Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.4 Cape Town Dec. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3774
CASE REPORT
Orbital metastases of breast carcinoma
C Pretorius; M Kemp
George Regional Hospital, South Africa
SUMMARY
Orbital metastases, although rare, originate from systemic breast cancer in up to 35% of patients. Metastases more commonly arise from invasive lobular carcinomas than from invasive ductal carcinomas. Due to the diagnostic challenge of determining the primary site for the metastases, immunohistochemistry is essential. Clinical and radiological information are usually insufficient. This disease typically progresses quickly and has a poor prognosis. We report the case of a 55-year-old female who presented in 2017 with a left breast carcinoma and defaulted treatment during many different stages, then returned three years later with a right orbital mass which was confirmed to be a breast cancer metastasis on biopsy.
Keywords: metastatic breast cancer, orbital metastases
Case report
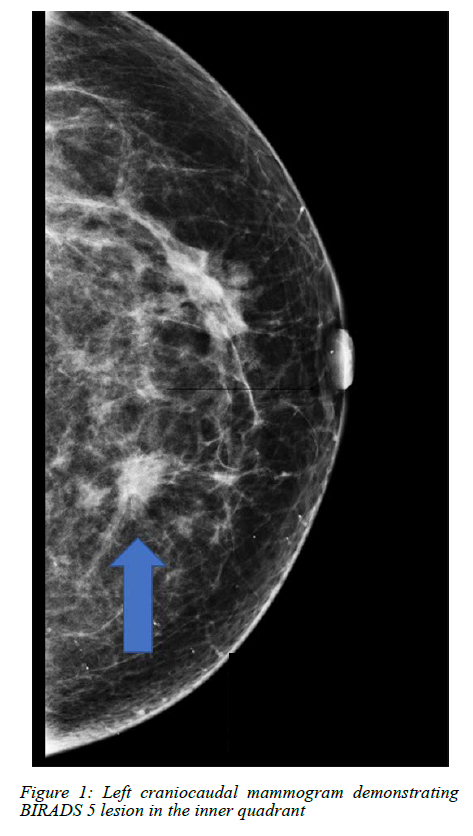
A 55-year-old post-menopausal female presented to George Regional Hospital in 2017 with a sinister left breast mass, suggestive of a cT4aN2 breast cancer. She had no family history of breast cancer and was not using hormone replacement therapy. Mammography demonstrated a Breast Imaging-Reporting and Data System (BIRADS) 5 lesion (Figure 1) in the left breast (> 95% probability of malignancy) which was biopsied under ultrasound guidance confirming an infiltrating ductal carcinoma. The biomarkers were oestrogen receptor (ER) positive (Allred score 7/8), progesterone receptor (PR) positive (Allred score 6/8) and human epidermal growth factor receptor 2 (HER2-neu) 2+positive. Gene amplification was performed to ascertain the true status of the HER2-neu receptor which was negative. No staging examinations were done at this stage.
She defaulted treatment and re-presented in November 2019 at which stage she was referred to oncology for neoadjuvant chemotherapy. She was restaged as T4cN2M0. Due to an adverse reaction to paclitaxel, she defaulted systemic treatment in December 2019.
A left modified radical mastectomy and axillary clearance was performed in March 2020, three months after defaulting neoadjuvant chemotherapy.
Histology demonstrated extensive invasive carcinoma of no special type which had invaded the left pectoralis muscle. Six out of eight lymph nodes removed demonstrated metastatic disease and there was only a partial treatment response to neoadjuvant chemotherapy. The E-cadherin was positive, confirming ductal origin of the tumour and the immunohistochemistry demonstrated strong oestrogen receptor positivity (Allred score 6/8). Both the progesterone and HER2-neu receptors were negative. She was started on oral chemotherapy and had left chest-wall radiation.
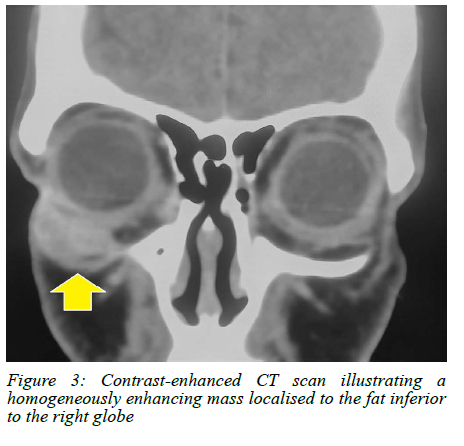
In May 2020, she presented to the ophthalmology department with a painless, fixed right inferolateral orbital rim mass (Figure 2). There was no sign of locoregional breast cancer recurrence. She was referred for a contrast enhanced computed tomography (CT) scan of the brain and orbits. The CT scan (Figure 3) of the right orbit demonstrated a homogeneously enhancing mass localised to the fat inferior to the right globe. The mass extended into the extraconal space along fascial planes but did not invade the rectus muscles or globe.
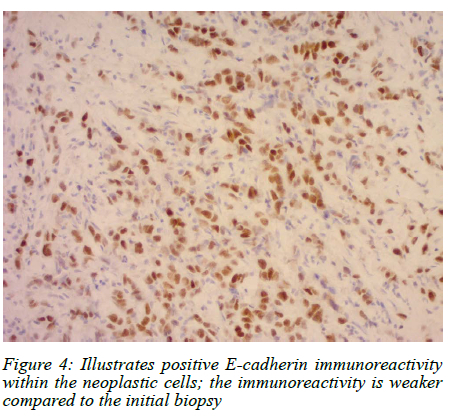
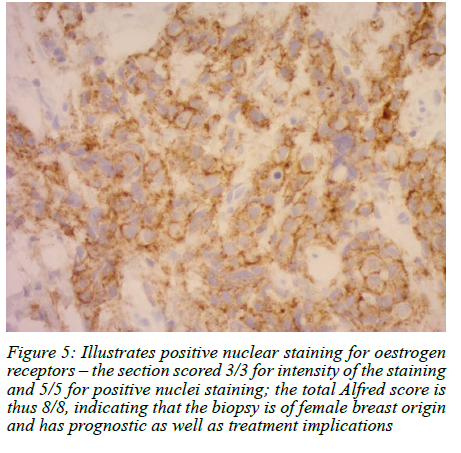
Excision biopsy of this mass demonstrated metastatic disease. The immunohistochemistry favoured a breast origin with a positive E-cadherin stain (Figure 4) and strong ER positivity (Allred score 8/8) (Figure 5), PR positivity (Allred score 6/8) and a HER2 1+ score (negative). She was restaged with a chest X-ray, liver ultrasound and nuclear medicine bone scan.
Bleomycin injections were commenced by ophthalmology in conjunction with her oncology management, which consisted of palliative systemic treatment in the form of arimidex. Unfortunately, she had a poor response to the palliative endocrine treatment and presented in November 2020 with a bony metastasis to the left tibia on X-rays.
She was then again lost to follow-up.
In March 2021, she presented with sudden onset of bilateral lower limb paralysis and CT scan confirmed extensive spinal metastases.
Discussion
Orbital metastasis (OM) is a rare finding in systemic cancer, with few case reports and less frequent elucidation of the primary tumour.1-3 Histologically confirmed OM are diagnosed once or twice at larger academic centres per year and most of the literature is from single case reports.2
Breast carcinoma is the most likely primary tumour, accounting for 29-35% of all tumours in the orbit.4 In a series by Raap et al., just over 25% of patients with breast carcinoma and OM, presented initially with OM.4
Other primary sites, in order of metastatic sequence, include lung, prostate, kidney, melanoma, gastrointestinal tumours and hepatocellular carcinoma.2,5 It is often difficult to make the diagnosis of an OM and elucidate the primary site clinically and radiologically; therefore, histopathology with immunohistochemistry is essential.2
Invasive lobular carcinoma is more likely to cause OM than invasive ductal carcinoma.35 The hypothesis is that there is a higher amount of oestrogen produced by the eye, which leads to a greater prediction of ILC to metastasise to the orbit. Blohmer et al. also demonstrated that there are a considerable number of patients with bilateral OM secondary to invasive lobular carcinoma.1 In our patient, the excision biopsy from the right orbital tumour demonstrated a similar morphology to the mastectomy specimen, which revealed invasive carcinoma of no special type. However, the E-cadherin staining was less strong and crisp than the internal control and compared to that of the mastectomy specimen. The tumour may have been a pleomorphic variant of invasive lobular carcinoma as 10% of invasive lobular carcinomas demonstrate retained E-cadherin staining.6 It is not possible to evolve from invasive carcinoma of no special type into an invasive lobular carcinoma. The rapid clinical progression is also in keeping with OM from breast carcinoma.7
Cross-sectional imaging, especially magnetic resonance imaging (MRI), is valuable in characterising and determining the extent of disease which then supplements the ophthalmological findings and diagnosis.3,7 Critical infor-mation includes which intra-orbital structures are involved, perineural spread and intracranial extension.7 CT is less sensitive than MRI.1,3 However, differentiating nonneoplastic orbital infiltrating processes such as sarcoidosis from OM often poses a diagnostic challenge.7 It may be difficult on imaging to determine the principle orbital tissue site as the disease may have markedly infiltrated surrounding tissues.7 OM from breast carcinoma are diffuse with irregular growth along rectus muscles and fascial planes and form ill-defined orbital massess.1,2,8 In our patient, the CT scan of the right orbit demonstrated a well-defined enhancing mass with growth along the fat and fascial planes, which did not extend along the rectus muscles.
OM may be diagnosed incidentally initially by PET CT.9 PET CT can also assist in detecting the primary tumour and other metastases.9
OM secondary to breast carcinoma do not occur in isolation. Bone and the central nervous system are the most common other metastatic sites in these patients1,3 Our patient presented with extensive metastases to the spine. Treatment options are all palliative as OM occurs as part of disseminated disease.4 These include surgical resection, local irradiation, chemotherapy or endocrine therapy.4
OM from breast carcinoma is characterised by very rapid progression and a poor prognosis. The average survival is 31 months after presentation.4 The outcome in our patient is not known as she was lost to follow-up.
Ethical approval
Ethics approval was obtained from the George Hospital Ethics Committee on 24 February 2021.
REFERENCES
1. Blohmer M, Zhu L, Atkinson JM, et al. Patient treatment and outcome after breast cancer orbital and periorbital metastases: a comprehensive case series including analysis of lobular versus ductal tumour histology. Breast Cancer Res. 2020;22(1):70. https://doi.org/10.1186/s13058-020-01309-3. [ Links ]
2. El Bakraoui K, El Morabit B. Orbital metastasis from triple-negative breast cancer: case report and literature review. Case Rep Oncol. 2020;13(2):1042-6. https://doi.org/10.1159/000509348. [ Links ]
3. Framarino-Dei-Malatesta M, Chiarito A, Bianciardi F, et al. Metastases to extraocular muscles from breast cancer: case report and up-to-date review of the literature. BMC Cancer. 2019;19(1):36. https://doi.org/10.1186/s12885-018-5253-1. [ Links ]
4. Raap M, Antonopoulos W, Dämmrich M, et al. High frequency of lobular breast cancer in distant metastases to the orbit. Cancer Med. 2015;4(1):104-11. https://doi.org/10.1002/cam4.331. [ Links ]
5. Goldberg R, Rootman J, Cline R. Tumours metastatic to the orbit: a changing picture. Surv Ophthalmol. 1990;35(1):1-24. https://doi.org/10.1016/0039-6257(90)90045-W. [ Links ]
6. Grabenstetter A, Mohanty AS, Rana S, et al. E-cadherin immunohistochemical expression in invasive lobular carcinoma of the breast: correlation with morphology and CDH1 somatic alterations. Hum Pathol. 2020;102:44-53. https://doi.org/10.1016/j.humpath.2020.06.002. [ Links ]
7. Tailor T, Gupta D, Dalley DR, Roberts W, Keene CD. Orbital neoplasms in adults: clinical, radiologic, and pathologic review. Radiographics. 2013;33(6):1739-58. https://doi.org/10.1148/rg.336135502. [ Links ]
8. Khan SN, Sepahdari AR. Orbital masses: CT and MRI of common vascular lesions, benign tumours, and malignancies. Saudi J Ophthalmol. 2012;26(4):373-83. https://doi.org/10.1016/j.sjopt.2012.08.001. [ Links ]
9. Solav S, Bhandari R, Sowani A. Choroidal metastasis from carcinoma of breast detected on F18-FDG PET CT scan: a case report and review of literature. Indian J Nucl Med. 2010;25(4):160-3. https://doi.org/10.4103/0972-3919.78252. [ Links ]
 Correspondence:
Correspondence:
email: chane.pretorious@gmail.com














