Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.61 no.1 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3890
VASCULAR TRAUMA
Significant differences in functional outcome between upper and lower limbs after vascular trauma of the extremities
GM HohenbergerI; P KonstantiniukII; J Cambiaso-DanielIII; AM SchwarzIV; R KrassnigV; W PragerI; TU CohnertII
IDepartment of Trauma Surgery, State Hospital Feldbach-Fürstenfeld, Austria
IIDivision of Vascular Surgery, Department of Surgery, Medical University of Graz, Austria
IIIDivision of Plastic, Aesthetic and Reconstructive Surgery, Department of Surgery, Medical University of Graz, Austria
IVAUVA-Trauma Hospital (UKH) Styria Graz, Teaching Hospital of the Medical University of Graz, Austria
VUVA Rehabilitation Clinic Tobelbad, Austria
ABSTRACT
BACKGROUND: This study aimed to compare the functional results between upper (UE) and lower extremity (LE) following arterial reconstruction due to vascular trauma
METHODS: Patients treated for arterial injuries with vascular reconstruction at two centres between 2005 and 2014 were assessed. The physical fitness questionnaire - Fitnessfragebogen (FFB-Mot) - was evaluated. The differences between pre- and post-traumatic values were compared statistically for UE and LE. Inability to return to the preoperative workplace or postoperative loss of at least 10% of the FFB-Mot were defined as the primary outcome events
RESULTS: Twenty-seven patients could be re-evaluated. The primary outcome event occurred in 52% (14/27) without significant difference between UE (43%) and LE (62%) (p = 0.45). The difference between the pre- and post-traumatic FFB-Mot scores showed a significantly poorer functional outcome after LE vascular injury (p = 0.012
CONCLUSION: Results indicate a poorer functional outcome after vascular extremity trauma to the LE than to the UE
Keywords: vascular trauma, extremity trauma, upper limb vascular trauma, lower limb vascular trauma
Introduction
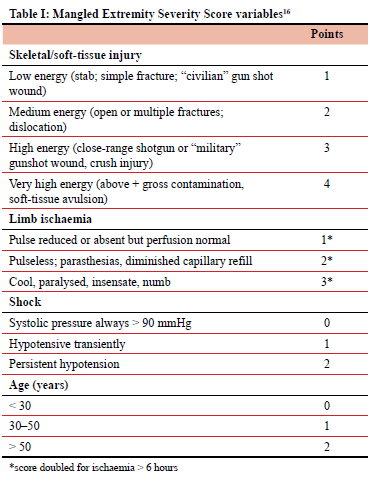
Approximately 1.6%1 to 4.4%2 of all civilian traumas involve vascular injuries; their frequency has tended to increase in recent years and the extremities are affected in 26.5%1 to 34%2. Amputations following these injuries decreased from 72.5% in 19463 to about 46%4 to 8%5 in military settings and 14.7%6 to 1.9%7 in civilian centres. Peripheral vascular trauma nonetheless remains a challenging life-and limb-threatening injury demanding rapid diagnosis and intervention.8-11 With respect to post-interventional outcomes, various studies have determined that concomitant injuries of the adjacent soft and skeletal tissues, especially neurological lesions, are the main reason for poor post-traumatic results.12-14 Prichayudh et al. reported significantly higher amputation rates following blunt vascular lesions when compared to penetrating traumas.15 Since current literature lacks detailed information on possible post-traumatic differences between upper (UE) and lower extremities (LE) following vascular injuries, this study aimed to compare the post-traumatic functional outcomes between UE and LE with comparable pre-interventional Mangled Extremity Severity Scores16 (MESS; Table I). The second aim of the study was to identify factors influencing the functional results after vascular injuries.
Materials and methods
Patient recruitment
All consecutive patients who presented with unilateral extremity trauma including arterial injury proximal to the radiocarpal or talocrural joint and underwent vascular reconstruction between January 2005 and December 2014 at a level I university trauma centre and a peripheral level III trauma centre were included in the study. Iatrogenic arterial lesions represented an exclusion criterion. Polytraumatised patients were included in the study; polytrauma was defined as the concomitant occurrence of traumas to different body parts, where the injuries, alone or combined, were potentially lethal.17
Patient characteristics
All data were collected prospectively in a dedicated vascular surgery database. Specific patient characteristics (age, gender) as well as trauma details (MESS, details on vascular trauma, muscular/neural/bone injuries, surgical procedures, secondary amputation rate of the traumatised extremity, duration of intensive care unit and hospital stay and inability to work) were evaluated retrospectively. The time interval between trauma and successful arterial reconstruction was defined as revascularisation time, and follow-up time as the timeline between trauma and patient assessment. Concerning trauma events, car and motorcycle events were classified separately from work accidents, even if they involved the way to or from work.
Outcome assessment
All patients were primarily contacted by telephone. If this was not successful, patients received an additional written study invitation by mail. As stipulated by the study protocol, patients were recalled to determine their current work status, sensory disorders, their score on the Canadian Study on Health & Aging (CSHA) Clinical Frailty Scale (CFS),18 and to fill in the pre- and postoperative physical fitness questionnaire (Fitnessfragebogen - FFB-Mot). The latter is a self-assessment instrument and includes 20 items concerning cardiorespiratory fitness, strength, flexibility, and coordination.19,20 The standard FFB-Mot score ranges from 20 to 100 points, with lower scores representing a poorer level of fitness (Appendix 1). Additionally, there are four sports scales and four activities of daily living (ADL) questions that were not included in the study according to the instructions for use of the original FFB-Mot publication. The CFS score ranges from 1 (very fit person) to 9 (terminally ill person) points (Appendix 1).
Postoperative inability to return to the pre-injury workplace was defined as the primary outcome event for comparison of UE and LE vascular injuries. Unemployability and change of workplace were regarded as equal to inability to resume previous employment. For retirees, a postoperative reduction of at least 10% of the FFB-Mot score was considered equivalent to the primary outcome event. Differences between pre- and post-interventional FFB-Mot and CFS values were defined as secondary outcome measures. To equalise the MOT for UE and LE, points from questions concerning the UE (2, 3, 5, 6, 18) were multiplied with 1.5, whereas the questions concerning the LE (9-13, 17, 19, 20, 23, 25) were multiplied with 0.75. The theoretically maximum score is equal to the original MOT (100 points).
Statistical analysis
All calculations were performed with Statistical Package for Social Sciences (SPSS) 21.0. Fisher's exact test was applied for comparison between UE and LE regarding the occurrence of an event as well as for the calculation of the impact of concomitant injuries thereupon. The t-test for unpaired samples was used to analyse differences between UE and LE regarding MESS, FBB-Mot, CFS and influence of concomitant injuries on FBB-Mot changes. P-values below 0.05 were considered statistically significant.
Results
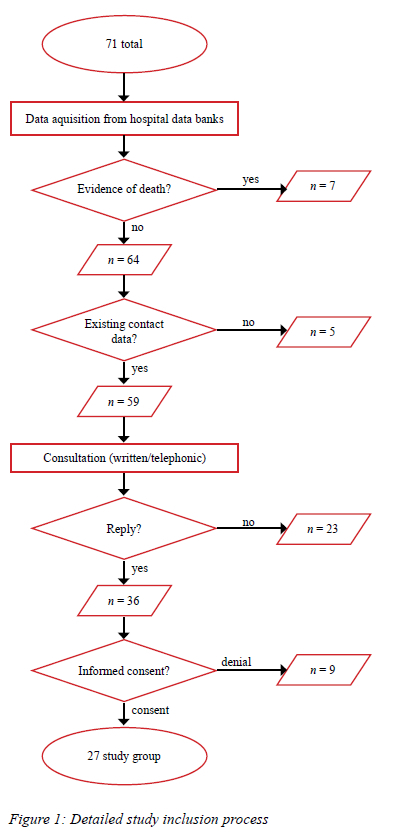
In total, 14 981 open surgical or endovascular procedures were performed at the department of surgery, division of vascular surgery of the level I centre between January 2005 and December 2014. Of these, 71 (0.47%) involved arterial reconstructions in patients with traumatised extremities. Sixty-one of these had undergone surgery at the level I and ten at the level III centre.
Twenty-seven patients signed informed consent and could be re-evaluated in 2015. The detailed study inclusion process can be seen in Figure 1. Eighty-two per cent (58/71) of the patients were males, and 18% were females. The mean age was 40.3 years. The UE was injured in 59% (42/71) and the LE in 41% (29/71) of cases. Detailed information on the total 71 patients has been published elsewhere.21
Comparison of re-evaluated and not re-evaluated groups
The re-evaluated and the not re-evaluated groups differed significantly concerning seven factors - age, incised wounds, performance of a preoperative computed tomography (CT), magnetic resonance tomography (MRT) and preoperative imaging in general, use of direct arterial suture and MESS (Table II) - 89 mm and range 0-29 at the median of the two measurement points (Table I).
Re-evaluated group
The mean follow-up time was 75.7 months (SD 33.6; range 16-124). Fifty-two per cent (14/27) of cases concerned the dominant and 48% (13/27) the non-dominant side. There was no statistically significant connection between handedness (left or right) and the traumatised body side (p = 0.62).
The trauma mechanism was blunt in 64.3% (9/14) of UE injuries and 92.3% (12/13) of LE injuries (p = 0.17). Thirty-seven per cent (10/27) of the patients sustained one or more fractures on the injured extremity, four of them (4/10) were open and six (6/10) closed fractures. In 41 per cent (11/27) of patients, a concomitant joint dislocation occurred, which affected the knee in six, the elbow in four and the symphyseal and iliosacral joints in one case. Additional injuries involved muscles (9/27; 33%) and nerves (13/27; 48%). In five cases only one nerve proved to be injured, and in eight cases at least two nerves were affected. In total, ten patients (37% of 27) underwent fasciotomy. Hereof, eight were conducted prophylactically during primary surgical intervention (four for UE and LE each) and two as a result of verified compartment syndrome (both LE).
Postoperative sensory disorders occurred in 78% (22/27); 79% (11/14) concerned the UE, 85% (11/13) the LE. Motor disorders were seen in 19% (5/27); 29% (4/14) affected the UE and 8% (1/13) the LE. Two patients suffered soft tissue infections (patient numbers 21 and 23 in supplementary Table III).
The mean MESS at admission showed no statistically significant difference (p = 0.754, Table IV) between UE (5.9) and LE (6.2). Inability to return to the pre-trauma workplace or post-traumatic loss of at least 10% of the FFB-Mot score was seen in 43% (6/14) for the UE and in 62% (8/13) for the LE (p = 0.449). In total, 14 patients returned to their pre-injury work (UE 9/14; LE 5/13), ten had to change jobs (UE 3/14; LE 7/13), and three patients became unemployable (UE 2/14; LE 1/13). The work changes took place as a result of a thigh amputation (1/10), reduction of strength (6/10) or due to a personal decision, which was not necessarily related to the trauma, of the respective patient (3/10). Cases of unemployability were related to a thigh amputation (1/3) or avulsion of the brachial plexus (2/3). The mean differences between pre- and post-interventional CFS scores did not differ significantly (p = 0.65) between the extremities. The differences between pre- and post-traumatic FFB-Mot scores showed a significantly (p = 0.012) poorer outcome for the LE (loss of 31.8%; SD 19.8%) than for the UE (loss of 13.3%; SD 15.8%). Regarding the concomitant injuries, muscular (p = 0.99) and neural lesions (0.27) as well as fractures (0.72) did not statistically influence the FFB-Mot difference. The latter was also not statistically influenced by age (p = 0.34) and secondary surgery (p = 0.066). The adapted version of the FFB-Mot also showed a statistically significantly (p = 0.048) poorer outcome for the LE (loss 30.5%; SD 19.9%) than for the UE (loss 15.5%; SD 17.3%).
Three patients (11%) underwent secondary amputation. Two of these concerned the thigh and one the lower leg. In the amputation group, the mean MESS was 7 points, with a range from 5 to 8. Hereof, one patient sustained primary dislocation of the knee joint including blunt injury of the popliteal artery including prolonged ischaemia time (> 6 hours). The patient underwent amputation of the thigh due to extensive muscular necrosis of the lower leg and had to change his job following amputation. The second case involved an open trauma of the common iliac artery including massive contamination. Thigh amputation was performed due to secondary femoral muscular necrosis and this patient became unemployable. The third case concerned a patient with dislocation of the knee joint, blunt injury of the popliteal artery and prolonged ischaemia time (> 6 hours). Lower leg amputation was required as a result of an infected haematoma of the medial ankle region. This patient was able to return to the pre-trauma workplace. The time intervals between the date of trauma and the amputation were 7 days (common iliac artery), 19 and 40 days (popliteal arteries). The mean loss of FFB-Mot points within the secondary amputation group was 33% (SD 13.8; range 13-42).
Discussion
The aim of this study was to compare the post-interventional results between UE and LE following vascular trauma with the main focus on functional outcomes. The primary outcome event, which was defined as inability to return to the preoperative workplace or a postoperative loss of at least 10% of the FFB-Mot questionnaire, occurred in 52% (14/27) without significant difference between UE (43%) and LE (62%) (p = 0.45). The difference between the pre-and post-traumatic FFB-Mot scores showed a statistically significantly poorer functional outcome after LE vascular injury (p = 0.012).
The surgical management of vascular extremity trauma is challenging. Haemorrhage control as well as maintenance of arterial and venous circulation are the main goals. The incidence of vascular injury has increased during the last decades with reference to large trauma centre reports.22 However, treatment strategies from wartime experiences have led to the improvement of interventional coping strategies, including a decrease of reported amputation rates.10,23
Regarding trauma mechanism, penetrating vascular lesions have been reported to be more frequent in comparison to blunt injuries.11 Dua et al. conducted a comparison between civilian versus military popliteal artery injuries, whereof the military group showed a significantly higher incidence of perforating traumas (96%) in comparison to the civilian group (30%).24 In Huynh et al., the trauma mechanism was mostly (74%) blunt in a civilian sample with LE vascular injuries.23 These findings are comparable to our blunt trauma rate (21/27; 77%). Contrastingly, Myers et al. reported a perforating trauma rate of 64% in a civilian collective of 80 patients, but their completely different wound-type distribution was due to a high number of gunshot- (11/80), stab- (7/80) and glass cut wounds (29/80).12 These injury types were not seen in our cases at all.
In contrast, amputation rates are stated as higher for vascular lesions due to blunt mechanisms.15 Klocker et al. evaluated a limb salvage rate of 98% in a sample of 89 patients who had sustained blunt UE injuries.25 This value is comparable to our sample since we observed no amputation in the UE subgroup. Popliteal artery injuries carry the highest amputation rates amongst all LE vascular injuries for both civilian and military patients.24,26 Ratnayake et al. observed a significantly higher delayed amputation rate after popliteal artery injuries for military (29%) in comparison to civilian patients (13%).26 Accordingly, the delayed amputation rate in our sample following popliteal artery injury was 25% (2/8). Liang and colleagues reported delayed amputation in 26% of their evaluated popliteal artery injuries; these patients sustained significantly more blunt traumas in comparison to the primary amputation group.27 These results are comparable to our collective (two amputations/eight popliteal artery injuries; 25% amputation rate).
Concerning affected vessels, Dua et al. observed the popliteal artery as the most commonly injured structure on the LE (22%).24 For the UE, reports either reveal the brachial artery as the most common affected vessel with rates from 34.6% up to 55%,15,22 or combined injuries of the radial and ulnar arteries.12 Among our patients, 50% (7/14) of all UE injuries concerned the brachial artery and for the LE, 62% (8/13) of the collective sustained a popliteal artery trauma.
Lesions of a second vessel occurred in 12 cases (44%), 75% of these were adjacent veins. This is a much higher rate in comparison to Markov et al. who observed an incidence of 23.4% of associated venous injuries in a civilian study group.28
With regard to patient age, data of military and civilian samples differ widely. Military reports include younger patients with age range from eight to 42 years,26,29 whereas civilian patients' age ranged from five up to 68 years.10,15,23 Our collective was comparable to the latter with a mean age of 34 years (SD 17.4; range 15-68) at time of trauma. Concerning gender distribution, vascular traumas tend to affect males more often with up to 89%,10 which was the same in our sample (24/27; 89%) and may be attributed to male risk behaviour.30
Dua et al. observed a significantly lower rate of knee dislocations in combination with popliteal artery lesions in their military collective (2%; 1/46 patients) in comparison to the civilian study group (30%; 19/64 patients).24 The knee dislocation rate within our popliteal artery injuries was much higher compared to the latter (75%, 6/8). This might be traced back to our higher MESS in the LE (6.2 in our sample and 5.1 in their civilian study group).
Associated fractures in patients with femoral artery injuries have been described as a risk factor for poor outcomes.31 Dragas et al. reported fractures of UE bones and brachial plexus injuries to be significant factors for limb loss.22 In our patients, muscular and neural lesions as well as fractures did neither statistically influence the main target sizes nor the FFB-Mot differences. The impact of concomitant lesions on the amputation rate could not be evaluated statistically due to the low number of cases (three LE major amputations).
The CFS has been proposed as a specific assessment for frailty.18 Up to now, literature only describes pre- and post-traumatic changes of its values in elder patients.32,33 Provencher and colleagues evaluated a collective with extremity fractures regarding their pre- and post-injury CFS.33 Their data are hardly comparable to ours since they used patients with at least 65 years (this study: mean of 34 years). The pre-trauma values of the CFS were between 1 and 2 points in 56.6%, between 3 and 4 in 32.2% and between 5 and 6 in 11.1%. This study sample had values of either 1 or 2 points in 96.3% of cases.
As a limitation of our study, only 27 out of 71 patients matching the defined inclusion criteria could be re-evaluated. It is possible that our sample is a positive selection of all treated patients since patients with satisfactory clinical results are more likely to accept invitations for follow-up studies than those with bad outcomes. Seven patients (7/71; 10%) had already died at the onset of this trial. More heavily injured patients have a worse life expectancy and therefore our study participants are likely to represent a positive selection. Because of the partially long-time interval between trauma and follow-up assessment (mean 75.7; SD 33.6; range 16-124 months) patients may have forgotten or upgraded their pre-traumatic FFB-Mot and CFS values. Regarding the FFB-Mot, only two questions (10%; 2/20) focus mainly on the UE whereas seven (35%; 7/20) concern the LE and eleven subitems (55%; 11/29) involve combined (LE, UE and trunk) activities. Due to this construction of the FFB-Mot a more detailed evaluation of the LE becomes possible and may have influenced our outcomes.
Conclusion
Concluding from our results, functional outcome after limb trauma with arterial reconstruction is worse for the LE compared to the UE. When assessed with the FFB-Mot, there was a significant difference (p = 0.012). This worse functional outcome was not associated with a higher rate of patients who were unable to return to their pre-trauma workplace.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
This study was approved by the Ethics Committee of the Medical University of Graz (27-460 ex 14/15) in accordance with the principles of the Declaration of Helsinki and the ICH-GCP guidelines. All patients gave their written informed consent to participate in the study.
ORCID
GM Hohenberger https://orcid.org/0000-0002-1831-9269
P Konstantiniuk https://orcid.org/0000-0002-4894-6810
J Cambiaso-Daniel https://orcid.org/0000-0003-2022-352X
AM Schwarz https://orcid.org/0000-0003-4369-9133
R Krassnig https://orcid.org/0000-0002-7628-7584
W Prager https://orcid.org/0000-0002-3310-3941
TU Cohnert https://orcid.org/0000-0001-7451-7588
REFERENCES
1. Barmparas G, Inaba K, Talving P, et al. Pediatric vs adult vascular trauma: a National Trauma Databank review. J Pediatr Surg. 2010;45(7):1404-12. https://doi.org/10.1016/j.jpedsurg.2009.09.017. [ Links ]
2. Perkins ZB, De'Ath HD, Aylwin C, et al. Epidemiology and outcome of vascular trauma at a British major trauma centre. Eur J Vasc Endovasc Surg. 2012;44(2):203-9. https://doi.org/10.1016/j.ejvs.2012.05.013. [ Links ]
3. Debakey ME, Simeone FA. Battle injuries of the arteries in World War II: an analysis of 2471 cases. Ann Surg. 1946;123(4):534-79.https://doi.org/10.1097/00000658-194604000-00005. [ Links ]
4. Al Wahbi A, Aldakhil S, Al Turki S, et al. Risk factors for amputation in extremity vascular injuries in Saudi Arabia. Vasc Health Risk Manag. 2016;12:229-32. https://doi.org/10.2147/VHRM.S91452. [ Links ]
5. Agrawal V, Bedi VS, Anand V, Garg MK. Management of vascular injury in counter insurgency area: a single-centre study. Indian Journal of Vascular and Endovascular Surgery. 2018;5(1):29. https://doi.org/10.4103/ijves.ijves_65_17. [ Links ]
6. Tanga C, Franz R, Hill J, Lieber M, Galante J. Evaluation of experience with lower extremity arterial injuries at an urban trauma center. Int J Angiol. 2018;27(1):29-34. https://doi.org/10.1055/s-0037-1618570. [ Links ]
7. Frech A, Pellegrini L, Fraedrich G, Goebel G, Klocker J. Long-term clinical outcome and functional status after arterial reconstruction in upper extremity injury. Eur J Vasc Endovasc Surg. 2016;52(1):119-23. https://doi.org/10.1016/j.ejvs.2016.03.028. [ Links ]
8. Fox CJ, Gillespie DL, O'Donnell SD, et al. Contemporary management of wartime vascular trauma. J Vasc Surg. 2005;41(4):638-44. https://doi.org/10.1016/jjvs.2005.01.010. [ Links ]
9. Doody O, Given MF, Lyon SM. Extremities - indications and techniques for treatment of extremity vascular injuries. Injury. 2008;39(11):1295-303. https://doi.org/10.1016/j.injury.2008.02.043. [ Links ]
10. Menakuru SR, Behera A, Jindal R, et al. Extremity vascular trauma in civilian population: a seven-year review from North India. Injury. 2005;36(3):400-6. https://doi.org/10.1016/j.injury.2004.06.017. [ Links ]
11. Rasouli MR, Moini M, Khaji A. Civilian traumatic vascular injuries of the upper extremity: report of the Iranian national trauma project. Ann Thorac Cardiovasc Surg. 2009;15(6):389-93. [ Links ]
12. Myers SI, Harward TR, Maher DP, et al. Complex upper extremity vascular trauma in an urban population. J Vasc Surg. 1990;12(3):305-9. https://doi.org/10.1016/0741-5214(90)90152-Z. [ Links ]
13. Sobnach S, Nicol AJ, Nathire H, et al. An analysis of 50 surgically managed penetrating subclavian artery injuries. Eur J Vasc Endovasc Surg. 2010;39(2):155-9. https://doi.org/10.1016/j.ejvs.2009.10.013. [ Links ]
14. Van der Sluis CK, Kucey DS, Brenneman FD, et al. Longterm outcomes after upper limb arterial injuries. Can J Surg. 1997;40(4):265-70. [ Links ]
15. Prichayudh S, Verananvattna A, Sriussadaporn S, et al. Management of upper extremity vascular injury: outcome related to the Mangled Extremity Severity Score. World J Surg. 2009;33(4):857-63. https://doi.org/10.1007/s00268-008-9902-4. [ Links ]
16. Johansen K, Daines M, Howey T, Helfet D, Hanse S. Objective criteria accurately predict amputation following lower extremity trauma. J Trauma. 1990;30(5):568-72; discussion 572-3. https://doi.org/10.1097/00005373-199005000-00007. [ Links ]
17. Tscherne H. Polytrauma management. 1st ed. Heidelberg: Springer; 1997. p. 225. [ Links ]
18. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489-95. https://doi.org/10.1503/cmaj.050051. [ Links ]
19. Boes K, Abel T, Woll A, et al. The Physical Fitness Questionnaire (FFB-MOT). Diagnostica. 2002;48(2):101-11. https://doi.org/10.1026//0012-1924.48.2.101. [ Links ]
20. Van Tulder R, Roth D, Havel C, et al. "Push as hard as you can" instruction for telephone cardiopulmonary resuscitation -a randomised simulation study. J Emerg Med. 2014;46(3):363-70. https://doi.org/10.1016/jjemermed2013.08.067. [ Links ]
21. Hohenberger GM, Konstantiniuk P, Cambiaso-Daniel J, et al. The Mangled Extremity Severity Score fails to be a good predictor for secondary limb amputation after trauma with vascular injury in Central Europe. World J Surg. 2020;44(3):773-9. https://doi.org/10.1007/s00268-019-05263-w. [ Links ]
22. Dragas M, Davidovic L, Kostic D, et al. Upper extremity arterial injuries: factors influencing treatment outcome. Injury. 2009;40(8):815-9. https://doi.org/10.1016/j.injury.2008.08.012. [ Links ]
23. Huynh TT, Pham M, Griffin LW, et al. Management of distal femoral and popliteal arterial injuries: an update. Am J Surg. 2006;192(6):773-8. https://doi.org/10.1016/j.amjsurg.2006.08.043. [ Links ]
24. Dua A, Patel B, Desai SS, et al. Comparison of military and civilian popliteal artery trauma outcomes. J Vasc Surg. 2014;59(6):1628-32. https://doi.org/10.1016/j.jvs.2013.12.037. [ Links ]
25. Klocker J, Falkensammer J, Pellegrini L, et al. Repair of arterial injury after blunt trauma in the upper extremity -immediate and long-term outcome. Eur J Vasc Endovasc Surg. 2010;39(2):160-4. https://doi.org/10.1016/j.ejvs.2009.11.019. [ Links ]
26. Ratnayake A, Samarasinghe B, Bala M. Outcomes of popliteal vascular injuries at Sri Lankan war-front military hospital: case series of 44 cases. Injury. 2014;45(5):879-84. https://doi.org/10.1016/j.injury.2014.01.003. [ Links ]
27. Liang NL, Alarcon LH, Jeyabalan G, et al. Contemporary outcomes of civilian lower extremity arterial trauma. J Vasc Surg. 2016;64(3):731-6. https://doi.org/10.1016/j.jvs.2016.04.052. [ Links ]
28. Markov NP, DuBose JJ, Scott D, et al. Anatomic distribution and mortality of arterial injury in the wars in Afghanistan and Iraq with comparison to a civilian benchmark. J Vasc Surg. 2012;56(3):728-36. https://doi.org/10.1016/jjvs.2012.02.048. [ Links ]
29. Salamon T, Lerner A, Rothem D, et al. Retrospective analysis of case series of patients with vascular war injury treated in a district hospital. Injury. 2016;47(4):811-7. https://doi.org/10.1016/j.injury.2016.02.008. [ Links ]
30. Paquette L, Dumais M, Bergeron J, Lacourse E. The effect of personality traits and beliefs on the relationship between injury severity and subsequent sport risk taking among adolescents. Pediatric Research International Journal. 2016;2016:1-14. https://doi.org/10.5171/2016.405500. [ Links ]
31. Yavuz C, Demirtas S, Caliskan A, et al. The predictors of poor outcomes in patients with femoral artery injuries. Eur Rev Med Pharmacol Sci. 2013;17(14):1901-8. [ Links ]
32. Masud D, Norton S, Smailes S, et al. The use of a frailty scoring system for burns in the elderly. Burns. 2013;39(1):30-36. https://doi.org/10.1016/j.burns.2012.03.002. [ Links ]
33. Provencher V, Sirois MJ, Émond M, et al. Frail older adults with minor fractures show lower health-related quality of life (SF-12) scores up to six months following emergency department discharge. Health Qual Life Outcomes. 2016;14:40. https://doi.org/10.1186/s12955-016-0441-7. [ Links ]
 Correspondence:
Correspondence:
GM Hohenberger
Email: hohenberger.gloria@gmail.com
Appendix 1
FFB-Mot questionnaire
For self-assessment of motor skills related to endurance, strength, mobility and coordination Choose the appropriate answer (1-5) to each of the following 28 questions:
1. I am not able to perform this activity.
2. I have major problems performing this activity.
3. I have moderate problems performing this activity.
4. I have minor problems performing this activity.
5. I have no problems performing this activity.
The simplest (1, 8, 15, 22) and most difficult (7, 14, 21, 28) activities are not included in your final score but may help you to assess your degree of fitness. Questions: Are you able to... Self-assessment of strength
1. get up from a chair without using your arms?
2. carry a heavy shopping basket (8 kilos) up several floors?
3. carry a full beverage carton down to the basement?
4. lift your upper body from a supine position without using your arms (sit-up)?
5. lift a heavy suitcase above your head (e.g., onto the baggage rack on a train)?
6. carry two heavy suitcases up several floors?
Self-assessment of endurance
7. lift a dumbbell that is as heavy as you are?
8. walk several blocks quickly?
9. go up several floors without stopping?
10. walk two kilometres fast without stopping?
11. jog one kilometre without stopping?
12. jog 30 minutes without stopping (about 5 kilometres)?
13. jog one hour without stopping (about 10 kilometres)?
14. run a marathon (42 kilometres)?
Self-assessment of mobility
15. get in and out of a tight pullover and socks by yourself?
16. touch the floor with both hands while sitting on a chair?
17. tie your shoes while standing?
18. touch your shoulder blade with your hand from below?
19. touch the floor with both hands while standing (knees locked)?
20. touch your locked knees with your head while standing?
21. do the splits?
Self-assessment of coordination
22. go down stairs without using the handrail?
23. stand on a one leg without holding on?
24. do a somersault?
25. dribble a ball while walking fast?
26. vault over a one-metre-high fence?
27. do a somersault off a one-metre diving board?
28. do a cartwheel?














