Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.1 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3836
ENDOCRINE SURGERY
Retroperitoneoscopic adrenalectomy - introducing a new surgical technique in South Africa
W ConradieI; M ConradieII; E GeldenhuysI; J EdgeI; A CoetzeeII; A LambrechtsI
IDepartment of Surgery, Faculty of Medicine and Health Sciences, Tygerberg Academic Hospital, Stellenbosch University, South Africa
IIDivision of Surgery, Department of Medicine, Faculty of Medicine and Health Sciences, Tygerberg Academic Hospital, Stellenbosch University, South Africa
ABSTRACT
BACKGROUND: Posterior retroperitoneoscopic adrenalectomy (PRA) is purported to be superior to the laparoscopic transperitoneal approach (LA) in patients with a select spectrum of benign adrenal pathologies. Advantages attributed to the technique include minimal blood loss, shortened operative times, and decreased postoperative pain, explained anatomically by the direct access to the adrenal gland. Reduced workspace is a limitation
METHODS: A retrospective review of 22 consecutive PRAs performed in a single centre between 1 September 2016 and 30 October 2020 is presented. Two experienced laparoscopic surgeons operated on all patients after acquiring the technique at international centres. Suitable candidates were carefully pre-selected. Non-benign pathology, high vascularity, body mass index (BMI) > 45 kg/m2 and anatomical concerns on prior computed tomography (CT) imaging were exclusion criteria
RESULTS: Twenty-two PRAs were performed for a spectrum of benign adrenal pathologies. Twenty-one surgeries (95%) were completed. A single case of pheochromocytoma required conversion. The procedure was safe, a minor postoperative complication (pneumaturia) occurred in one case, and the mortality rate was 0%. Median operative time (80 minutes) is comparable to other reported series in the literature, with a modest linear descending tendency noted over the study period. Underlying pathology influenced operative times. Pheochromocytomas proved to be most challenging and required careful preoperative evaluation
CONCLUSION: The PRA procedures performed at Tygerberg Academic Hospital were safe and reproducible in a select group of cases with benign adrenal pathology. Endocrine surgeons proficient with laparoscopic techniques should be encouraged to use the PRA approach when encountering adrenal neoplasms that fit the criteria
Keywords: adrenalectomy, posterior retroperitoneoscopic adrenalectomy, benign adrenal pathology, operative times, pheochromocytoma, adrenal
Introduction
Laparoscopic adrenalectomy (LA), first performed in 1992, is safer, more effective and less invasive than traditional open posterior and transabdominal approaches. The technique ensures a rapid return to baseline daily activity, is associated with minimal blood loss, less postoperative pain and reduced surgical time.1-4 Therefore, the laparoscopic approach is superior to the traditional open methods and is established as the gold standard for adrenal surgery.13
The anatomical location of the adrenal gland, characteristically situated in the upper retroperitoneal space, facilitated the development of alternative laparoscopic approaches. Compared to the standard transperitoneal (TP) technique, retroperitoneal endoscopic methods have gained popularity over the last decade, and posterior retroperitoneoscopic adrenalectomy (PRA) has brought about a paradigm shift in the surgical treatment of adrenal lesions.56 This technique facilitates immediate and direct access to the adrenal gland (Figure 1A) without traversing the abdominal cavity. Therefore, PRA may be superior to the anterior and lateral LA methods.7 Barczynski and colleagues confirmed decreased intraoperative blood loss, reduced postoperative pain, and less shoulder-tip discomfort with PRA compared to TP. In addition, the same study group reported reduced time to oral intake after surgery, faster and improved ambulation, shortened length of hospital stay, and ultimately, lower cost.8
The increased use of PRA globally has also led to modifications of the traditional PRA procedure.7 Walz and colleagues proposed a PRA technique where access is gained posteriorly from below the twelfth rib with the patient positioned kneeling in the prone position (Figure 1B). Three ports (balloon port, 10 mm port, 5 mm port) are placed, and the retroperitoneum is inflated with CO2 to maintain a pressure of 20-30 mmHg. This is followed by surgical mobilisation of the upper pole of the kidney and dissection of the adrenal gland from lateral to medial. The adrenal gland is subsequently lifted to locate and ligate the adrenal vein with the Maryland Ligasure®, considering the variation in left and right venous anatomy. Meticulous resection of the rest of the adrenal gland aims to prevent capsular injury.7
Notably, a limitation of the PRA approach is the reduced working space. This is accentuated in patients with a high body mass index (BMI) and larger lesions. Therefore, the TP technique is preferred in adrenal lesions larger than 6-8 cm maximum dimension, in patients with a BMI exceeding 45 kg/m2, and in a suspected adrenocortical carcinoma (the latter being a contraindication due to the risk of capsular injury and seeding7).
Despite gaining international recognition, the PRA approach has been used infrequently in South Africa. Most local surgeons still prefer the TP technique with a familiar and wider working space. The PRA technique was introduced to the endocrine surgery unit at Tygerberg Hospital (TBH) in September 2016 after the local endocrine surgeons obtained surgical experience at international centres proficient in the PRA technique (Prof. Julie Miller, Melbourne,9 and Prof. Martin Walz, Germany7). At TBH, the PRA technique is now the standard approach for patients with benign adrenal lesions meeting criteria.
We report on the first 22 PRAs performed by two surgeons at TBH. The aims were to elucidate this approach's applicability, outcomes and safety, and reflect on the learning curve in terms of operative time.
Materials and methods
A retrospective review of 22 consecutive PRAs performed in a single centre between 1 September 2016 and 30 October 2020 is presented. TBH is an academic hospital in the Western Cape of South Africa and serves as a tertiary referral hospital. Two surgeons, WC and AL, experienced in laparoscopic operations, perform all adrenal surgery.
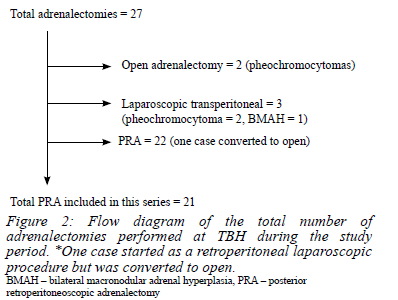
Patients with functional and non-functional adrenal tumours < 6 cm without clinical, biochemical, or radiological concern for adrenocortical carcinoma were included. The TP approach was selected when there was a high likelihood of conversion to laparotomy. The following served as exclusion criteria: lesions with marked vascularity, anatomical challenges concerning proximity and adherence to vascular structures on computed tomography (CT) imaging, patients with a high BMI (> 45 kg/m2) and concomitant intra-abdominal pathology (Figure 2).
Data were collected from clinical and surgical notes, radiology reports from the picture archiving and communications system (PACS), and pathology reports obtained from the National Health Laboratory Service (NHLS). Variables of interest included: patient-related variables (i.e., age, gender, and BMI), disease-related variables (i.e., morphology and function of tumour based on clinical, biochemical, and imaging characteristics, laterality, and final histology), and procedure-related variables (i.e., operative time, complications, and conversion to laparotomy).
Data were analysed using the IBM Statistical Package for the Social Sciences (SPSS) version 26. Descriptive statistics were computed for demographic and clinical variables of interest and presented as mean and standard deviation (SD) for continuous variables (or median and interquartile range [IQR], where appropriate) and counts and associated percentages for categorical variables. The Mann-Whitney U test was used to compare operative times between the first 11 and the last ten cases. Statistical significance was set at p < 0.05.
Approval was obtained from the Health Research Ethics Committee (HREC) of the University of Stellenbosch, approval number N18/10/115. A waiver of informed consent was provided, given the study's retrospective nature, and all data were de-identified.
Results
Twenty-two PRA procedures were performed between 1 September 2016 and 30 October 2020. The same surgeons who learned the PRA technique in 2016 operated together on all patients.
Patient characteristics, operative outcomes, and final histological diagnoses are presented in Tables I and II. The mean age of the participants was 45 years (SD 16 years; range 23-72 years), and 17 (77%) were female. Weight and height were recorded in 21 of the 22 patients. The mean BMI was 31.6 kg/m2 (SD 6.7; range 22-44 kg/m2). Based on the World Health Organization diagnostic criteria, 16 (76% of known BMIs) patients were overweight (BMI > 25), and 11 (52%) were obese (BMI > 30).10
Adrenal imaging was performed for 13 patients with suspected adrenal endocrinopathy, three as part of staging for breast cancer, one as part of surveillance for known multiple endocrine neoplasia type 2a (MEN2a) syndrome, and four were true incidentalomas. Seventeen (77%) of the adrenal lesions in this series were functional adenomas. Seven autonomously produced aldosterone, five cortisol, and five catecholamines. The patient with MEN2a and one case with an incidentaloma had biochemically confirmed catecholamine excess. Two patients had subclinical Cushing's syndrome that prompted the need for surgery. None of the adrenal lesions identified as part of staging for breast cancer were functional (Table I). The indications for surgery in the non-functional adenomas were diagnostic in four cases and pain in one case.
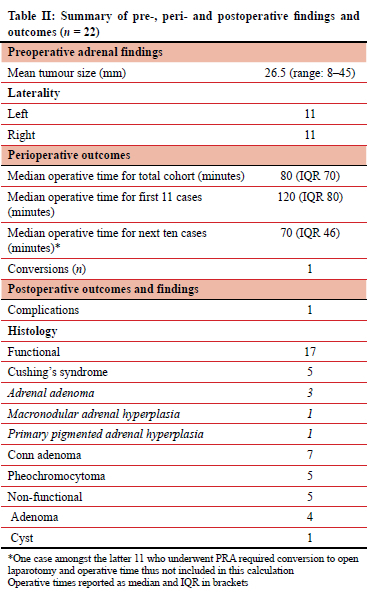
The mean lesion size, based on imaging, was 26.5 mm (SD 13.6; range 8-52 mm). Eleven tumours were in the left adrenal and 11 on the right. Of the 22 patients who underwent PRA, only one case (5%) was converted to open laparotomy. The conversion was necessitated due to excessive intraoperative bleeding. The adrenal lesion was an incidentally discovered pheochromocytoma on a CT scan following abdominal trauma in a 42-year-old male. The tumour was large (i.e., 49 mm in largest diameter), very vascular, and closely related to the inferior vena cava (IVC) and the right crus of the diaphragm. Postoperatively, one patient developed pneumaturia. There were no postoperative fatalities or other adverse events. The operative time for the 21 completed PRAs ranged between 45 and 195 minutes, with a median operative time of 80 minutes (IQR 70).
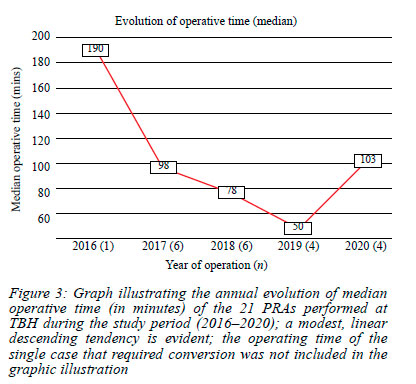
When comparing operative times between the first 11 and the last ten cases (excluding the patient who required the conversion procedure), the median operative time for the previous ten cases was less compared to the initial 11 cases operated (70 minutes; IQR 46 vs 120 minutes; IQR 80). However, the difference in operative time was not statistically significant between the two groups. This may be due to the wide range within groups and the limited number of procedures. The length of operation appeared to be influenced by the underlying pathology (Table II). The four PRA procedures with the most prolonged duration in this study were the first two procedures for non-functional adenomas (operation times of 190 and 130 minutes, respectively) and two where multicentric pathology was the cause of clinical and biochemical Cushing's syndrome (one case with PPNAD, time = 140 minutes and one case with bilateral macronodular adrenal hyperplasia (BMAH), time = 195 minutes). The annual evolution of operative times is illustrated in Figure 3. A modest linear descendant tendency was noted for operative times over the study period.
Histological examination confirmed the clinical and biochemical diagnosis of the functional lesions in all but one case. Preoperatively, subclinical, biochemical cortisol excess was ascribed to bilateral adrenal macronodular hyperplasia in two cases but was noted on histology due to primary pigmented micronodular hyperplasia in one of the patients. Radiologically, indeterminate morphology was reported in 11 of the cases; all five pheochromocytomas had indeterminate imaging characteristics (100%). The other six indeterminate lesions were all confirmed adenomas on histology (four non-functional, one cortisol producing and one aldosterone producing).
Discussion
This study reports on the first 22 cases that underwent PRA in our unit. The same two surgeons with experience in laparoscopic surgery operated on all patients. The PRA technique was learned at international centres, with training provided by surgeons proficient with this technique (Prof. Julie Miller, Melbourne9 and Prof. Martin Walz, Germany7). The PRA technique proved successful and safe after the careful preoperative selection of suitable candidates. Only one case required conversion from PRA to TP, one minor postoperative complication (pneumaturia) was encountered, and the mortality rate in this series was 0%.
Many surgeons still prefer the TP approach. They feel safer traversing the traditional peritoneal space and are generally unfamiliar with the retroperitoneal approach and the lack of anatomical references at the start of the procedure. Prior training in this technique, with direct input and guidance from an experienced surgeon, is paramount. Port placement is challenging when learning this operation, especially in obese cases, and a recalculation of orientation is helpful throughout the procedure.
Given our limited experience with this technique when it was introduced at TBH in 2016, patients were carefully pre-selected for the PRA technique to ensure safety. It is anticipated that more extensive regional exposure is required in patients with suspected non-benign adrenal pathology, those with large lesions, and where preoperative imaging indicates marked vascularity and adherence to vascular structures. Given the known reduced workspace associated with the PRA technique, these patients were thus not considered for inclusion. In addition, although regarded as an ideal approach for the obese patient, those with a BMI exceeding 45 kg/m2 were excluded as excess visceral fat and anticipated obstruction by the abdominal wall may further reduce workspace.
Compared to the transperitoneal route, the PRA approach has advantages. The technique facilitates easy and direct access to the adrenal gland without entering the intra-abdominal cavity, thereby preventing intra-abdominal visceral injury.11 Only three trocar sites are needed to access the retroperitoneal space.12 In addition, the PRA technique is regarded as a more practical approach in obese patients (i.e., with a BMI between 30 kg/m2 and 45 kg/m2) and in patients with previous abdominal surgery.11,13 We encountered difficult port placements in some cases with higher BMIs. Due to the concern that the abdominal wall cannot 'fall away' and open the retroperitoneal space, we opted to exclude morbidly obese patients with a BMI of more than 45 kg/m2, in accordance with other laparoscopic surgeons who utilise this technique.
Although the lateral decubitus retroperitoneoscopic approach has been well described in the literature, the prone kneeling position for PRA may be superior as it not only allows for bilateral adrenal access without changing the patient's position, but also permits a clear and sufficient view of the renal hilum and adrenal vasculature.11,14 Although adrenal vein variations are known to occur, particularly on the right side, the adrenal veins in our cases were easily identified, exposed, and dissected. Using only vessel sealing instruments (e.g., LigaSureTM) when taking the adrenal vein is essential, avoiding the use of any clips. The relatively high retroperitoneal pressure prevents intraoperative bleeding, with a Liga Clip® having a risk of slipping off the thin-walled IVC. It is critical to ligate the vein close to the adrenal gland (especially on the right) to prevent injury to the IVC.
The only patient in our cohort who underwent conversion to open surgery was a case in which pheochromocytoma was incidentally discovered on abdominal CT performed for trauma. This tumour was large (49 mm), very vascular, and closely related to the renal vessels, IVC, and the right diaphragmatic crus. Excessive bleeding necessitated the conversion of the surgical approach. The patient was repositioned onto his back to allow for the laparotomy, the retroperitoneal space was packed with Raytec gauze, and the 'closed' space of the retroperitoneum limited the bleeding and prevented the need for blood transfusion.
Another case with a pheochromocytoma had a difficult PRA dissection due to a low-lying left adrenal tumour and proximity to the renal vessels. An intraoperative bleed complicated the procedure. Following compression of the bleeding, a minor arterial bleed was identified and ligated with two Liga Clip®'s without needing a blood transfusion. The process was challenging and emphasised the importance of knowing and accurately identifying arterial anatomy, especially in patients with pheochromocytomas. Based on our experience, pheochromocytomas that are classically vascular tumours should be carefully assessed preoperatively in terms of vascularity, size, and location, and a low threshold for an anterior approach should be maintained in this subgroup of patients with adrenal pathology.
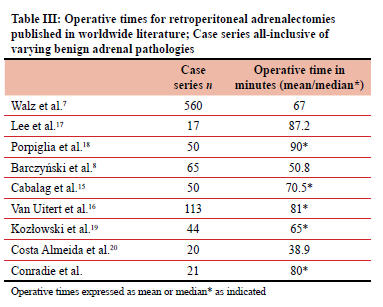
Significant variation in operative time amongst the 21 patients who had complete PRAs was encountered in our study. The median operative time was 80 minutes. The median operative time for the first half of the cohort was 120 minutes which was reduced to 70 minutes for the latter half, indicative of a modest learning curve. Operative times documented in the literature vary and are expressed as either mean or median operative times. Our median times are comparable to many reported case series (Table III).7,8,15-20 In the 560 cases initially reported by Walz et al. in 2006, the mean operating time was 67 minutes. This declined significantly from the earlier procedures (106 minutes for the first 112 operations) to the more recently performed (40 minutes for the last 112 cases). The authors noted longer operating times in male patients with pheochromocytomas, right-sided tumours and in tumours exceeding 3 cm.7 A learning curve with reduced operative times is reported in most of the mentioned case series of PRAs.
Interestingly, PRAs for single functional cortical adenomas (n = 10) took a median time of 60 minutes to complete, compared to 118 minutes for the pheochromocytomas and 75 minutes for the non-functional adenomas. The two operations where multicentric pathology was the cause of clinical and biochemical Cushing's syndrome (PPNAD, BMAH) took 140 and 195 minutes, respectively. Given the limited numbers, care must be taken when interpreting these findings.
The operative times for the first two cases, both nonfunctional cortical adenomas, were two of the longest noted in our cohort and may reflect surgeon caution and inexperience rather than implying an influence of specific pathology on the duration of surgery. That said, our findings suggest that pheochromocytoma surgery and operations for multinodular adrenal pathology are more time-consuming and possibly more technically challenging than surgery for cortical adenomas.
According to a study by Baba and colleagues, the operating time associated with a PRA is 50 minutes shorter on average when compared to the lateral retroperitoneoscopic and open adrenalectomy approaches.12,21 We did not formally compare the operating time of PRAs with other techniques used within our department. In doing so, one must be careful not to introduce bias. The PRA technique is confined to a specific subset of patients and not necessarily comparable to the cohort selected to undergo lateral retroperitoneoscopic and open adrenalectomy.
After performing 22 cases of PRA, the authors documented safety, technical feasibility, minimal morbidity, and no mortality with the newly introduced technique in a preselected patient group. The study's findings should not be extrapolated to include all patients presenting with adrenal pathology. PRA is now the standard of care at TBH but only utilised in the absence of the abovementioned contraindications.
Conclusion
The PRA procedures performed at TBH have been shown to be safe and reproducible in a select group of cases with benign adrenal pathology. Endocrine surgeons proficient with laparoscopic techniques should be encouraged to use the PRA approach when encountering adrenal neoplasms that fit the criteria.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Ethical approval was obtained from the Health Research Ethics Committee (HREC) of Stellenbosch University (N18/10/115).
ORCID
W Conradie https://orcid.org/0000-0002-9220-331X
M Conradie https://orcid.org/0000-0003-3092-4098
E Geldenhuys https://orcid.org/0000-0002-2733-8170
J Edge https://orcid.org/0000-0003-3005-7254
A Coetzee https://orcid.org/0000-0001-9993-6439
A Lambrects https://orcid.org/0000-0003-0565-3978
REFERENCES
1. Gagner M, Lacroix A, Prinz RA, et al. Early experience with laparoscopic approach for adrenalectomy. Surgery. 1993;114(6):1120-25. [ Links ]
2. Lee J, El-tamer M, Schifftner T, et al. Open and laparoscopic adrenalectomy: analysis of the national surgical quality improvement program. J Am Coll Surg. 2008;206(5):953-9. https://doi.org/10.1016/jjamcollsurg.2008.01.018. [ Links ]
3. Smith CD, Weber CJ, Amerson JR. Laparoscopic adrenalectomy new gold standard. World J Surg. 1999;23(4):389-96. https://doi.org/10.1007/PL00012314. [ Links ]
4. Jankulovski N, Stankov O, Stavridis S, Saidi S. Laparoscopic adrenalectomy: first single-centre experience in the Balkans. Pril (Makedone Akad Nauk Umet Odd Med Nauki). 2015;36(3):27-33. https://doi.org/10.1515/prilozi-2015-0075. [ Links ]
5. Kiriakopoulos A, Economopoulos KP, Poulios E, Linos D. Impact of posterior retroperitoneoscopic adrenalectomy in a tertiary care centre: a paradigm shift. Surg Endosc. 2011;25(11):3584-9. https://doi.org/10.1007/s00464-011-1762-6. [ Links ]
6. Walz MK, Peitgen K, Hoermann R, et al. Posterior retroperitoneoscopy as a new minimally invasive approach for adrenalectomy: results of 30 adrenalectomies in 27 patients. World J Surg. 1996;20(7):769-74. https://doi.org/10.1007/s002689900117. [ Links ]
7. Walz MK, Alesina PF, Wenger FA, et al. Posterior retroperitoneoscopic adrenalectomy - results of 560 procedures in 520 patients. Surgery. 2006;140(6):943-50. https://doi.org/10.1016/j.surg.2006.07.039. [ Links ]
8. Barczynski M, KonturekA, Nowak W. Randomised clinical trial of posterior retroperitoneoscopic adrenalectomy versus lateral transperitoneal laparoscopic. Ann Surg. 2014;260(5):740-8. https://doi.org/10.1097/SLA.0000000000000982. [ Links ]
9. Miller JA, Kwon DS, Dkeidek A, et al. Safe introduction of a new surgical technique: remote telementoring for posterior retroperitoneoscopic adrenalectomy. ANZ J Surg. 2012;82(11):813-6. https://doi.org/10.1111/j.1445-2197.2012.06188.x. [ Links ]
10. Romero-Corral A, Somers V, Sierra-Johnson J, et al. Accuracy of body mass index to diagnose obesity in the us adult population. Int J Obes. 2008;32(6):959-66. https://doi.org/10.1038/ijo.2008.11. [ Links ]
11. Walz MK, Peitgen K, Walz MV, et al. Posterior retroperitoneoscopic adrenalectomy: lessons learned within five years. World J Surg. 2001;25(6):728-34. https://doi.org/10.1007/s00268-001-0023-6. [ Links ]
12. Sasagawa I, Suzuki Y, Itoh K, et al. Posterior retroperitoneoscopic partial adrenalectomy: clinical experience in 47 procedures. Eur Urol. 2003;43(4):381-5. https://doi.org/10.1016/S0302-2838(03)00087-3. [ Links ]
13. Dickson PV, Alex GC, Grubbs EG, et al. Posterior retroperitoneoscopic adrenalectomy is a safe and effective alternative to transabdominal laparoscopic adrenalectomy for pheochromocytoma. Surgery. 2011;150(3):452-8. https://doi.org/10.1016/j.surg.2011.07.004. [ Links ]
14. López PJ, Pierro A, Curry JI, Mushtaq I. Retroperitoneoscopic adrenalectomy: an early institutional experience. J Pediatr Urol. 2007;3(2):96-99. https://doi.org/10.1016/j.jpurol.2006.05.010. [ Links ]
15. Cabalag MS, Mann GB, Gorelik A, Miller JA. Posterior retroperitoneoscopic adrenalectomy: outcomes and lessons learned from initial 50 cases. ANZ J Surg. 2015;85(6):478-82. https://doi.org/10.1111/ans.12508. [ Links ]
16. Van Uitert A, D'Ancona FCH, Deinum J, Timmers HJ, Langenhuijsen JF. Evaluating the learning curve for retroperitoneoscopic adrenalectomy in a high-volume centre for laparoscopic adrenal surgery. Surg Endosc. 2017;31(7):2771-5. https://doi.org/10.1007/s00464-016-5284-0. [ Links ]
17. Lee CR, Walz MK, Park S, et al. A comparative study of the transperitoneal and posterior retroperitoneal approaches for laparoscopic adrenalectomy for adrenal tumours. Ann Surg Oncol. 2012;19(8):2629-34. https://doi.org/10.1245/s10434-012-2352-0. [ Links ]
18. Porpiglia F, Fiori C, Bertolo R, et al. Laparoscopy and robotics mini-retroperitoneoscopic adrenalectomy: our experience after 50 procedures. Urology. 2014;84(3):596-601. https://doi.org/10.1016/j.urology.2014.04.040. [ Links ]
19. Kozlowski T, Choromanska B, Wojskowicz P, et al. Laparoscopic adrenalectomy - lateral transperitoneal versus posterior retroperitoneal approach: prospective randomised trial. Wideochir Inne Tech Maloinwazyjne. 2019;14(2):160-9. https://doi.org/10.5114/wiitm.2019.84694. [ Links ]
20. Costa Almeida CE, Caroço T, Silva MA, et al. An update of posterior retroperitoneoscopic adrenalectomy - case series. Int J Surg Case Rep. 2020;71:120-5. https://doi.org/10.1016/j.ijscr.2020.04.101. [ Links ]
21. Baba S, Miyajima A, Uchida A, et al. A posterior lumbar approach for retroperitoneoscopic adrenalectomy: assessment of surgical efficacy. Urology. 1997;50(1):19-24. https://doi.org/10.1016/S0090-4295(97)00119-2. [ Links ]
 Correspondence:
Correspondence:
W Conradie
Email: ilnaconradie@sun.ac.za














