Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.60 no.4 Cape Town dic. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3725
CASE REPORT
Colonic perforation in a right atraumatic diaphragmatic hernia
N AllopiI; MH WellmannI; VR BlancoII
IDepartment of Surgery, Tygerberg Hospital, Stellenbosch University, South Africa
IIDepartment of Surgery, Kimberley Hospital Complex, South Africa
SUMMARY
A 38-year female with no prior medical or surgical history presented with pleuritic pain and respiratory distress. Imaging revealed a right diaphragmatic hernia with colonic content. At right anterolateral thoracotomy, a diaphragmatic hernia containing a perforated right hemi-colon was found. The colon was resected in the chest and continuity restored via a laparotomy. This case illustrates the risk of obstruction, ischaemia and perforation and highlights the importance of early identification and prompt surgical management to reduce morbidity and mortality.
Keywords: right-sided, atraumatic diaphragmatic hernia, perforated right hemi-colon
Case report
A 38-year female with no known medical comorbidities or surgical history presented to the emergency room with a 3-day history of pleuritic chest pain with accompanying constipation. She denied history of blunt or penetrating trauma or previous presentation to medical institution. Examination revealed a lean patient in respiratory distress with decreased air entry on the right hemithorax with intra-thoracic bowel sounds audible, suggesting a right-sided diaphragmatic hernia, which was confirmed on an erect chest radiograph (Figure 1). Abdominal examination revealed localised right upper quadrant tenderness without peritonism. Due to her relative haemodynamic stability at the time, and lack of known history of trauma, a contrasted CT thorax/abdomen was requested to facilitate elective surgical planning and to exclude an alternate diagnosis (Figure 2).

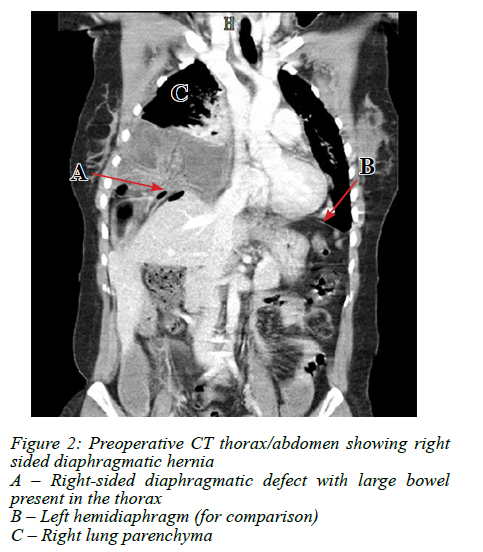
Haematological investigations showed a white cell count (WCC) of 13.7 x 109. The CT confirmed a right-sided diaphragmatic defect with large bowel present in the thorax, with no intra-abdominal fluid collections. At that stage, the patient had a sudden decompensation cardiorespiratory collapse and was taken immediately to theatre, where a right anterolateral thoracotomy was performed, revealing a perforated right hemi-colon with feculent contamination of the thorax, entering through a 5 x 3 cm medial defect in the diaphragm. A right hemicolectomy was performed with extensive washout of the thorax, the stapled ends reduced into the abdominal cavity and the chest was drained and closed. The patient stabilised haemodynamically and an exploratory laparotomy was then performed to restore bowel continuity in an uncontaminated field. The diaphragmatic defect was closed without tension by direct suture.
After a brief intensive care unit stay for ventilatory support, the patient was discharged to the ward where the intercostal drain was removed, and a chest radiograph revealed no residual effusion. She developed a surgical site infection which was treated nonoperatively for 2 weeks, after which she was discharged. She was in good health when reviewed at 3 months in the surgical clinic.
Discussion
Atraumatic diaphragmatic hernias are virtually unheard of in the adult population, with left-sided hernias being more common than right.1 The most common aetiology of diaphragmatic hernias is thought to be trauma secondary to penetrating or blunt force, followed by congenital malformations of the diaphragm.2 Other possible causes include a pseudopneumoperitoneum, such as Chilaiditi's syndrome, whereby colon is interposed between the superior surface of the liver and inferior surface of the right hemidiaphragm, giving the impression of free intraabdominal air similar to that seen in Figure 1. Other relevant causes of pseudopneumoperitoneum to this case include basal linear atelectasis, or a pseudo-Rigler sign from intra-abdominal fat.3 Described in this case report is an uncommon, right-sided atraumatic diaphragmatic hernia, confirmed with preoperative imaging and intraoperative findings, with the suspected aetiology for this case as an undiagnosed congenital diaphragmatic weakening with rupture secondarily to increased intra-abdominal pressure.4,5
In contrast, traumatic diaphragmatic hernias are far more common than their atraumatic counterparts, with an incidence of between 3.4% and 47%;6 it is noted, however, that between 7-26% of these patients may be undiagnosed or unaware or a prior traumatic event. Pathogenesis is thought to broadly consist of an acute phase of trauma, where a negative intra-thoracic and positive intra-abdominal pressure causes the relocation of abdominal contents into the thoracic cavity via a newly created defect in the diaphragm, a latent phase of recovery from the insult and an obstructive phase, where incarcerated contents may become ischaemic and perforated.6
Minimally invasive or open transabdominal and thoracic approaches have been used alone or in combination to dissect and resect the hernia sac, reduce and or resect the contents, and assure a tension-free closure of the defect, with or without a mesh.5,6
In this case, the initial surgical approach was an antero-lateral thoracotomy, where resection was performed. The bowel was then reduced into the uncontaminated abdominal cavity anastomosed, and the diaphragmatic defect repaired. In an acute traumatic event resulting in intra-abdominal organs herniating intra-thoracically, a laparotomy is acceptable, especially where associated abdominal injuries may exist, but a thoracotomy or even a combined set of incisions has been described to good effect in older injuries.7,8 The debate as to whether to perform a primary anastomosis or an ileostomy, with mucous fistula omnipresent, with the factors of intraoperative contamination, infection, the use of blood products and vasopressors favouring diversion.9,10 It should be noted, however, that the surgical decision-making must take into consideration the morbidity and mortality associated with stoma reversal as well as the social, physical and sexual side effects of an ileostomy fashioned without precounselling.11,12
Irrespective of aetiology, diagnostic dilemmas are common and a high index of suspicion should be maintained for diaphragmatic hernias as misdiagnosis; resulting death can easily occur as a result of clinical and radiological misinterpretation. In cases of haemodynamic stability, a case could be made for further investigation to allow for surgical planning and to exclude differential diagnoses. However, the interval between radiology and theatre should be kept as short as possible to minimise risk of ischaemia and perforation hence avoiding the associated morbidity and mortality.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Ethical approval was obtained from Stellenbosch University HREC Reference No: C20/06/015.
ORCID
Ν Allopi https://orcid.org/0000-0002-1343-302X
Μ Wellmann https://orcid.org/0000-0002-5787-6789
VR Blanco https://orcid.org/0000-0001-8993-1925
REFERENCES
1. Kurt A, Yazicioglu KR, Ipek A, Tosun Ö, Coçkun M. Right sided diaphragmatic hernia in an adult without history of trauma: unusual CT findings. Eur J Gen Med. 2004;1(3):55-57. https://doi.org/10.29333/ejgm/82213. [ Links ]
2. Mar Fan MJ, Coulson ML, Siu SK. Adult incarcerated right-sided Bochdalek hernia. Aust N Z J Surg. 1999;69(3):239-41. https://doi.org/10.1046/j.1440-1622.1999.01538.x. [ Links ]
3. Jones J, Bell D. Pseudopneumoperitoneum. 2009. Available from: https://radiopaedia.org/articles/pseudopneumoperitoneum?lang=us. [ Links ]
4. Thomas S, Kapur B. Adult Bochdalek hernia - clinical features, management and results of treatment. Jpn J Surg. 1991;21(1):114-9. https://doi.org/10.1007/BF02470876. [ Links ]
5. Faridi SH, Rizvi AA, Siddiqui B, Khalid M. Late post traumatic right-sided diaphragmatic hernia presenting with acute intestinal obstruction and strangulation: a rare presentation. Oman Med J. 2013;28(1):e041. https://doi.org/10.5001/omj.2013.21. [ Links ]
6. Filosso PL, Guerrera F, Sandri A, et al. Surgical management of chronic diaphragmatic hernias. J Thorac Dis. 2019;11(Suppl 2):S177-85. https://doi.org/10.21037/jtd.2019.01.54. [ Links ]
7. Ahmad Ganie F, Nabi Lone G, Chowdhary M, Lone H. The characteristics and surgical approach in post-traumatic diaphragmatic hernia: a single centre experience. Bull Emerg Trauma. 2013;1(3):108-111. [ Links ]
8. Deng X, Deng Z, Huang E. Surgical management of traumatic diaphragmatic hernia - a single institutional experience of more than two decades. BMC Surg. 2021;21(1):142. https://doi.org/10.1186/s12893-021-01141-2. [ Links ]
9. Sultan R, Chawla T, Zaidi M. Factors affecting anastomotic leak after colorectal anastomosis in patients without protective stoma in tertiary care hospital. J Pak Med Assoc. 2014;64(2):166-70. [ Links ]
10. McDermott FD, Heeney A, Kelly ME, et al. Systematic review of preoperative, intra-operative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg. 2015;102(5):462-79. https://doi.org/10.1002/bjs.9697. [ Links ]
11. Berne JD, Velmahos GC, Chan LS, Asensio JA, Demetriades D. The high morbidity of colostomy closure after trauma -further support for the primary repair of colon injuries. Surgery. 1998;123(2):157-64. https://doi.org/10.1016/S0039-6060(98)70253-3. [ Links ]
12. De Campos K, Benites Bot LH, Petroianu A, et al. The impact of colostomy on the patient's life; impacto da colostomia na vida de seus portadores. J Coloproctol. 2017;37(3):205-10. https://doi.org/10.1016/jjcol.2017.03.004. [ Links ]
 Correspondence:
Correspondence:
email: nabeelallopi@gmail.com














