Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.1 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3696
PAEDIATRIC TRAUMA
High-grade renal trauma in children and adolescents can be successfully managed non-operatively
V ThirayanI; VY KongII, III, IV; A ElsabaghV; W XuVI; N RajaretnamVII; B ConradieVI; C CheungVIII; DL ClarkeIII; JL BruceIV; GL LaingIV; V ManchevIV; W BekkerIV
IDepartment of Surgery, Waikato Hospital, New Zealand
IIDepartment of Surgery, Auckland City Hospital, New Zealand
IIIDepartment of Surgery, University of the Witwatersrand, South Africa
IVDepartment of Surgery, University of KwaZulu-Natal, South Africa
VDepartment of Surgery, St John of God Midland Public Hospital, Australia
VIDepartment of Surgery, University of Auckland, New Zealand
VIIDepartment of Surgery, St James's Hospital, Ireland
VIIIDepartment of Surgery, Chris Hani Baragwanath Academic Hospital, South Africa
ABSTRACT
BACKGROUND: This paper reviews our experience with management of renal injuries in children and adolescents with a focus on the outcome of non-operative management (NOM
METHODS: Retrospective review of the clinical characteristics, injury grade (I-III, low grade and IV and V high grade), management and outcomes of children < 18 years old with renal trauma presenting to a major trauma centre in South Africa between December 2012 and October 2020
RESULTS: Sixty-one children with a renal injury were identified with a median age of 13 (range 0-18) years. Forty-five were boys; blunt and penetrating mechanisms of trauma were sustained by 55 (90%) and six (10%) children, respectively. The median American Association for the Surgery of Trauma (AAST) grade of renal injury was 3 (range 1-5): this included eight (13%) with grade I, six (10%) with grade II, 17 (28%) with grade III, 20 (46%) with grade IV and 10 (16%) with grade V injuries. Forty children (66%) were successfully managed non-operatively and 21 required a laparotomy; of these six (28%) required nephrectomy. The overall renal salvage rate was 55/61 (90%). Children who required laparotomy were significantly more likely to have sustained a penetrating mechanism of injury (24% vs 2%) and have greater length of hospital stay (median 9 vs 3 days) compared to children managed non-operatively (p < 0.05). Children who underwent a nephrectomy had a significantly greater length of hospital stay (median 9 vs 4 days, p = 0.03); however, their demographics, outcomes and complications were otherwise not different. Twenty-four (39%) children developed complications. Two children (3%) died; one managed non-operatively and one with a laparotomy
CONCLUSION: Paediatric renal trauma can be successfully managed non-operatively in over two-thirds of cases in this middle-income country. High grade of renal injury does not absolutely predict need for surgery or nephrectomy and can be managed non-operatively
Keywords: paediatric, trauma, abdominal injury, non-operative management
Introduction
There has been a radical change in the management of intra-abdominal solid organ injury in children over the last fifty years, from an operative approach to a non-operative management (NOM) strategy.1,2 This transition has been supported by ongoing improvements in imaging, as well as by advances in interventional radiology and critical care.1-3 The application of NOM to low-grade renal trauma in children is now routine, and increasingly NOM is applied to high-grade injuries.4,5 However there is still a lack of consensus in children regarding renal salvage in higher grades of renal injury.4-12 Increasingly, contemporary reports suggest that NOM of high-grade renal injury in children is both feasible and desirable.4-12 In light of the above discussion, this audit reviewed a single unit's experience with paediatric renal trauma over an eight-year period. It sought to review our management of renal trauma, in the paediatric and adolescent age group, to ascertain the success of NOM in high-grade injury in our setting.
Methods
Grey's Hospital is a tertiary hospital located in Pietermaritzburg, the capital of KwaZulu-Natal (KZN) province, South Africa. The Pietermaritzburg Metropolitan Trauma Service (PMTS) maintains a prospectively entered surgical registry known as the Hybrid Electronic Medical Registry (HEMR).
The approach to the management of renal trauma by the PMTS in adults has been previously reported.13 The approach to renal trauma in children is similar. Children with blunt abdominal trauma are resuscitated and monitored. Those who do not stabilise haemodynamically are expedited to the operating room. Stable children are assessed with an abdominal computed tomography (CT) scan and any renal injury is identified and graded according to the American Association for the Surgery of Trauma (AAST) renal injury scale I-V (low grade is I-III and high grade is IV-V). Provided the child remains stable, he or she is treated non-operatively. The grade of the injury is not routinely an indication for operation. Children with penetrating abdominal trauma are managed according to a selective approach. Those who have peritonitis or are haemodynamically unstable go promptly to the operating room. Children who do not meet our indications for laparotomy are admitted for observation and are selectively imaged. At laparotomy, peri-renal haematomas are explored on a selective basis, depending on whether the haematoma is expanding or actively bleeding. If a peri-renal haematoma is opened, attempts may be made to repair and salvage the kidney if the patient is stable. If the injury is high grade and if the patient's physiology is compromised, then nephrectomy is the default procedure. Paediatric renal trauma is managed by the adult trauma surgeons of the PMTS. Complex injuries are managed in conjunction with the urology department.
All children under 18 years of age who were admitted to our centre following trauma between December 2012 and October 2020 were identified from the HEMR. Those who sustained renal trauma were retrieved. Patient demographics, duration of time from injury to admission, mechanism of injury, admission vital signs, clinical laboratory data, injury severity score (ISS), Glasgow coma scale (GCS), management strategy (laparotomy vs NOM), complications, hospital length of stay and survival were analysed. Operative management was defined as immediate laparotomy.
Statistical analysis
All relevant data were extracted and initially summarised onto an Excel spreadsheet for review. Normality of data was assessed via the Shapiro-Wilk test. All statistical analysis was performed using R (version 4.0.2; R Foundation for Statistical Computing, Vienna, Austria). All normally distributed continuous variables were described using means with standard deviation (SD). Continuous variables with non-normal distribution were reported using a median with range. Independent samples t-test was used to compare normally distributed continuous variables and Mann-Whitney U test for non-normally distributed continuous variables. Chi-squared test was used to compare categorical variables with the Fisher's exact test used when one group had < 5 events. Statistical significance is achieved when p < 0.05.
Results
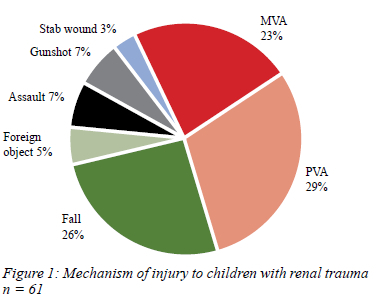
Between December 2012 and October 2020, 406 children were admitted with abdominal trauma, of which 61 (15%) sustained a renal injury with a median age of 13 (range 0-18) years old. Forty-five (74%) were boys. A mean of 7.5 (± 4.14) traumatic renal injuries occurred per year. Blunt and penetrating mechanisms of trauma were sustained by 55 (90%) and six (10%) children, respectively. Figure 1 summarises the mechanisms of injury. Figure 2 shows a trend for older children to be more frequently involved in motor vehicle accidents (MVA) or to sustain stab wounds and gunshot wounds when compared to younger children who were more frequently involved in pedestrian-vehicle accidents (PVA) and falls.
AAST grade of kidney injury
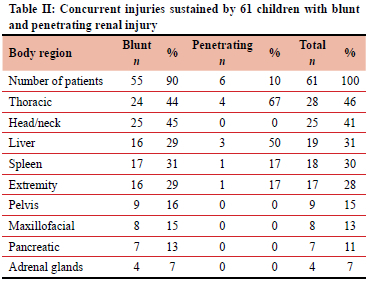
AAST grading was determined via CT scan in fifty (82%) children, and intraoperatively in the remainder. The median AAST grade of renal injury was III (range 1-5) - this included eight (13%) with grade I, six (10%) with grade II, 17 (28%) with grade III, 20 (46%) with grade IV and 10 (16%) with grade V injuries. Children with a low-grade renal injury compared to those with a high-grade renal injury had no statistically significant difference in age, sex, time to admission, mechanism, shock index (SI), revised trauma score (RTS), ISS, management, outcome or complications (Table I). There was no statistical difference between high-grade and low-grade renal injuries in terms of the need for surgery or nephrectomy. Eleven (18%) children sustained an isolated renal injury. Over a third of children with renal trauma sustained concurrent injuries of the thorax, head/ neck, liver or spleen (Table II).
Management
Forty children (66%) were successfully managed non-operatively and 21 required a laparotomy. Of those undergoing laparotomy, six (28%) required a nephrectomy. The overall renal salvage rate was 90% (55/61). Seven children required a repeat laparotomy. Children who required laparotomy were significantly more likely to have sustained a penetrating mechanism of injury (24% vs 2%) and have greater length of hospital stay, a median 9 vs 3 days, compared to children managed non-operatively (p < 0.05, Table III). Children who underwent a nephrectomy had a significantly greater length of hospital stay compared to those who did not, median 9 vs 4 days (p = 0.03). However, their demographics, outcomes and complications were otherwise not significantly different. There was a trend for children who underwent a laparotomy and nephrectomy to have a higher grade of renal injury than those who had no nephrectomy (median 4 [3-5] vs 3 [1-5], p = 0.105). Of the 11 children with an isolated renal injury, two required laparotomy (p = 0.31) and none underwent a nephrectomy. Thirty (49%) children required intensive care unit (ICU) admission. Ten (16.4%) required positive pressure ventilation. Median length of hospital stay was 5 (range 0-69) days, with 20 (33%) children being transferred to another centre for ongoing management. Twenty-four (39%) children developed complications which included respiratory (n = 8), renal (4), cardiac (3), abdominal (3) and neurological (3) systems. Three (5%) children developed a urinoma and eight (13%) a surgical site infection. Two (3%) children died; one managed non-operatively and one operatively. The patient managed non-operatively had a severe traumatic brain injury. The patient who underwent a laparotomy after sustaining blunt abdominal trauma died from multi-organ failure secondary to ischaemic bowel. Neither patient underwent a nephrectomy. There was no statistically significant difference in management and outcome between children with high-grade and low-grade renal injuries. No statistically significant differences in demographics, management, outcomes or complications were observed between children who died and survived. Angiographic embolisation was not used in any of these children.
Discussion
There is increasing evidence to support NOM of all grades of renal injury in children and adolescents.412 A recent metaanalysis generated a cohort of 5 561 children with renal trauma, of which 579 (10%) required surgery.4 Our rate of laparotomy is much higher, in the order of one third of all children. This may be explained by the relatively high rate (10%) of penetrating mechanism in our local cohort.4 The management of blunt and penetrating renal trauma is not analogous. The stable patient with blunt abdominal trauma can undergo an abdominal CT scan to grade the injury and guide NOM.12 In penetrating trauma, unstable children and those with clinical features of peritonitis undergo mandatory laparotomy and the renal injury may only be discovered at operation.
In our series, 10% (6/61) of children required a nephrectomy. This compares favourably with renal salvage rates in the range of 80-90% reported from recent studies.4,7-12 Comparison between the operative and non-operative group shows a higher frequency of penetrating mechanisms of injury and less frequent use of CT scan imaging in the operative group (Table III). It is the overall clinical scenario rather than the grade of injury which determines the need for operation. In the recent meta-analysis in the operative cohort, just under half (44.9%) required nephrectomy.4 In our operative cohort, only 28% required a nephrectomy. This may reflect our conservative approach in not exploring peri-renal haematomas acutely unless they are expanding or in cases of gross haemodynamic instability.
Grade of renal injury in itself is not associated with an increase in mortality or with increased likelihood of surgery or increased need for nephrectomy. This supports the growing consensus that relatively high-grade renal injuries can be managed non-operatively in children and adolescents. Grade of injury does not absolutely predict need for surgery or need for nephrectomy. As such, grade of injury is no longer central to managing these children. Other factors apart from grade of injury will determine the need for surgery in the acute setting.
Study limitations
This is a retrospective audit of a prospectively maintained data set and as such shares many of the limitations associated with such systems. However, this system is well validated and has extensive quality control mechanisms built into it. Limited sample size limits some statistical analysis.
Conclusion
Renal trauma in children and adolescents can be successfully managed non-operatively in over two-thirds of cases. Grade of injury does not absolutely predict the need for surgery or the need for nephrectomy, and high-grade injuries can be successfully managed non-operatively.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
Ethical approval for the HEMR has been granted by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (ref. no BE207/09 BCA 221/13). This approval is renewed annually and is current. The system has been functional since December 2012.
ORCID
VY Kong https://orcid.org/0000-0003-2291-2572
W Xu https://orcid.org/0000-0002-1270-2769
B Conradie https://orcid.org/0000-0002-9141-1467
DL Clarke https://orcid.org/0000-0002-8467-1455
JL Bruce https://orcid.org/0000-0001-8666-4104
GL Laing https://orcid.org/0000-0001-8075-0386
V Manchev https://orcid.org/0000-0001-9152-0092
W Bekker https://orcid.org/0000-0003-0695-5994
REFERENCES
1. Durso AM, Paes FM, Caban K, et al. Evaluation of penetrating abdominal and pelvic trauma. Eur J Radiol. 2020;130:109187. https://doi.org/10.1016/j.ejrad.2020.109187. [ Links ]
2. Kanlerd A, Auksornchart K, Boonyasatid P. Non-operative management for abdominal solid organ injuries: a literature review. Chin J Traumatol. 2022;25(5):249-56. https://doi.org/10.1016/j.cjtee.2021.09.006. [ Links ]
3. Leppâniemi A. Nonoperative management of solid abdominal organ injuries: from past to present. Scand J Surg. 2019;108(2):95-100. https://doi.org/10.1177/1457496919833220. [ Links ]
4. Hagedorn JC, Fox N, Ellison JS, et al. Paediatric blunt renal trauma practice management guidelines: collaboration between the Eastern Association for the Surgery of Trauma and the Paediatric Trauma Society. J Trauma Acute Care Surg. 2019;86(5):916-25. https://doi.org/10.1097/TA.0000000000002209. [ Links ]
5. LeeVan E, Zmora O, Cazzulino F, et al. Management of paediatric blunt renal trauma: a systematic review. J Trauma Acute Care Surg. 2016;80(3):519-28. https://doi.org/10.1097/TA.0000000000000950. [ Links ]
6. Margenthaler JA, Weber TR, Keller MS. Blunt renal trauma in children: experience with conservative management at a paediatric trauma centre. J Trauma. 2002;52(5):928-32. https://doi.org/10.1097/00005373-200205000-00018. [ Links ]
7. Rogers CG, Knight V, MacUra KJ, et al. High-grade renal injuries in children - is conservative management possible? Urology. 2004;64(3):574-9. https://doi.org/10.1016/j.urology.2004.04.069. [ Links ]
8. Henderson CG, Sedberry-Ross S, Pickard R, et al. Management of high-grade renal trauma: 20-year experience at a paediatric level I trauma centre. J Urol. 2007;178(1):246-50. https://doi.org/10.1016/jjuro.2007.03.048. [ Links ]
9. Umbreit EC, Routh JC, Husmann DA. Non-operative management of nonvascular grade IV blunt renal trauma in children: meta-analysis and systematic review. Urology. 2009;74(3):579-82. https://doi.org/10.1016/j.urology.2009.04.049. [ Links ]
10. Tsui A, Lazarus J, Van As AB. Non-operative management of renal trauma in very young children: experiences from a dedicated South African paediatric trauma unit. Injury. 2012;43(9):1476-81. https://doi.org/10.1016/j.injury.2010.12.027. [ Links ]
11. He B, Lin T, Wei G, He D, Li X. Management of blunt renal trauma: an experience in 84 children. Int Urol Nephrol. 2011;43(4):937-42. https://doi.org/10.1007/s11255-011-9965-2. [ Links ]
12. Redmond EJ, Kiddoo DA, Metcalfe PD. Contemporary management of paediatric high-grade renal trauma: 10-year experience at a level 1 trauma centre. J Pediatr Urol. 2020;16(5):656.e1-656.e5. https://doi.org/10.1016/jjpurol.2020.06.033 [ Links ]
13. Salem MS, Urry RJ, Kong VY, et al. Traumatic renal injury: five-year experience at a major trauma centre in South Africa. Injury. 2020;51(1):39-44. https://doi.org/10.1016/j.injury.2019.10.034. [ Links ]
 Correspondence:
Correspondence:
VY Kong
Email: victorywkong@yahoo.com














