and no respiratory distress was present. Vital signs included a blood pressure of 149/56 mmHg, pulse rate of 84 beats/minute, though the radial pulse was difficult to palpate. His respiratory rate was 16 breaths per minute.
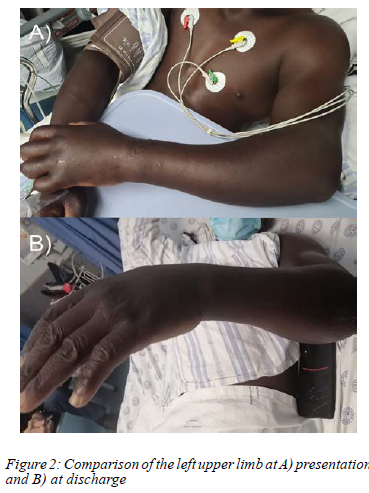
On examination of the left arm, significant swelling was appreciated extending up to the axilla, with fang marks noted on the volar aspect of the wrist, and no necrotic areas. He had significant limitation to both active and passive movement of his fingers, wrist and elbow. The swelling was tense and tender, particularly in the hand and forearm.
He was correctly diagnosed with painful progressive swelling (PPS) syndrome and after a dose of adrenalin as premedication, in anticipation of the possibility of anaphylaxis, four vials of polyvalent antivenom were administered and the arm was elevated.
Laboratory investigations revealed thrombocytopenia and a slightly prolonged international normalised ratio (INR), demonstrating cross-over haemotoxicity.
Twelve hours later, the swelling was stable but still tense, and the arm was still considered at risk for compartment syndrome due to severe pain and inability to move the joints. Fasciotomy was considered. Point-of-care ultrasound (POCUS) was performed to measure the subcutaneous and muscle compartments. It demonstrated subcutaneous tissue with increased echogenicity (in keeping with inflammation) and a thickness of 0.71 cm compared to 0.31 cm on the unaffected limb. The muscle compartments measured 4.3 cm on the affected side compared to 4.1 cm on the unaffected limb. Doppler flow was present in major arteries and muscles on both sides. A diagnosis of "pseudo-compartment syndrome" was thus made and an additional four vials of antivenom were administered. After 4 hours, repeat POCUS showed that the subcutaneous swelling was diminishing (0.68 cm) and on clinical examination, the upper arm and axillae were no longer swollen. Another two vials of antivenom were administered.
A third scan performed 4 hours later showed further reduction of swelling in the subcutaneous compartment (0.62 cm) and resolution of the swelling up to the level of the elbow. The decision was made to administer a final two vials of antivenom. A total of 12 vials of antivenom were administered over a period of 12 hours.
Twenty-four hours later, swelling was minimal. The subcutaneous tissue layer measured 0.47 cm. The patient was able to move all joints and the limb was no longer tense. Pain was easily controlled with oral analgesia.
He was admitted to the ward for clinical monitoring for the development of late necrosis and progressive haematological abnormalities, which did not occur. He was discharged home with a fully functional arm after 4 days.
Discussion
Venomous snakebites are common in Africa resulting in approximately 20 000 deaths per annum.1 It is estimated that > 7 000 amputations occur in Africa annually.1 Out of 176 snake species found in Southern Africa, 20 are considered highly venomous and potentially lethal.2
Snake venom has three distinct pathophysiological effects: cytotoxic, neurotoxic and haemotoxic. However, some snake venoms have overlapping effects resulting in mixed clinical pictures.3 Cytotoxic envenomation is by far the most common clinical presentation, resulting in PPS and late tissue necrosis.4
Cytotoxic snake venom contains digestive enzymes (proteolytic enzymes, phospholipases) and other poly-peptides that destroy tissues, including skeletal muscle. Tissue lysis increases capillary permeability resulting in local oedema, blistering, necrosis and gangrene. Southern African snakes responsible for bites which present as PPS syndrome are the spitting cobras (N. mossambica, N. nigricollis, N. nigricinta), Rinkhals and the large adders.
Swelling results from the proximal spread of venom via lymphatic vessels. It usually begins within 30 minutes of the bite, becomes extensive, involving the entire limb and may extend into the torso. This clinical presentation is typical in adder bites. Lymph nodes are often enlarged and painful in the first 60 minutes. Typically, skin blisters with fluid or blood as well as large ecchymotic areas appear in the first 24 hours. 'Skip lesions' are patches of necrosis characteristic in spitting cobra bites. Previously an unexplained phenomenon, many experts now believe them to simply be multiple bite sites. Extravasation of plasma may cause hypovolaemia in children. Skin necrosis and spontaneous sloughing occurs several days later.
Controversy and misunderstanding exist with regard to the diagnosis and management of what is perceived as an acute limb compartment syndrome associated with severe cytotoxic envenomation.5 Envenomation from a cytotoxic species may present with signs apparently suggestive of compartment syndrome such as severe pain, tense swelling and reduced or absent movement of major and minor joints of the affected limb. Many of these patients undergo an unnecessary fasciotomy, due to the misdiagnosis of pseudo-compartment syndrome as compartment syndrome.6 This results in delayed wound healing of the envenomated tissues, significant haemorrhage due to the associated haemotoxic effects (thrombocytopenia and increased INR), leading to increased morbidity with prolonged hospital stay and escalating costs.
The incidence of true compartment syndrome in PPS syndrome is reported to be between 2 and 6% and the need for fasciotomy 1.2 and 6.3%.7,8 Many of these cases result from inappropriate first aid treatment such as tourniquet application.3
Clinical differentiation between PPS syndrome and true compartment syndrome is nearly impossible, however, the pathophysiology differs significantly. In snakebite, severe subcutaneous swelling is present (i.e., pseudo-compartment syndrome), which is completely different from the muscular compartment swelling of traumatic injuries (true compartment syndrome).5
By its very nature and activity, cytotoxic venom, when rarely injected directly into a muscle compartment may result in primary muscle destruction not reversible by fasciotomy, as demonstrated in animal studies.9
Rapid administration of the correct dose of antivenom reduces the severity of PPS syndrome and the progression of the pseudo-compartment syndrome, avoiding the need for fasciotomy and its accompanying issues. Late tissue necrosis can be treated with surgical debridement when appropriate.
The use of POCUS, reported in observational studies, has demonstrated that the tense, painful, swelling resulting from cytotoxic envenomation affects mostly the subcutaneous space of the limb rather than the true muscle compartments.10 The procedure is less painful and assists in assessing the level of tissue involvement, assisting in determining the need for antivenom or surgical intervention.10 Ultrasound assessment of the affected limb has been suggested as an alternative to direct compartment pressure assessment (e.g., Striker or similar devices) to diagnose pseudo-compartment syndrome.8,10 Comparative measurements of the subcutaneous and muscle compartments in the affected vs unaffected limb can assist in guiding treatment strategies and preventing unnecessary fasciotomies.10
We propose that patients with PPS syndrome who develop clinical features of compartment/pseudo-compartment syndrome may be assessed with POCUS in the absence of other methods to assess intra-compartmental pressure and the degree of subcutaneous swelling. A policy of active observation and clinical evaluation is preferred over aggressive early surgical intervention, such as fasciotomy, together with rational use of antivenom and limb elevation in severe PPS syndrome.6
Conflict of interest
The authors declare no conflict of interest.
Funding source
The authors received no funding for this article.
Ethical approval
Written consent has been obtained from the patient in question for publication of the information contained in the article, as well as for the images included.
ORCID
A Smit: https://orcid.org/0000-0003-2229-7821
V Lalloo: https://orcid.org/0000-0002-5547-8461
A Engelbrecht: https://orcid.org/0000-0001-9846-189X
LD Mashego: https://orcid.org/0000-0003-2590-1780
BI Monzon: https://orcid.org/0000-0002-3543-6352
REFERENCES
1. Appiah B. Snakebite neglect rampant in Africa. CMAJ. 2012;184(1):E27-E28. https://doi.org/10.1503/cmaj.109-4046. [ Links ]
2. African Snikebite Institute [Internet]. c2021. Available from: https://www.africansnakebiteinstitute.com. Accessed 30 Mar 2022. [ Links ]
3. Blaylock RS. The identification and syndromic management of snakebite in South Africa. SA Fam Pract. 2005;47(9):48-53. https://doi.org/10.1080/20786204.2005.10873288. [ Links ]
4. Woods D, Sartorius B, Hift R. Snakebite in north-eastern South Africa - clinical characteristics and risk for severity. SA Fam Pract. 2016;1(1):1-6. https://doi.org/10.1080/20786190.2015.1120934. [ Links ]
5. Fry BG. Snakebite: when the human touch becomes a bad touch. Toxins. 2018;10:170. https://doi.org/10.3390/toxins10040170. [ Links ]
6. Campbell BT, Corsi JM, Boneti C, et al. Paediatric snakebites: lessons learned from 114 cases. J Ped Surg. 2008;43:1338-41. https://doi.org/10.1016/j.jpedsurg.2007.11.011. [ Links ]
7. Pattinson JP, Kong VY, Bruce JL, et al. Defining the need for surgical intervention following a snakebite still relies heavily on clinical assessment: the experience in Pietermaritzburg, South Africa. S Afr Med J. 2017;107(12):1082-5. https://doi.org/10.7196/SAMJ.2017.v107i12.12628. [ Links ]
8. Mars M, Hadley GP, Aitchison JM. Direct intracompartmental pressure measurement in the management of snakebites in children. S Afr Med J. 1991;80:227-8. [ Links ]
9. Cumpston KL. Is there a role for fasciotomy in crotalinae envenomations in North America? Clin Toxicol (Phila). 2011;49(5):351-65. https://doi.org/10.3109/15563650.201L597032. [ Links ]
10. Wood D, Sartorius B, Hift R. Ultrasound findings in 42 patients with cytotoxic tissue damage following bites by South African snakes. Emerg Med J. 2016;33(7):477-81. https://doi.org/10.1136/emermed-2015-205279. [ Links ]
 Correspondence:
Correspondence:
A Smit
Email: almien.boshoff@gmail.com














