Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.1 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3862
COLOPROCTOLOGY
Outcomes of haemorrhagic radiation proctitis at a South African tertiary hospital
MI JaliI; Y MoodleyI, II; S KaderI; S CheddieI
IGastrointestinal Cancer Research Group, Department of Surgery, University of KwaZulu-Natal, South Africa
IIDepartment of Global Health, Stellenbosch University, South Africa
ABSTRACT
BACKGROUND: Haemorrhagic radiation proctitis occurs in 5-10% of patients undergoing radiotherapy. In our resource-constrained South African setting, this study aimed to describe the clinicopathological spectrum and management of radiation proctitis referred to a tertiary centre, to address the deficit in our setting-specific understanding of the condition
METHODS: This was a sub-analysis of data from an existing colorectal cancer registry at the Inkosi Albert Luthuli Central Hospital in Durban. We reviewed the registry for all patients between 2008 and 2019 with haemorrhagic radiation proctitis and describe the various patient characteristics, treatments and outcomes for these patients
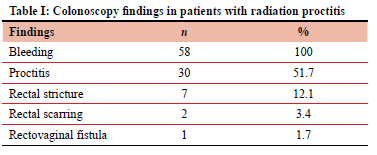
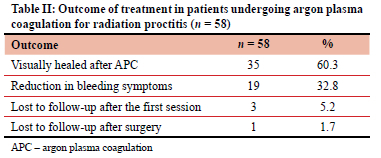
RESULTS: Fifty-eight patients with haemorrhagic radiation proctitis were identified. Colonoscopy findings included bleeding (58 patients), endoscopic proctitis (30 patients) and rectal stricture (7 patients). The median time elapsed between radiotherapy and development of symptoms was 16.5 months (IQR 12-25). Median number of argon plasma coagulation (APC) sessions for endoscopic healing or symptom resolution was three sessions (IQR 2-4). At follow-up, 35 patients had complete healing and 19 patients had symptom improvement. Complications occurring during or after APC therapy included rectal ulceration (2 patients) and rectovaginal fistula (1 patient
CONCLUSION: APC is a safe and effective treatment modality with complete resolution or significant improvement in symptomatology in the vast majority of patients with three or four treatments. Morbidity is likely to be related to ongoing radiation effects
Keywords: chronic radiation proctitis, argon plasma coagulation, radiation-induced enteritis, endoscopic management
Introduction
Radiation therapy (radiotherapy) is a vital modality for the treatment of malignancy.1,2 Radiotherapy can be used as monotherapy or part of multi-modal therapy.1,3,4 Its beneficial effects against malignancy are usually offset by its unintended complications.1 One of the commonly seen complications is radiation-induced enteritis, which is defined as direct inflammation of the gastrointestinal (GI) mucosal membranes.3,4 When this enteritis is confined to the rectum following pelvic radiation, it leads to radiation proctitis. Radiation-induced proctitis is reported to occur in 5-20% of patients receiving pelvic radiation.23 Bleeding occurring in 29-89.6% of patients can lead to iron deficiency anaemia that may require hospital admission as well as blood transfusions.4,5 Rectal bleeding has been noted to affect quality of life as well as daily routines in up to 6% of patients post pelvic radiation.5
Radiation proctitis is classified as acute or chronic depending on development of symptoms relative to the initiation of radiotherapy.1-3,6 In acute radiation proctitis the symptoms begin to appear within three months of commencement of pelvic radiation and are self-limiting, usually abating within six months of completion of radiation.126 Chronic radiation proctitis occurs in 5-10% of patients undergoing radiotherapy,2,6 and it occurs as a continuation of acute radiation proctitis beyond 6 months or onset of new symptoms 3-6 months after completion of radiotherapy.1-3,6 The reason for the propensity of the rectum to radiation injury is related to its fixity in the pelvis and constant exposure to radiation.2,4,6
Chronic radiation proctitis is related not only to the dose of radiation delivered but to other patient-related factors such as age > 60, low BMI, smoking, diabetes, hypertension, peripheral vascular disease, inflammatory bowel disease and HIV infection.4,7-9
Pathophysiology of acute radiation proctitis is thought to arise from radiation-induced damage to rapidly dividing crypt cells and intestinal mucosa.2,3,10 Chronic radiation proctitis is the result of vascular endothelial damage resulting in obliterative endarteritis and fibrosis of the rectal mucosa with stricturing and fistulation.1-3,6,10 Symptoms of radiation proctitis include lower gastrointestinal bleeding, diarrhoea, tenesmus, urgency, obstruction and fistula formation.2,3,6,10 Advances in radiotherapy, such as better focused delivery dose adjustment, reduce irradiation to surrounding tissue and hence the risk of complications.
There is no consensus on the gold standard for managing haemorrhagic radiation proctitis. Management options include non-surgical (medical and endoscopic) and surgical measures with non-surgical management as the mainstay.1,2,11 Medical measures include the use of sucralfate and 5-aminosalicylic acid (ASA), while endoscopic measures include the use of argon plasma coagulation (APC), formalin application and cryoablation amongst others.1,2,11-13 APC is available at tertiary centres and formalin is used at regional and district level. In our resource-constrained South African setting, literature is scarce and limits our understanding and management of this condition. In order to address this dearth, we sought to describe the clinical spectrum and outcome of APC management of haemorrhagic radiation proctitis in patients attending a South African tertiary hospital.
Methods
This study was a sub-analysis of patient data collected at the colorectal unit associated with the Inkosi Albert Luthuli Central Hospital (IALCH), a tertiary referral hospital in Durban, the main coastal city in the KwaZulu-Natal (KZN) Province with a population of 10 million people.14
The study population was comprised of patients diagnosed with radiation proctitis by colonoscopy at either IALCH or a referral hospital who underwent APC at IALCH between 2008 and 2019. These patients were identified, and their data extracted from the colorectal carcinoma (CRC) database established in 2000.15 Database variables were merged with follow-up data that were obtained from the password-protected hospital information management system (Soarian®, Siemens, USA). Data analysed included demographics, primary pathology, types of radiation and treatment outcome. Data related to primary admission and use of blood transfusion at base hospital were not obtained. Patients underwent initial colonoscopy to establish the cause of bleeding and identify any other pathology. The main outcome measures were healing of the proctitis on flexible sigmoidoscopy and symptom resolution or improvement.
The method used to treat the haemorrhagic proctitis was APC. APC is a non-contact thermal method of coagulation and haemostasis that utilises a jet of argon gas as a conducting medium which is delivered to the tissue by a bipolar diathermy via a colonoscopy catheter.1,2,6,10 It is delivered via a probe under endoscopic vision allowing for more proximal rectal lesions to be addressed.2 The application of the probe does not touch the target; the current jumps from the probe to the target lesion with the arc of energy transfer broken once the tissue is desiccated.1,2,6,8,10 The coagulation is predictable and achieves a uniform depth of thermal injury of approximately 0.5-3 mm.2,6,8
The data were descriptively analysed and expressed as median with interquartile range (IQR) for continuous variables and frequencies with percentages for categorical variables. Microsoft Excel was used to conduct the descriptive analysis.
Results
Fifty-eight patients were treated for radiation proctitis during the study period. There were 55 females. The median age at presentation with radiation proctitis was 52 years (IQR 44.5-61.5). The primary pathology requiring radiation therapy was cervical cancer which was found in 52 patients along with endometrial cancer (2 patients) and anal cancer (1 patient), while prostatic cancer was noted in all male patients.
All patients presented to their base hospitals with lower GI haemorrhage and were subsequently referred to IALCH. It was not documented if any of these patients required transfusion at their base hospital. One patient had a rectovaginal fistula (RVF) on initial assessment at IALCH colorectal unit. The findings at colonoscopy are shown in Table I with bleeding occurring in all patients. The median elapsed time between the completion of radiation and the presentation with the symptoms of radiation proctitis was 16.5 months (IQR 12.0-23.0). Two patients had previous treatment with topical formalin prior to referral to the unit with no success.
Fifty-seven patients underwent APC treatment. The median number of APC sessions was three (IQR 2-4). One patient underwent pelvic exenteration as a result of haemorrhage and disease progression. The patient with radiation-induced fistula underwent conservative management of the fistula.
Patients were followed up for median of 8 months (IQR 4-18). The outcome of treatment as seen at last follow-up is shown in Table II including four patients being lost to follow-up. Residual pathology following APC was seen in four patients, namely residual proctitis (1 patient), anorectal stricture (2 patients) and RVF (1 patient). None of the patients died during treatment or follow-up.
Discussion
Patients who had pelvic radiotherapy complications presented to IALCH with lower GI haemorrhage and proctitis, and needed to be investigated by proctoscopy, sigmoidoscopy or colonoscopy to ascertain the cause of the bleeding.4,8,11 History of radiotherapy should alert the treating clinician to the high probability of radiation induced proctitis and biopsies should be avoided unless there is suspicion of malignancy or inflammatory bowel disease for fear of poor healing and risk of fistulation.7-9 Other radiation associated complications of RVF and stricture were rare in this series and always occurred in association with bleeding. The study population did not include patients with the non-haemorrhagic complications, obstruction and RVF that are currently managed by the referral hospital with a surgical stoma.
There are no clearly defined treatment guidelines in the management of chronic haemorrhagic radiation proctitis.7,16 The mainstays of therapy are medical and endoscopic treatments with surgery being reserved for uncontrolled bleeding of other associated complications.1,2,6,8-11,17 Non-surgical interventions include the endoscopic method used in this study (APC),1,2,4,5,12 topical formalin applications,1,6 radiofrequency ablation (RFA),1,2,6 cryoablation,2,6 hyper-baric oxygen therapy (HBOT)2,4,6,9,11 and medical treatments, namely sucralfate and 5-ASA.1,2,6,8
The main finding of this study was that APC is a safe and effective treatment modality for haemorrhagic proctitis. Female patients accounted for all but three of the patients in this series, in keeping with the high prevalence of carcinoma of the cervix requiring pelvic radiation in our setting.18 The median age at presentation in the study was 52 years, which falls within 48-70 years reported in the literature.5,16 The median duration of symptoms prior to presentation was 16.5 months which is higher than the 8-13 months reported in the literature.1,8,19 This delayed referral to the colorectal unit is most likely attributed to several factors not explored in this study that cause delayed presentation: low socioeconomic status, low levels of health education (patient being unaware of complications of radiation), inadequate referral pathways and prior ineffective formalin treatment.
Internationally, APC has become the preferred endoscopic method for first-line treatment of haemorrhagic radiation induced proctitis as it is more effective than conservative treatment, cost effective, easily available, technically easy to apply and safe.1,2,6,10
APC achieves effective haemorrhage resolution in 68.998.5% of patients.1,2,17,19,20 This series had a marginally lower complete resolution rate of 60.3%, which was thought to be due to 5.2% of the patients being lost to follow-up after the first session of APC; this was attributed to progression of primary disease, resolution of symptoms or cost associated with attending IALCH. Bansal et al. noted partial symptom resolution in 16% of patients, while in this series it was noted 32.8% of patients.2 This study revealed a median of three sessions were needed to achieved symptom resolution which is higher than the median of two sessions noted in other studies1,17 and the average of 1.3 sessions in Zhong's study of 45 patients.19
Post-APC complications, such as rectal pain, mucous discharge and rectal ulcerations, occur in 5-20% of patients and are self-limiting,1,2,6,17 while in 10% of cases significant complications, such as perforation, necrosis and stricture, were documented.2,6 In this series, major complications post-APC were noted in 3.5% of patients. Rectal mucosal ulcerations occurred in two (3.4%) patients, of which one was lost to follow-up and the other developed an RVF too large for surgical repair resulting in a diverting colostomy. Paquette et al. found severe post-APC complications - RVF and rectal stricture - in about 3% which was comparable to this series.17 In contrast, Zhong et al. reported higher rates of severe complications (13.3%) including extensive bleeding, perforation, necrosis, rectal strictures and formation of fistula compared to this series.19 Zhong et al. attributed the complication rate to proctitis-induced ulcerations greater than 1 cm2, while in this series we did not note any pre-APC rectal ulcers.19 However, it may well be that RVF and rectal strictures are attributable to ongoing radiation damage rather than APC.
Endorectal topical sucralfate application is an effective, well-tolerated medical treatment with symptom improvement in 75-92% of patients with minimal side effects.1,2,6-9,11,12,17 The use of 5-ASA is not routinely recommended as it has shown mixed results.1,2,6,9,11,16
Endoscopic options like cryoablation have been shown to improve symptoms in 70-80% of patients with endoscopic improvement in 70% of patients,2,6,11,13,20 while RFA improved symptoms in 88% of patients (15/17).20
HBOT has a role in treatment of chronic radiation proctitis.2 HBOT inhibits bacterial growth, toxin production as well as decreasing tissue hypoxia by providing higher concentration of oxygen ultimately promoting neovascularisation, re-epithelisation and collagen formation.4,6,11 Symptom improvement and resolution including bleeding has been reported in 67-89% of patients.4,6,11,12,17 HBOT is not readily available in our setting, but when available is a good option for treating radiation proctitis.
South Africa is a resource-constrained country which faces many challenges in the public healthcare system. Resources such as APC are not freely available in KZN; it is currently only available at IALCH. Endorectal instillation of 4% formalin is a safe, effective, readily available and well-tolerated alternative to APC.5 Endorectal instillation of formalin is thus the first-line interventional modality in regional hospitals that refer to IALCH. International literature reports an average of two sessions of endorectal formalin instillation to achieve improvement of symptoms.5,17,21 Studies found that 50% had resolution after the first session, 93-100% bleeding cessation, with recurrence of bleeding noted in 30% of patients.3,5,17,20 No patient returned to the unit with recurrence of symptoms, which could be biased by a short follow-up duration as well patients returning to their regional hospitals with symptoms and being managed at that level and not referred to IALCH. Multicentre centre studies need to be undertaken to compare efficacy with international literature and to compare with APC. Complications are described as infrequent and include rectal pain, incontinence, rectal ulceration and rectal strictures.17,21,22
Formalin instillation is still widely used in the South African setting, but more studies on APC and formalin painting need to be done to determine if these modalities are comparable in our setting.
Radiation injury results in fibrosis, fixation of tissues and poor vascularity caused by microvascular damage resulting in poor and/or delayed wound healing in patients undergoing surgery management.9,23,24 In the series it was noted that seven (21%) patients had rectal strictures which were non obstructing and two (3.4%) had some degree of rectal scarring/fibrosis, none of which required surgical intervention.
Surgical management represents the most invasive mode of treatment in radiation proctitis.1,6,8 Surgical options should be considered the last option and reserved for patients with symptoms refractory to medical as well as endoscopic management.1,2,6,8-11 Common surgical options used include faecal diversion and proctectomy.1,6,9-11 Surgical management is required in less than 10% of patients with radiation proctitis and is necessitated by brisk haemorrhage, perforation, obstructing stricture or fistula.1,6,9-11
The only patient who presented with an RVF and haemorrhagic proctitis in this series was treated conservatively with a diverting colostomy as the fistula was too large to manage surgically and the haemorrhage was treated with APC.
The major limitation of this single tertiary centre study is that frequency of and the modes of treatment of radiation proctitis presenting to regional hospitals is not known. Hence, we do not know if this tertiary referral cohort accurately reflects the true spectrum of disease or its treatment. An additional limitation is only a short duration of follow-up. Follow-up of at least 12 months from the last APC session would have been ideal.19 The limited published data with relation to the use of APC in South Africa limits the ability to compare our results.
Conclusion
Despite these limitations, the study attests to the safety and short-term efficacy of standardised APC administration within a dedicated tertiary hospital surgical team to treat haemorrhagic radiation proctitis with results that are comparable with those in literature. Future studies should address the paucity of data from regional hospitals and the assessment of the efficacy of alternate treatments, particularly formalin instillation.
Acknowledgements
This manuscript would not have been possible without the tireless efforts and guidance of Professor TE Madiba who sadly passed away during the writing of this manuscript.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Ethical approval for the conduct of the study was obtained from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (Protocol number BE356/19).
ORCID
MI Jali https://orcid.org/0000-0002-2889-2747
Y Moodley https://orcid.org/0000-0002-4119-1734
S Kader https://orcid.org/0000-0002-6216-5703
S Cheddie https://orcid.org/0000-0002-1844-5759
REFERENCES
1. Weiner JP, Wong AT, Schwartz D, et al. Endoscopic and non-endoscopic approaches for the management of radiation-induced rectal bleeding. World J Gastroenterol. 2016;22(31):6972-86. https://doi.org/10.3748/wjg.v22.i31.6972. [ Links ]
2. Bansal N, Soni A, Kaur P, Chauhan AK, Kaushal V. Exploring the management of radiation proctitis in current clinical practice. J Clin Diagn Res. 2016;10(6):XE1-XE6. https://doi.org/10.7860/JCDR/2016/17524.7906. [ Links ]
3. Ashburn JH, Kalady MF. Radiation-induced problems in colorectal surgery. Clin Colon Rectal Surg. 2016;29(2):85-91. https://doi.org/10.1055/s-0036-1580632. [ Links ]
4. Trzcinski R, Mik M, Dziki L, Dziki A. Radiation proctitis. In: Cianci P, editor. Proctological Diseases in Surgical Practice [Internet]. London: IntechOpen; 2018. https://doi.org/10.5772/intechopen.76200. [ Links ]
5. Dziki L, Kujawski R, Mik M, et al. Formalin therapy for haemorrhagic radiation proctitis. Pharmacol Rep. 2015;67(5):896-900. https://doi.org/10.1016/j.pharep.2015.03.006. [ Links ]
6. Tabaja L, Sidani SM. Management of radiation proctitis. Dig Dis Sci. 2018;63(9):2180-8. https://doi.org/10.1007/s10620-018-5163-8. [ Links ]
7. Vanneste BGL, Van De Voorde L, De Ridder RJ, et al. Chronic radiation proctitis: tricks to prevent and treat. Int J Colorectal Dis. 2015;30(10):1293-303. https://doi.org/10.1007/s00384-015-2289-4. [ Links ]
8. Dipankar R. Chronic radiation proctitis- a common but difficult problem. J Evid Based Med Healthc. 2019;6(31):2121-5. https://doi.org/10.18410/jebmh/2019/432. [ Links ]
9. Do NL, Nagle D, Poylin VY. Radiation proctitis: current strategies in management. Gastroenterol Res Pract. 2011;(2011):1-9. https://doi.org/10.1155/2011/917941. [ Links ]
10. Tagkalidis PP, Tjandra JJ. Chronic radiation proctitis. ANZ J Surg. 2001;71(4):230-7. https://doi.org/10.1046/j.1440-1622.2001.02081.x. [ Links ]
11. Grodsky MB, Sidani SM. Radiation proctopathy. Clin Colon Rectal Surg. 2015;28(2):103-11. https://doi.org/10.1055/s-0035-1547337. [ Links ]
12. Leiper K, Morris A. Treatment of radiation proctitis. Clin Oncol. 2007;19(9):724-9. https://doi.org/10.1016/j.clon.2007.07.008. [ Links ]
13. Rustagi T, Mashimo H. Endoscopic management of chronic radiation proctitis. World J Gastroenterol 2011;17(41):4554-62. https://doi.org/10.3748/wjg.v17.i41.4554. [ Links ]
14. Stats SA. Census 2011 statistical release. Statistics South Africa, Pretoria, South Africa; 2012. Available from: https://www.statssa.gov.za/publications/P03014/P030142011.pdf. [ Links ]
15. Madiba T, Moodley Y, Sartorius B, et al. Clinicopathological spectrum of colorectal cancer among the population of the KwaZulu-Natal Province in South Africa. Pan Afr Med J. 2020;37:74. [ Links ]
16. Wu C, Guan L, Yao L, Huang J. Mesalazine suppository for the treatment of refractory ulcerative chronic radiation proctitis. Exp Ther Med. 2018;16(3):2319-24. https://doi.org/10.3892/etm.2018.6464. [ Links ]
17. Paquette IM, Vogel JD, Abbas MA, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the treatment of chronic radiation proctitis. Dis Colon Rectum. 2018;61(10):1135-40. https://doi.org/10.1097/DCR.0000000000001209. [ Links ]
18. Jordaan S, Michelow P, Richter K, Simoens C, Bogers J. A review of cervical cancer in South Africa: previous, current and future. Health Care Curr Rev. 2016;4(4):1-6. https://doi.org/10.4172/2375-4273.1000180. [ Links ]
19. Zhong QH, Liu ZZ, Yuan ZX, et al. Efficacy and complications of argon plasma coagulation for hemorrhagic chronic radiation proctitis. World J Gastroenterol. 2019;25(13):1618-27. https://doi.org/10.3748/wjg.v25.i13.1618. [ Links ]
20. Lee JK, Agrawal D, Thosani N, et al. ASGE guideline on the role of endoscopy for bleeding from chronic radiation proctopathy. Gastrointest Endosc. 2019;90(2):171-82. https://doi.org/10.1016/j.gie.2019.04.234. [ Links ]
21. Tjandra JJ, Sengupta S. Argon plasma coagulation is an effective treatment for refractory hemorrhagic radiation proctitis. Dis Colon Rectum. 2001;44(12):1759-65. https://doi.org/10.1007/BF02234451. [ Links ]
22. Tsujinaka S, Baig MK, Gornev R, et al. Formalin instillation for hemorrhagic radiation proctitis. Surg Innov. 2005;12(2):123-8. https://doi.org/10.1177/155335060501200209. [ Links ]
23. Vogel JD, Johnson EK, Morris AM, et al. Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Dis Colon Rectum. 2016;59(12):1117-33. https://doi.org/10.1097/DCR.0000000000000733. [ Links ]
24. Zelga P, Tchórzewski M, Zelga M, Sobotkowski J, Dziki A. Radiation-induced rectovaginal fistulas in locally advanced gynaecological malignancies - new patients, old problem? Langenbeck's Arch Surg. 2017;402(7):1079-88. https://doi.org/10.1007/s00423-016-1539-4. [ Links ]
 Correspondence:
Correspondence:
MI Jali
Email: dr.markjali@gmail.com














