Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.4 Cape Town Dec. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3865
CASE REPORT
Transdiaphragmatic pericardial washout post penetrating cardiac injury found incidentally at diagnostic laparoscopy
H WainI; V ManchevI, II; JL BruceI, II; W BekkerII; DL ClarkeII, III, IV
IDepartment of Surgery, Harry Gwala Regional Hospital, South Africa
IIDepartment of Surgery, University of KwaZulu-Natal, South Africa
IIIDepartment of Surgery, Greys Hospital, South Africa
IVDepartment of Surgery, University of the Witwatersrand, South Africa
SUMMARY
A 22-year-old male presented following a precordial stab. He was haemodynamically and metabolically normal. Initial investigations did not reveal pericardial fluid or haemothorax. At diagnostic laparoscopy, we encountered haemoperi-toneum and a diaphragmatic injury through which the heart was visible. After pericardial washout, laparoscopic repair was effected. This case highlights a potential problem with extended focused assessment with sonography in trauma (eFAST) in that it will only be positive if there is an accumulation of pericardial fluid. It also confirms the utility of diagnostic laparoscopy for penetrating left thoracoabdominal injuries and shows that principles of open surgery can be safely applied laparoscopically in select patients.
Keywords: left thoracoabdominal penetrating injury, penetrating cardiac injury, diagnostic laparoscopy, stab heart, eFAST
Case report
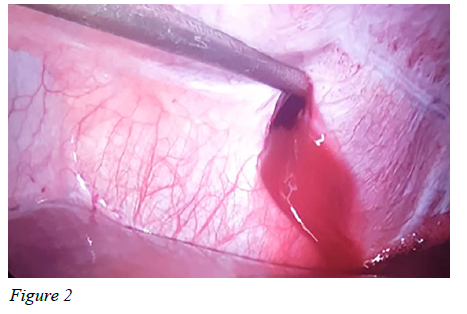
A 22-year-old male presented to the emergency department following a precordial stab with a spear approximately 12 hours prior. On arrival, he was haemodynamically normal, normothermic, Glasgow Coma Scale (GCS) 15/15, and had normal blood gas. He had a 2 cm wound approximately 3 cm above the left anterior costal margin, mid-way between the sternum and nipple. He had normal heart and respiratory sounds, and no raised jugular venous pulsation. His abdomen was mildly tender generally, but there were no signs of peritonism. Erect chest radiography did not reveal any free sub-diaphragmatic air or evidence of haemopneumothorax. Extended focused assessment with sonography in trauma (eFAST ) showed free intraperitoneal fluid, no pericardial fluid, and no evidence of pleural injury. As per local policy, he was considered a candidate for selective non-operative management (SNOM) of his abdominal injury and offered diagnostic laparoscopy in view of the left-sided thoracoabdominal stab. Whilst in the ward, he did not demonstrate the need for urgent laparotomy. He underwent diagnostic laparoscopy three days post injury. Upon entry, a significant amount of haemoperitoneum was encountered. A 10 mm defect to the diaphragm overlying the pericardium was noted (Figure 1), through which the heart could be visualised. Further ports were inserted under vision to facilitate pericardial washout. Initially this was bloody but was continued until the wash ran clear (Figure 2). No cardiac injury could be identified, however, the presence of blood in the pericardium was suspicious for cardiac injury. The diaphragmatic defect was then closed with interrupted Ethibond™ 1, and abdomen suctioned clear of haemoperitoneum. A small liver laceration to segment II was noted and required no further management. The following day there was no pericardial fluid on ultrasonography, and the patient was discharged uneventfully. On review three weeks later, there was no pericardial fluid identified on transthoracic pericardial ultrasonography.

Discussion
Penetrating thoracic and thoracoabdominal trauma is a common reason for presentation to emergency departments across South Africa. All patients presenting with penetrating thoracoabdominal injuries are investigated and managed according to standard protocols. Those who require urgent surgery are offered such. Those who do not immediately meet criteria for operative management are assessed for their suitability for SNOM, a decision based on haemodynamic and metabolic status, radiographic findings, as well as clinical thoracic and abdominal assessment. Those with left-sided thoracoabdominal penetrating injuries are offered diagnostic laparoscopy to assess for diaphragmatic injury. Similarly, the assessment and management of penetrating precordial injuries follow a standard protocol. Those who need surgery upfront receive it. The patients who are haemodynamically and metabolically well are investigated by means of eFAST, chest radiography, and usually electrocardiograph (ECG). Serum cardiac enzymes do not form part of the standard assessment. Those with a significant pericardial effusion, but who are well, are offered a subxiphoid pericardial window (SPW) in a manner similar to that popularised by Nicol et al.1
This case highlights some important points. Firstly, the utility of eFAST in penetrating precordial injuries is limited to the detection of pericardial fluid, and in cases where the fluid is unable to collect, the eFAST will be falsely negative. This is demonstrated in the sensitivity of 20%, but specificity of 100% noted in our unit by Kong et al.2 Several authors have noted that the presence of a haemothorax concurrent with a penetrating cardiac injury may result in a 'false negative' on eFAST.34 As highlighted in this case, intra-abdominal free fluid in eFAST may be a harbinger of a false negative, meaning that a 'negative' eFAST (for pericardial fluid) in the presence of a haemothorax or free intra-abdominal fluid should possibly be viewed with some caution. This caveat perhaps enhances the utility of electrocardiography in the diagnosis of penetrating cardiac injury, as the presence of a J-wave bares an 85% specificity for the same.5 This may be of some use in patients who have a negative eFAST but a haemothorax or free abdominal fluid. Unfortunately, our patient did not have an ECG preoperatively.
Secondly, this case affirms the usefulness of diagnostic laparoscopy for left-sided thoracoabdominal penetrating injury. Our patient had no clinical signs of significant intra-peritoneal injury and was observed according to standard principles ofSNOM yet was found to have high-risk pathology at operation. Publications from our local unit,67 as well as others in South Africa8 have shown that a significant number of patients undergoing diagnostic laparoscopy are found to have diaphragmatic injuries that were not detected by other means (range 7-48%). The natural course of undiagnosed, and therefore unmanaged, left-sided diaphragmatic injuries is not known, but it is widely accepted that the sequelae of intra-abdominal organs herniating into the left hemithorax are potentially devastating. Considering that other means of diagnosing diaphragmatic injury are so fraught with inaccuracy, we offer all patients with penetrating left-sided thoracoabdominal injuries diagnostic laparoscopy.
Finally, our case shows that select principles from open operative techniques can be safely applied in the laparoscopic domain, and the presence of significant pathology is not necessarily an indication for immediate conversion. The principle of SPW is that, upon encountering haemopericardium, this is irrigated and observed, and if no ongoing bleeding is apparent then the need for further exploration is obviated. Similarly, in this case, laparosco-pic transdiaphragmatic pericardial washout proved a safe method to assess for and exclude ongoing cardiac bleeding. This was, however, an incidental finding in a patient who happens to have self-selected to survive a penetrating cardiac injury, and we thus do not believe this to be an appropriate method of investigation in all patients in whom cardiac injures are suspected. Diagnostic laparoscopy remains standard in our institution for assessment of the diaphragm following a left thoracoabdominal penetrating injury, and SPW remains standard for pericardial washout. There are reports in the literature detailing transdiaphragmatic pericardial washout for recurrent pericardial effusions from non-surgical disease,9 as well as planned transdiaphragmatic pericardial washout following suspected penetrating cardiac trauma.10 It is evident, however, that most surgeons prefer either subxiphoid or transthoracic/thoracoscopic pericardial assessment.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Written consent was obtained from the patient for use in this case report. Class approval for the database kept by our department is BCA 13/209, of which this submission is a sub-study.
ORCID
Η Wain https://orcid.org/0000-0002-6693-0062
V Manchev https://orcid.org/0000-0001-9152-0092
JL Bruce https://orcid.org/0000-0001-8666-4104
W Bekker https://orcid.org/0000-0003-0695-5994
DL Clarke https://orcid.org/0000-0002-8467-1455
REFERENCES
1. Nicol AJ, Navsaria P, Hommes M, et al. Sternotomy or drainage for a hemopericardium after penetrating trauma: a randomised controlled trial. Ann Surg. 2014;259(3):438-42. https://doi.org/10.1097/SLA.0000000000001146. [ Links ]
2. Kong VY, Oosthuizen G, Sartorius B, Bruce J, Clarke DL. Penetrating cardiac injuries and the evolving management algorithm in the current era. J Surg Res. 2015;193(2):926-32. https://doi.org/10.1016/jjss.2014.09.027. [ Links ]
3. Nicol AJ, Navsaria P, Beningfield S, Hommes M, Khan D. Screening for occult penetrating cardiac injuries. Ann Surg. 2015;261(3):573-8. https://doi.org/10.1097/SLA.0000000000000713. [ Links ]
4. Ball CG, Williams B, Wyrzykowski A, et al. A caveat to the performance of pericardial ultrasound in patients with penetrating cardiac wounds. J Trauma Acute Care Surg. 2009;67(5):1123-4. https://doi.org/10.1097/TA.0b013e3181b16f30. [ Links ]
5. Nicol AJ, Navsaria PH. The J-wave: a new electrocardio-graphic sign of an occult cardiac injury. Injury. 2014;45(1):112-5. https://doi.org/10.1016/j.injury.2013.06.015. [ Links ]
6. D'Souza N, Bruce JL, Clarke D, Laing GL. Laparoscopy for occult left-sided diaphragm injury following penetrating thoracoabdominal trauma is both diagnostic and therapeutic. Surg Laparosc Endosc Percutan Tech. 2016;26(1):e5-e8. https://doi.org/10.1097/SLE.0000000000000239. [ Links ]
7. D'Souza N, Clarke D, Laing G. Prevalence, management and outcome of traumatic diaphragm injuries managed by the Pietermaritzburg Metropolitan Trauma Service. Ann R Coll Surg Eng. 2017;99(5):394-401. https://doi.org/10.1308/rcsann.2017.0029. [ Links ]
8. Koto MZ, Matsevych OY, Aldous C. Diagnostic laparoscopy for trauma: how not to miss injuries. J Laparoendosc Adv Surg Tech. 2018;28(5):506-13. https://doi.org/10.1089/lap.2017.0562. [ Links ]
9. Totte E, Van Brabant P, Wollaert B, et al. Laparoscopic transabdominal pericardial window. Surg Endosc. 2002;16(5):859-63. https://doi.org/10.1007/s004640090128. [ Links ]
10. McMahon D, Sing R, Hoff W, Schwab C. Laparoscopic transdiaphragmatic diagnostic pericardial window in the hemodynamically stable patient with penetrating chest trauma. Surg Endosc. 1997;11(5):474-5. https://doi.org/10.1007/s004649900394. [ Links ]
 Correspondence:
Correspondence:
email: howardwain@icloud.com














