Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.61 n.1 Cape Town 2023
http://dx.doi.org/10.36303/SAJS.3796
SURVEY: OPINION
The supernumerary registrar experience in KwaZulu-Natal
A Gxobole; R Naidoo; B Singh
Department of Surgery, Nelson Mandela School of Medicine, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: We sought to assess the experiences of trainees enrolled in the supernumerary registrar programme at the University of KwaZulu-Natal, South Africa, with a specific focus on their assimilation into host clinical units and their intentions to return to their home countries upon completion of the training
METHODS: This was a cross-sectional survey involving 50 supernumerary registrars attached to six academic hospitals affiliated with the University of KwaZulu-Natal. The survey collected information on registrar's demographics and financial support, speciality, opportunities for advanced training in their home country, assimilation into host clinical units and intentions to return home upon completing the training. The survey data were analysed using descriptive statistics
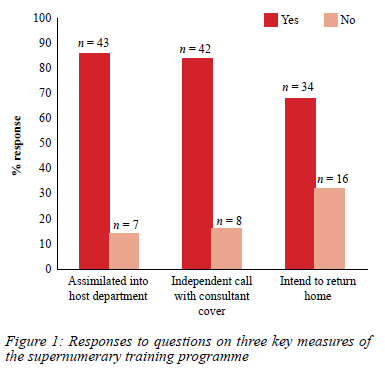
RESULTS: The majority of supernumeraries were < 36 years old (n = 32, 64%), male (n = 31, 62%), and self-funded (n = 31, 62%). Only a few supernumeraries were associated with a training facility in their home country (n = 9, 18%). Most supernumeraries (n = 44, 88%) reported not having an equivalent training programme in their home country. Awareness of the programme was predominantly acquired through self-research (n = 35, 70%), and the application process was perceived as problematic by many supernumeraries (n = 46, 92%). Most supernumeraries (n = 43, 86%) assimilated into their host clinical units, and nearly one-third (n = 16, 32%) did not plan on returning home upon completion of their training
CONCLUSION: Most supernumerary registrars assimilate into host clinical units and play an important role in service delivery during their training. Mechanisms should be put in place to facilitate retention of these individuals in their home countries upon completion of their training
Keywords: supernumerary registrar, trainee, capacity development, Africa
Introduction
The critical shortage of medical professionals in Africa, more especially sub-Saharan Africa, has been a perennial problem.1 Great efforts have since been made to improve the number of doctors trained on the continent by concentrating on strengthening primary healthcare in the region.2 As primary healthcare standards continue to improve in sub-Saharan Africa, the need for specialist care will inevitably increase as well. Currently, there is a shortage of medical specialists in many sub-Saharan African countries and even in countries where specialists practise, these individuals are concentrated in urban areas.3
The capacity for medical specialist training on the African continent is severely limited.46 Specialist training in Africa has traditionally followed one of the following training routes: training programmes in high-income countries (HICs), training programmes run solely in sub-Saharan Africa which are supported by HIC partners, training programmes run by regional accreditation bodies such as the West African and East African Colleges of Physicians and Surgeons, university-based training programmes in other sub-Saharan African countries and other training partnerships between African countries.7
Although there are advantages to training sub-Saharan African doctors in HICs which include access to highly skilled trainers and other sophisticated resources, this might not adequately prepare them to render specialist services in the resource-constrained hospitals of their home country. Another disadvantage of a training route in a HIC is that it may facilitate emigration of sub-Saharan African doctors to these HICs. Sub-Saharan training supported by HICs relies on funding and continued interest and support from HICs, which is not guaranteed and hence cannot be considered a long-term solution for postgraduate medical training in sub-Saharan Africa. Thus, the other training routes appear to be more feasible options for sub-Saharan African doctors who wish to gain specialist medical training. University-based training in serving sub-Saharan Africa is well established in South Africa and is one of the preferred options for medical specialist training on the African continent. South Africa is in a unique position to lead efforts in improving medical care on the continent through medical education programmes. The South African medical specialist training programme is internationally benchmarked, but also adequately prepares its trainees to tackle the disease and healthcare system challenges which the African continent currently faces.7,8
The supernumerary medical registrar programme has been in existence at the Nelson R Mandela School of Medicine, University of KwaZulu-Natal, South Africa, since the mid-1990s.9 This programme admits doctors from African countries to enter postgraduate medical training programmes in South Africa. These registrars join the local programmes and assume the responsibilities of local
South African trainees. The original programme saw these doctors being paired with local trainees. Furthermore, these doctors were unpaid and considered additional staff beyond that of the local South African trainees, hence the term "supernumerary".9
In recent years, the South African public health system has been plagued by budget cuts and staff shortages.10,11 This has led to supernumerary registrars being incorporated into the normal staff pool at public hospitals and assisting with clinical service delivery.9 Supernumerary registrars can comprise up to 25% of the total registrar body in some South African clinical departments.12 Traditionally, the supernumerary registrars are expected to return to their home countries and use their newly acquired skills to enhance the level of healthcare and engage in capacity development of other doctors in their home country.9 There are, however, no legally binding agreements in place to ensure that this occurs. It is therefore possible that a proportion of the supernumerary registrar cohort will not return to their home countries upon completion of their specialisation, but may choose to remain in South Africa or pursue opportunities in HICs for a variety of reasons.
The aim of this study was to investigate two important aspects of the supernumerary registrar training programme at the Nelson R Mandela School of Medicine, University of KwaZulu-Natal, South Africa - whether the programme provides a supportive environment for supernumerary specialist training with the goal of improving health care and uplifting medical education on the African continent, and the intentions of the supernumerary registrars to return to their home country following completion of their training in South Africa.
Methods
Study design and setting
This was a survey conducted at University of KwaZulu-Natal, South Africa. The supernumerary trainees approached were attached to the six academic hospitals, all affiliated to the University of KwaZulu-Natal.
Participants
Supernumerary registrars were identified as non-South African citizens who were registered for a "Masters of Medicine" postgraduate degree at the University of KwaZulu-Natal. The supernumerary registrars were approached to participate in the survey at departmental academic meetings held at the Nelson R Mandela School of Medicine campus of the University of KwaZulu-Natal. Only registrars who provided written informed consent completed the survey.
Survey procedure
The survey was conducted in 2018 and 2019. The survey instrument was developed in consultation with senior academic staff at the Nelson R Mandela School of Medicine, University of KwaZulu-Natal, and incorporated feedback from an initial pilot study conducted in three registrars. The survey instrument collected information on participant demographics and host discipline, source of financial support, association with a training institution in home country, existence of a comparable registrar training programme in home country, experience with applying to the South African training programme, the role of supernumerary registrars in the host clinical unit in comparison to the local registrar, and the intention of the supernumerary registrars to return to their home country once the training has been completed. The survey was anonymised and information on the participant's nationality was not collected, given the concerns around confidentiality and the potential for discrimination which was voiced by the registrars who were involved in the pilot study. Registrars who agreed to participate were given the paper-based survey and afforded up to two weeks to complete it. Data from the returned paper surveys were transferred to a Microsoft Excel spreadsheet for the statistical analysis.
Statistics
The survey data were analysed descriptively using the Statistical Package for the Social Sciences (SPSS) version 27.0 (IBM, USA). Survey responses are presented as counts and percentages. Where appropriate, the data has been graphically represented using simple bar charts constructed in Microsoft Excel.
Results
The final study sample was composed of 50 supernumerary registrars (response rate of 96%). The characteristics of the study sample are presented in Table I. Most registrars were < 36 years old (n = 32, 64%), and male (n = 31, 62%). Fifty-four per cent (n = 27) of all registrars who participated in the survey were in their final year of study. Approximately two-thirds of all registrars were self-funded (n = 31, 62%). The greatest proportion of registrars were from the general surgery discipline (n = 15, 30%). Relatively few registrars were associated with a training facility in their home country (n = 9, 18%). The vast majority of registrars (n = 44, 88%) reported not having an equivalent training programme in their home country. Awareness of the supernumerary registrar programme was predominantly acquired through self-research (n = 35, 70%). Most registrars reported that the application process was a very complex one (n = 47%).

A presentation of the responses to three key measures of the supernumerary registrar programme states: firstly, if they were absorbed into the host clinical department with the same clinical and academic responsibilities and opportunities as South African trainees; secondly, if they were extraneous staff with limited clinical participation and did independent calls with consultant cover; and thirdly, if they intended to return home. Figure 1 shows the participants' responses. It was common for the registrars to be absorbed into their host clinical service unit as part of the normal staff complement (n = 43, 86%). It was also common for supernumerary registrars to perform independent calls with consultant cover in their host clinical service unit (n = 42, 84%). Nearly one-third of all supernumerary registrars who participated in the survey indicated that they would not return to their home country following the completion of their training in South Africa (n = 16, 32%).
Discussion
Our findings suggest that the supernumerary registrar training programme at the Nelson R Mandela School of Medicine, University of KwaZulu-Natal, offers an enabling environment for medical specialist training of foreign doctors. This is evidenced by the fact that 86% of the registrars confirmed being absorbed into the local clinical units as the part of the normal staff complement. In recent years, funded specialist training posts for local doctors in the province of KwaZulu-Natal have been drastically reduced. The programme, however, has the capacity to train many more specialists than the province can fund. This presents a unique opportunity for foreign trainees as they have been absorbed into the local programme as equals. This allows for them to be supervised and mentored by senior registrars early in their careers and progressively given independence on calls and on theatre slates adhering to the accepted design of individual speciality training programmes.
It was noted that 28% of registrars interviewed became aware of the programme by word of mouth, which suggests that there would have been some positive feedback relayed to prospective trainees by registrars who returned to their home country upon completion of their training. Our finding that 70% of registrars self-researched the training programme does highlight the need to introduce a formal method of promoting the programme and trainee recruitment. This should endeavour to foster relations with other African countries or universities in these countries. Improvements to the application process might also be required, as failure to do so may deter future applicants. The application process is cumbersome with multiple facets that include qualification verification to attain limited registration with the Health Professionals Council of South Africa, applications to individual universities and their affiliated health departments, and finally the acquisition of a work permit.9
Eighty-four per cent of supernumerary registrars in our study reported working independently on call with consultant cover, as do the local registrars. This is advantageous when compared with specialisation in HICs, where foreign trainees have limited clinical experience. It is also advantageous when compared with hybrid programmes between HICs and African countries, as the trainees have access to personal supervision by their trainers. Furthermore, current South African supernumerary registrar programmes represent a mutually beneficial relationship for both the registrar and the South African Department of Health, which benefits from the pro bono clinical services delivered by the supernumerary registrar.9
Worryingly, a sizable portion of the supernumerary registrars who participated in our survey (32%) expressed that they did not wish to return to their home countries upon completion of the training. In contrast, a University of Cape Town study reported a 96% sub-Saharan retention rate with most of the supernumerary registrars in the Cape Town study being government-funded or sponsored and only 20% self-funded.8 However, most registrars in our study (86%) were self-funded through their own personal funds or student loans and are thus not obliged to return home as would be required for those who received government bursaries or scholarships. Another important finding from our survey was that 82% of supernumerary registrars were not associated with a training facility in their home country. It is suggested that these are crucial factors which inform the decision of supernumerary registrars to return to their home country upon completion of their training in South Africa. Although one can empathise with these doctors, their failure to return home and make good on the expectation of the supernumerary trainee programme is of concern as this means that the skills acquired are not being used to improve the health of the population in their home country, nor is there a skills transfer to the doctors that remain in their country.
This study revealed that 62% of supernumerary registrars affiliated with the University of KwaZulu-Natal were male. This may reflect the profession in Africa, but we also feel that females are less likely to study in a foreign country due to safety concerns, cultural norms, or family obligations. For the aspirant female specialist trainee on the continent, access to higher training is also curtailed if the newly trained supernumerary registrars fail to transfer skills by not returning to their home country.
South Africa has a definite role to play in higher medical education and training within the African continent. An overwhelming 88% of survey participants reported that there was no comparable training programme in their home country. The University of KwaZulu-Natal has much to offer in terms of medical training. In recent years, the university has created decentralised teaching centres to accommodate the South African-Cuban collaboration undergraduate medical student programme.13 These centres are now well equipped to accommodate these undergraduate students. In preparation for these students, staffing was improved at various regional hospitals. Given the adoption of virtual teaching practices in the era of global infectious disease pandemics, it is easy to fathom that postgraduate training will be able to piggyback on this resource. The peripheral hospitals with their specialist consultants will be able to provide clinical support for the supernumerary registrars while they have access to university teaching. The presence of supernumerary registrars in peripheral hospitals will also bolster the undergraduate and junior doctor teaching capacity.
This study has limitations - the survey instrument did not collect information on the nationality of the supernumerary registrars, it is therefore not possible to identify to which countries the return of supernumerary registrars must be improved. The survey was conducted in a single metropolitan area in the KwaZulu-Natal Province, which might have a distinct supernumerary registrar profile from other cities or provinces in South Africa. Thus, the generalisability of the study findings to groups of supernumerary registrars in other cities or provinces in South Africa might be limited.
Conclusion
Supernumerary registrar programmes in South Africa have the potential to improve the quality of healthcare in sub-Saharan Africa through increasing access to specialist medical education and training. In return, the South African health system benefits from the role they play in delivering specialist medical services in the South African public healthcare system, which serves the healthcare needs of the majority of South Africans. We recommend that the South African Departments of Health and Higher Education devise a policy for the postgraduate training of foreign doctors. Consideration should be given to drafting this policy in consultation with other African governments, to make this venture profitable for healthcare across the continent. We also feel that this would be a key step in ensuring the retention and transfer of specialist medical skills on the continent.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
This research was approved by the Biomedical Research Ethics Committee at the University of KwaZulu-Natal, South Africa (Protocol reference BE500/18).
ORCID
A Gxobole https://orcid.org/0000-0002-8431-9793
R Naidoo https://orcid.org/0000-0002-1992-5615
B Singh https://orcid.org/0000-0003-0799-256X
REFERENCES
1. Naicker S, Plange-Rhule J, Tutt RC, Eastwood JB. Shortage of healthcare workers in developing countries-Africa. Ethn Dis. 2009;19(1 Suppl 1):S1-60-64. [ Links ]
2. Strasser R, Kam SM, Regalado SM. Rural health care access and policy in developing countries. Annu Rev Public Health. 2016;37:395-412. https://doi.org/10.1146/annurev-publhealth-032315-021507. [ Links ]
3. Flinkenflögel M, Sethlare V, Cubaka VK, et al. A scoping review on family medicine in sub-Saharan Africa: practice, positioning and impact in African health care systems. Hum Resour Health. 2020;18(1):27. https://doi.org/10.1186/s12960-020-0455-4. [ Links ]
4. Greysen SR, Dovlo D, Olapade-Olaopa EO, et al. Medical education in sub-Saharan Africa: a literature review. Med Educ. 2011;45(10):973-86. https://doi.org/10.1111/j.1365-2923.2011.04039.x. [ Links ]
5. Schluger NW, Sherman CB, Binegdie A, et al. Creating a specialist physician workforce in low-resource settings: reflections and lessons learnt from the East African Training Initiative. BMJ Glob Health. 2018;3(5):e001041. https://doi.org/10.1136/bmjgh-2018-001041. [ Links ]
6. Chen C, Buch E, Wassermann T, et al. A survey of sub-Saharan African medical schools. Hum Resour Health. 2012;10:4. https://doi.org/10.1186/1478-4491-10-4. [ Links ]
7. Cox M, Masunge J, Nkomazana O. Postgraduate medical specialty training for Botswana - a successful innovative partnership with South Africa. Afr J Health Professions Educ. 2020;12(2):53-5. https://doi.org/10.7196/AJHPE.2020.v12i2.1221. [ Links ]
8. Naidu P, Fagan JJ, Lategan C, Devenish LP, Chu KM. The role of the University of Cape Town, South Africa, in the training and retention of surgeons in sub-Saharan Africa. Am J Surg. 2020;220(5):1208-12. https://doi.org/10.1016/j.amjsurg.2020.06.070. [ Links ]
9. Naidoo R, Singh B. Supernumerary registrars: are we helping them or are they helping us? S Afr J Surg. 2017;55(2):38-39. [ Links ]
10. Hlafa B, Sibanda K, Hompashe DM. The impact of public health expenditure on health outcomes in South Africa. Int J Environ Res Public Health. 2019;16(16):2993. https://doi.org/10.3390/ijerph16162993. [ Links ]
11. Maphumulo WT, Bhengu BR. Challenges of quality improvement in the healthcare of South Africa post-apartheid: a critical review. Curationis. 2019;42(1):e1-e9. https://doi.org/10.4102/curationis.v42i1.1901. [ Links ]
12. Peer S, Burrows SA, Mankahla N, Fagan JJ. Supernumerary registrar experience at the University of Cape Town, South Africa. S Afr Med J. 2016;107(1):76-79. https://doi.org/10.7196/SAMJ.2016.v107.i1.11345. [ Links ]
13. Bateman C. Doctor shortages - unpacking the 'Cuban solution'. S Afr Med J. 2013;103(9):603-5. https://doi.org/10.7196/SAMJ.7323. [ Links ]
 Correspondence:
Correspondence:
R Naidoo
Email: ruvashni@gmail.com














