Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.1 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3296
PAEDIATRIC SURGERY
The profile and outcome of small bowel atresia at Universitas Academic Hospital
H du Preez; E Brits
Department of Surgery, School of Clinical Medicine, Faculty of Health Sciences, University of the Free State, South Africa
ABSTRACT
BACKGROUND: In patients with intestinal atresia, associated congenital anomalies and prematurity are the main predictors of mortality in high-income countries (HIC). In low-and middle-income countries (LMIC), late referrals and lack of resources contribute to mortality. This study aims to describe the outcome of small bowel atresia at a tertiary institution in a LMIC
METHODS: A retrospective descriptive and analytical study was done on all neonates admitted with small bowel atresia from 1 January 2010 to 31 October 2016. Birth demographics, status on arrival, atresia type, surgical interventions and clinical course were analysed in relation to outcomes including mortality
RESULTS: The study included 92 patients. Thirty-three patients had duodenal atresia and 59 jejunal atresia. Median gestation was 34 weeks, with average birth weight 2.2 kg. Seven were diagnosed antenatally and 13 (14.1%) were born in a tertiary institution. A cardiac congenital anomaly was present in 43.5%. Late referrals comprised 72.8%. Sixty per cent were dehydrated and 55.4% were septic on arrival. The median age at surgery was 7.5 days after being admitted, for a median of 2 days. The median age reaching full feeds was 18 days, and 28.6% had a feeding intolerance. The median number of septic episodes were two and the median length of stay 28 days. Of the 92 patients, 8.7% were palliated and 10.9% died. Mortality was strongly associated with prematurity and sepsis with hospital stay
CONCLUSION: Despite late referrals, our mortality was comparable to HICs. We overcame this burden due to access to resources, sophisticated equipment and a low surgical complication rate. The length of stay could be decreased with a feeding protocol and discharge goals
Keywords: small bowel atresia, profile, outcome, low- and middle-income countries
Introduction
Intestinal atresia can be defined as a congenital absence of what should be a patent lumen, resulting in either a complete obstruction or a stenosis. The worldwide incidence of intestinal atresia ranges between 2.5 and 3 per 10 000 live births. Associated anomalies are not uncommon and occur in up to 50% in those with duodenal atresia. This includes growth retardation, prematurity and cardiac lesions. The frequency of associated congenital anomalies is less in those with jejunal and ileal atresia.14
Major advances in neonatal intensive care and neonatal surgery has led to the mortality of infants with intestinal atresia decreasing from 50% in the 1950s to between 5-10% currently.5 However, due to under-resourced health systems, mortality in low- and middle-income countries (LMICs) remains as high as 30%.5,6
Factors influencing mortality vary between high-income countries (HICs) and LMICs. In HICs, the strongest predictors of mortality are prematurity, associated congenital abnormalities and low birth weight.5,7 In LMICs, late presentation, lack of resources such as parenteral nutrition, lack of trained staff, high sepsis rates and dehydration also influence mortality.8
South Africa is an LMIC which has an under-resourced state healthcare system that provides services for 80% of the population. Neonatal care is centralised in the urban areas with poor infrastructure in the smaller cities and rural areas that are unfavourable for advanced care of surgical neonates. This study aimed to determine, in a tertiary care hospital with specialised services for neonatal surgery, the effect of status on arrival and clinical course on the outcome of neonates admitted for treatment of small bowel atresia, and to compare to those of other LMICs and HICs.
Methods
A retrospective descriptive study design that included all patients admitted with small bowel atresia to Universitas Academic Hospital (UAH) from 1 January 2010 to 31 October 2016 was done. UAH is a tertiary centre in Bloemfontein and located in central South Africa. The hospital is the only paediatric surgery referral centre for the Free State Province, Northern Cape Province, parts of the Eastern Cape Province and the neighbouring country Lesotho. The hospital serves a population of 6.1 million people from a large geographical area. Neonatal transfers have many logistic factors, including travel time of up to 12 hours. The two paediatric surgeons employed at UAH see approximately 20 cases of small bowel atresia per year. The hospital has a neonatal intensive care unit with ventilatory facilities and parenteral nutrition available.
The names of patients with small bowel atresia were obtained from the paediatric surgical statistical records. Patient information was extracted from patient notes on the MediTech© system and the hospital files. Information regarding birth history, status on arrival with regards to hydration, sepsis and age, in hospital management with regards to age at surgery, surgical management, time to full feeds, and outcomes were recorded on a data sheet by the researchers. The diagnosis of small bowel atresia should be made within 24 to 48 hours of life, so we defined a late referral as an arrival later than day two of life. We defined sepsis as having clinical or biochemical signs of sepsis.
Data were captured and analysis was done by the Department of Biostatistics, Faculty of Health Sciences, University of the Free State. The results were summarised by frequencies and percentages (categorical variables), means and standard deviations (SD) or percentiles (numerical variables). Comparisons between groups were done using contingency tables with chi-squared or Fisher's exact tests as appropriate. A level of significance was accepted as a two-tailed p-value < 0.05.
Approval was obtained from the Health Sciences Research Ethics Committee of the UFS, Free State Department of Health, and relevant department heads. To ensure patient confidentiality, no identifying detail was captured on the data sheets.
Results
In total, 92 patients were included in the study. Patients were almost evenly distributed along gender (Table I). Their median birth weight was 2.2 kg (SD 0.6 kg; range 980 g-3.6 kg) with an average gestation of 35 weeks (SD 3.7 weeks; range 24-42 weeks). Only 7.6% of the patients were diagnosed antenatally. While 55.4% of the patients were born in the low birth-weight category, the weight for age was deemed appropriate for 60.7%.
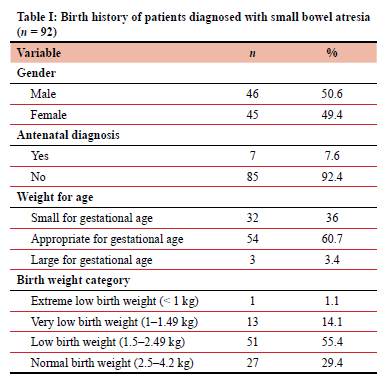
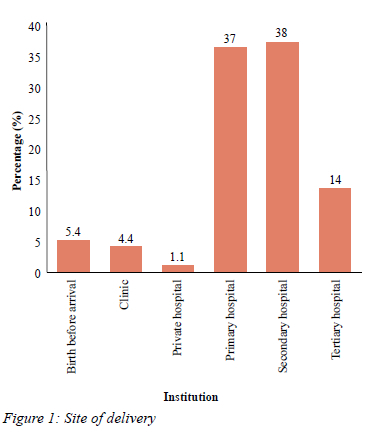
The majority of the patients were born in the Free State (69.6%), followed by the Northern Cape (26.1%) and Lesotho (4.4%). Figure 1 shows the institution at which delivery occurred. The low percentage of tertiary deliveries was due to only seven of the 92 patients being diagnosed antenatally.
Twenty-three of the patients were HIV exposed of which 19 had a negative birth polymerase chain reaction (PCR) test result. PCR test results were not available for the other four patients.
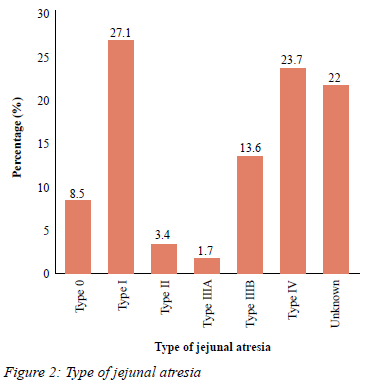
Thirty-three of the 92 patients were diagnosed with duodenal atresia. Specific type was not documented in the patient files. Jejunal atresia types were recorded according to the Grosfeld classification9 (Figure 2).
The most common associated congenital abnormality was a cardiac lesion (43.5%). Five (5.5%) had trisomy 21 and all were diagnosed with duodenal atresia. Sixteen patients (17.4%) had malrotation. The patients with malrotation were equally distributed among duodenal atresia and jejunal atresia. Other associated congenital abnormalities were oesophageal atresias (5.4%) and anorectal malformations (4%), that all occurred in patients with duodenal atresia.
Other anomalies that were encountered were colonic atresia and annular pancreas (3 each) and one each of a Meckels diverticulum, situs inversus, gastric duplication, Dandy Walker malformation, hypospadias and foetal alcohol syndrome.
The patients arrived at a median of 4 days after birth (range 1-46). Sixty-seven (72.8%) arrived later than day 2 after birth. All of the late arrivals were due to a delay in the diagnosis. Fourteen babies had multiple reasons for late arrivals in addition to delayed diagnosis, which included: transport delays (n = 9), obtaining a passport (n = 4) and no intensive care bed available (n = 1).
Fifty-six (60.9%) had signs of dehydration and 44 (52.2%) had abnormal electrolytes. Comparing the effect of late referrals on hydration, it was found that there was a strong association between late referrals and dehydration, with a p-value of 0.0005. Fifty-one (55.4%) patients were suspected of having sepsis or had raised infective markers on admission and all were started on antibiotics.
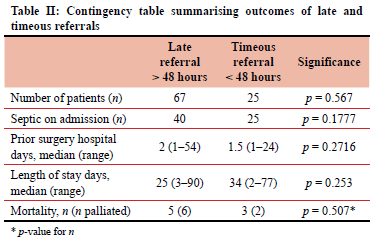
Comparison with regards to number of septic episodes, time admitted prior to surgery, length of stay and mortality, showed no statistical significance between the groups.
Although 40 of the septic patients were late referrals, there was no significant association between late referrals and sepsis on admission (p = 0.18). The patients' age at arrival had no statistically significant effect on mortality (p = 0.57). If the patients were referred late, their age at surgery was older (p < 0.0001). The patients stayed in hospital for a median of 28 days (range 2-90 days). However, the age at surgery had no significant effect on length of stay (p = 0.14). In the group that was referred late, patients were operated on a median of 2 days after admission (range 1-54 days). There was no statistical association between being referred late and length of time admitted prior to surgery (p = 0.27) (Table II).
The median age at the time of their first surgery was 7.5 days (range 1-73 days), after being admitted for a median number of 2 days (range 1-54 days). A primary repair was done in 81 of the 92 patients. The patients with duodenal atresia received a Kimura diamond-shaped anastomosis, and the patients with jejunal atresia had a tapered, end-end anastomosis. Due to the presence of other anomalies, such as oesophageal atresia, colonic atresia, and distal bowel perforation, six of the patients had a different approach during their index surgery. Three patients were palliated: one was due to cardiac arrest in theatre and two for having insufficient residual bowel for survival. The 16 patients with malrotation received a modified Ladd's procedure.
Two patients had anastomotic leaks: one had sealed off and the other patient had overt contamination from an anastomotic leak. Four patients developed short bowel syndrome and three patients developed wound sepsis. In addition to the two patients with anastomotic leaks, one patient was re-operated for a later bowel perforation and three for anastomotic strictures.
Feeding intolerance was present in 26 (28.6%) patients. The median days to full feeding was 18 days (range 7-88 days), with the median number of days on intravenous nutritional support at 11 days range. Parenteral nutrition-associated liver disease hepatitis developed in 15 (16.3%) patients.
The duodenal atresia group took a median of 19 days (range 9-88 days) to reach full feeds. They were more prone to develop a feeding intolerance and took longer to reach full feeds (p = 0.05). The jejunal atresia group took a median number of 17 days to reach full feeds (range 7-55 days). There was no association between the number of septic episodes and the time to full feeds (p = 0.39), and age at surgery to time to full feeds (p = 0.10).
Sepsis occurred in 84 patients in this study. The median number of septic episodes per patient during their hospital stay was 2 (range 1-8 episodes). There was no association between the children who were HIV exposed and the number of septic episodes (p = 0.74). The most common organisms cultured were Candida and gram-negative species. There was a strong positive association between the number of septic episodes and length of stay (p < 0.0001).
The median length of stay in hospital was 28 days for both duodenal and jejunal atresia patients. Eighteen (19.6%) of the 92 patients included in this study died. Eight of the 18 patients were palliated due to: short bowel syndrome (2), liver failure as a result of long-term TPN (1), sepsis (2), and multi-organ failure (5). The number of septic episodes had no significant influence on mortality (p = 0.76). The presence of associated congenital abnormalities had no effect on mortality. Gestation had an effect on mortality, as prematurity was associated with mortality (p = 0.045).
Discussion
Only seven of the 92 patients were diagnosed with small bowel atresia antenatally. Small bowel atresia can be diagnosed antenatally with great accuracy. Studies from the UK have shown that intestinal atresia can be diagnosed antenatally between 75-100% of the time.7
Authors report variable results depending on gestational age and operator experience.7,10
Much of the morbidity and cost in treating a patient is due to late presentation and subsequent sequalae of inadequate management in peripheral hospitals. Patients diagnosed antenatally arrive up to 4 days earlier.11 One can argue that there is an immense benefit in adequate parental counselling and pre-delivery planning as well as eliminating waiting times for transport.
The outcomes of surgery in HIV-positive patients are well documented and suggest an increased morbidity and complication rate by almost 12 times.12,13 Even when infants are simply HIV exposed, they will have an impaired passive immunity. Infants awaiting surgery for repair of their atresia are kept nil per mouth. Thus, they will not benefit from the protective antibodies found in breastmilk. This, alongside an immature immune system, will increase their susceptibility to neonatal sepsis and postoperative complications. No statistically significant association between HIV exposure and the number of septic episodes postoperatively was found. This can be due to a small sample size of our HIV-exposed patients as well as the ubiquitous nature in the diagnosis of neonatal sepsis.
As a group, cardiac lesions were the most common general associated congenital anomaly found, which is in line with international literature.2,3
Duodenal atresia occurs due to defects in foregut canalisation and is more associated with other congenital anomalies.11 Trisomy 21 occurs in up to 30% of patients with duodenal atresia, which is in line with our results since all the children diagnosed with trisomy 21 had duodenal atresia and 15.2% of those with duodenal atresia had trisomy 21. It can also be linked with VACTERL association, therefore as expected, all patients with either an anorectal malformation or oesophageal atresia occurred in the group with duodenal atresia.
In comparison, jejunal atresia occurs later in gestation and is a result of an isolated vascular event, which causes ischaemia of the adjacent bowel and therefore less associated congenital abnormalities are found.1,9
Delay in presentation, long waiting times in peripheral hospitals and delays in transport, all contribute to late referrals in LMICs. Studies from Nepal, India and China confirm this pattern of late referrals, with patients presenting on average on day 3 or even day 7 (range 1-28 days) of life. Late presentation may attribute to mortality rates of up to 28.5%.8,11,14-16
Bilious vomiting and failure to pass normal meconium are common clinical signs in intestinal atresia. Furthermore, bilious vomiting in an infant necessitates an emergency referral to a paediatric surgeon. Even though it was not statistically analysed in our study, it was found that almost all of the study subjects vomited bile-stained fluid; sometimes for many days, prior to presenting to our institution. Missing this common sign, along with a lack of resources, further delays the diagnosis and referral process.
By the time infants present at our institution, they are dehydrated and many of them septic. This can be attributed to continued vomiting and a delay in initiating the correct treatment, such as intravenous fluid resuscitation and recognising sepsis. Dehydration and acid-base disturbances (29.6%) and renal impairment (5%) on arrival have been shown in other studies from LMICs.11
Three of the six relook operations done were for anastomotic strictures. Anastomotic leaks after surgery for small bowel atresia are rare. If they occur, the consequence can be devastating. The rate of anastomotic leaks in our study is (2%) compared with literature in HICs (2%).14,17
After surgery for small bowel atresia, an ileus is expected. Infants should reach full feeds, on average, 21 days postoperatively for both jejunal and duodenal atresia.18,19 Feeding intolerance has been shown to increase morbidity and mortality as well as length of stay.20,21 Prolonged parenteral nutrition exposes an infant to develop TPN hepatitis and central line-associated sepsis. This can be prevented by starting SMOF-lipid TPN when it is expected that the patient might require TPN for more than 2 weeks.
Sepsis and septic episodes will also delay the progression of feeds.
Neonatal sepsis increases the mortality of premature and lower birth weight infants. Due to the low yield of a positive blood culture to diagnose neonatal sepsis, the present practise is to treat a septic episode not only based on a positive blood culture but on clinical suspicion. Clinical sepsis alone has an increased mortality that could not be explained by any other morbidities other than infection.22 Coagulase-negative staphylococcus is a common pathogen, specifically in the presence of central lines. This is followed by gram-negative organisms. There is a growing concern regarding the increasing incidence of fungal sepsis. This can be seen in this study as well, as the most general organism cultured was Candida.
With regards to small bowel atresia and sepsis, in LMICs, sepsis contributed to the postoperative mortality. This is not seen in HICs.
Our length of stay was considerably longer compared to other institutions. Studies from India and China reported a length of stay between 11 and 17 days, respectively.11,14
It often happens that patients wait for transport out of our institution, and we do not have adequate down referral centres to discharge patients in order to achieve full enteral feeds or to complete current treatment.
There is a marked difference in mortality between HICs (10-15% due to prematurity and other congenital anomalies) and LMICs (30% due to lack of infrastructure, skilled personnel, surgical complications, sepsis, prematurity) in patients with small bowel atresia.11,14,17
It is important to consider that we lack resources to care for children with short bowel syndrome. Therefore, our mortality rate is higher, as we had to palliate infants who were clinically at risk of developing short bowel syndrome. In our study, we found that only prematurity was strongly associated with mortality. This is in keeping with literature from HICs.5 We suspected that the massive burden of late referrals would influence our mortality, but this was not the case. We believe that access to well-trained personnel, nutritional support, critical care support and a low surgical complication rate are the reasons for our low mortality in the face of late referrals
Conclusion
Improved education of healthcare workers with regards to danger signs, such as bilious vomiting, as well as improving antenatal care and screening programmes should counteract late referrals and their consequences. A clear protocol on initiation and advancement of feeds, discharge goals and adequate down referral centres could decrease the length of stay and costs associated with it. Further improvements in our infrastructure such as central line teams, neonatal SMOF-lipid TPN bags, and a multidisciplinary team to care for short bowel syndrome patients could also improve our morbidity and mortality.
Acknowledgements
The authors thank Mr C van Rooyen, Faculty of Health Sciences, Department of Biostatistics, University of the Free State, for the help and guidance with the statistical analysis of the data, and Ms T Mulder, Faculty of Health Sciences, University of the Free State, for technical and editorial preparation of the manuscript.
Conflict of interest
The authors declare no conflict of interest.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Ethical permission was obtained from the University of the Free State (HSREC 184/2016) and the Free State Department of Health (FS2017RP22928).
ORCID
H du Preez https://orcid.org/0000-0002-7787-7324
E Brits https://orcid.org/0000-0002-6422-9272
REFERENCES
1. Robb A, Lander A. Duodenal and small intestinal atresias and stenosis. Surgery. 2007;25(7):287-90. https://doi.org/10.1016/j.mpsur.2007.05.013. [ Links ]
2. Walker K, Badawi N, Hamid CH, et al. A population-based study of the outcome after small bowel atresia/stenosis in New South Wales and the Australian Capital Territory, Australia, 1992-2003. J Pediatr Surg. 2008;43(3):484-8. https://doi.org/10.1016/j.jpedsurg.2007.10.028. [ Links ]
3. Frischer JS, Azizkhan RG. Jejunoileal atresia and stenosis. In: Coran AG, Caldamone A, Adzick NS, Krummel TM, Laberge J-M, Shamberger R, editors. Pediatric Surgery. 7th ed. Philadelphia: Elsevier Saunders; 2012. p. 1059-71. https://doi.org/10.1016/B978-0-323-07255-7.00082-9. [ Links ]
4. Applebaum H, Sydorak R. Duodenal atresia and stenosis-annular pancreas. In: Coran AG, Caldamone A, Adzick NS, Krummel TM, Laberge J-M, Shamberger R, eds. Pediatric Surgery. 7th ed. Philadelphia: Elsevier Saunders; 2012. p. 1059-71. https://doi.org/10.1016/B978-0-323-07255-7.00081-7. [ Links ]
5. Piper HG, Alesbury J, Waterford SD, Zurakowski D, Jaksic T. Intestinal atresias: factors affecting clinical outcomes. J Pediatr Surg. 2008;43(7):1244-8. https://doi.org/10.1016/j.jpedsurg.2007.09.053. [ Links ]
6. Chirdan LB, Uba AF, Pam SD. Intestinal atresia: management problems in a developing country. Pediatr Surg Int. 2004;20(11-12):834-7. https://doi.org/10.1007/s00383-004-1152-4. [ Links ]
7. Wax JR, Hamilton T, CartinA, et al. Congenitaljejunal and ileal atresia: natural prenatal sonographic history and association with neonatal outcome. J Ultrasound Med. 2006;25(3):337-42. https://doi.org/10.7863/jum.2006.25.3.337. [ Links ]
8. Shakya VC, Agrawal CS, Shrestha P, et al. Management of jejunoileal atresias: an experience at eastern Nepal. BMC Surg. 2010;10:35. https://doi.org/10.1186/1471-2482-10-35. [ Links ]
9. Grosfeld JL, Ballantine TV, Shoemaker R. Operative management of intestinal atresia and stenosis based on pathologic findings. J Ped Surg. 1979;14(3):368-75. https://doi.org/10.1016/S0022-3468(79)80502-3. [ Links ]
10. Virgone C, D'antonio F, Khalil A, et al. Accuracy of prenatal ultrasound in detecting jejunal and ileal atresia: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2015;45(5):523-9. https://doi.org/10.1002/uog.14651. [ Links ]
11. Chen Q, Gao Z, Tou J, et al. Congenital duodenal obstruction in neonates: a decade's experience from one centre. World J Pediatr. 2014;10(3):238-44. https://doi.org/10.1007/s12519-014-0499-4. [ Links ]
12. Karpelowsky JS, Millar AJ, Van der Graaf N, Van Bogerijen G, Zar HJ. Outcome of HIV-exposed uninfected children undergoing surgery. BMC Pediatr. 2011;11:69. https://doi.org/10.1186/1471-2431-11-69. [ Links ]
13. Karpelowsky JS, Millar AJ, Van der Graaf N, Van Bogerijen G, Zar HJ. Comparison of in-hospital morbidity and mortality in HIV-infected and uninfected children after surgery. Pediatr Surg Int. 2012;28(10):1007-14. https://doi.org/10.1007/s00383-012-3163-x. [ Links ]
14. Gupta S, Gupta R, Ghosh S, et al. Intestinal atresia:experience at a busy centre of North-West India. J Neonatal Surg. 2016;5(4):51. https://doi.org/10.21699/jns.v5i4.405. [ Links ]
15. Verma A, Rattan KN, Yadav R. Neonatal intestinal obstruction: a 15-year experience in a tertiary care hospital. J Clin Diagn Res. 2016;10(2):SC10-SC13. https://doi.org/10.7860/JCDR/2016/17204.7268. [ Links ]
16. Abdalla AR, Hussien S, Karsani A. Pattern of neonatal surgical presentation and outcome in Sinnar Hospital (20132014). Glob J Med Res. 2014;14(4-1). [ Links ]
17. Singh V, Pathak M. Congenital neonatal intestinal obstruction: retrospective analysis at tertiary care hospital. J Neonatal Surg. 2016;5(4):49. https://doi.org/10.21699/jns.v5i4.393. [ Links ]
18. Yang C, Liu Z, Tian M, et al. Relationship between serum albumin levels and infections in newborn late preterm infants. Med Sci Monit. 2016;22:92-98. https://doi.org/10.12659/MSM.895435. [ Links ]
19. Erickson T, Vana PG, Blanco BA, et al. Impact of hospital transfer on surgical outcomes of intestinal atresia. Am J Surg. 2017;213(3):516-20. https://doi.org/10.1016/j.amjsurg.2016.11.009. [ Links ]
20. Blaser AR, Starkopf L, Deane AM, Poeze M, Starkopf J. Comparison of different definitions of feeding intolerance: a retrospective observational study. Clin Nutr. 2015;34(5):956-61. https://doi.org/10.1016/j.clnu.2014.10.006. [ Links ]
21. Moore TA, Wilson ME. Feeding intolerance: a concept analysis. Adv Neonatal Care. 2011;11(3):149-54. https://doi.org/10.1097/ANC.0b013e31821ba28e. [ Links ]
22. De Souza Rugolo LM, Bentlin MR, Mussi-Pinhata M, et al. Late-onset sepsis in very low birth weight infants: a Brazilian Neonatal Research Network Study. J Trop Pediatr. 2014;60(6):415-21. https://doi.org/10.1093/tropej/fmu038. [ Links ]
 Correspondence:
Correspondence:
H du Preez
Email: dupreez.hilge@gmail.com














