Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.60 no.4 Cape Town Dez. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3735
CARDIOTHORACIC SURGERY
Mediastinoscopy as a diagnostic tool in a South African tertiary hospital
CKP Ofoegbu; N Swai; A Moodley; R Manganyi
Chris Barnard Division of Cardiothoracic Surgery, Groote Schuur Hospital, South Africa
ABSTRACT
BACKGROUND: Mediastinoscopy is an effective and safe diagnostic tool for anterior mediastinal lesions. The study was done to assess the usefulness of mediastinoscopy as a diagnostic modality for mediastinal lesions.
METHODS: A retrospective study of patients who had mediastinoscopy over 12 years at the Groote Schuur Hospital, Cape Town. Preoperative data, intraoperative and postoperative data were collected.
RESULTS: The records of 115 patients were reviewed. Male to female ratio was 1.4:1 with a mean age of 48.5 (± 16.8) years. Preoperative computerised tomography (CT) scan was done in 98.3%. The most common indications for mediastinoscopy were mediastinal lymphadenopathy (87.8%) and anterior mediastinal mass (12.2%). Prior endobronchial ultrasound (EBUS) biopsy was done in 11.3%. All the patients had conventional cervical mediastinoscopy. Lung cancer staging accounted for 16.5% of the procedures. A biopsy was successfully done in 103 patients (89.6%). The most common lymph node station biopsied was 2R (55.7% of 76 patients), though the information on stations biopsied could not be ascertained in 25.2% of patients. The complication rate was 1.7 % (suprasternal haematoma and brachiocephalic artery injury). Histopathologic diagnoses were obtained in 89.5% (103/115 patients). Benign diagnoses accounted for 72.8% (75), while malignant diagnoses were 27.2% (28). Intensive care unit (ICU) stay and mechanical ventilation were required in 5% and 2.5% of patients, respectively. The median postoperative hospital stay was 2 days. There were no postoperative deaths. The median follow-up period was 14 days.
CONCLUSION: Mediastinoscopy's diagnostic role is assured, still required and is safe with minimal morbidity and no mortality.
Keywords: mediastinoscopy, mediastinal lymph nodes, mediastinal mass
Introduction
Mediastinoscopy is a surgical procedure that entails endoscopic visualisation of the superior and middle mediastinum. It was first described by Carlens in 1959 and involved insertion of a laryngoscope through a supraclavicular incision with biopsies of lymph nodes done.1 It is mainly used for staging of lung cancer by assessing the N2 nodes and also for diagnosis of other mediastinal masses.2
Mediastinoscopy is important for preoperative evaluation of the mediastinum with the added advantage of tissue diagnosis and staging in lung cancer and subsequently ensuring appropriate therapy.3 The procedure can access the mediastinal lymph node groups, proximal hilar lymph nodes and the most superior/anterior portions of subcarinal lymphadenopathy.
Mediastinoscopy is also useful for the diagnosis of other mediastinal lesions apart from lung cancer, including tuberculosis, lymphoma, Hodgkin's disease, sarcoidosis, histoplasmosis and coccidioidomycosis.4
The recent emergence of endobronchial ultrasound fine-needle aspiration (EBUS-FNA) as a possible replacement of mediastinoscopy has also been proposed.5
Mediastinoscopy may become necessary if a definitive result is not obtained by EBUS-FNA, especially where there are enlarged mediastinal lymph nodes.3
The non-invasive imaging modalities including chest computerised tomography (chest CT) and positron emission tomography/computer tomography (PET/CT) are limited by high false positive and false negative rates. The quoted sensitivity/specificity for chest CT and PET/CT were 55/81% and 62/90% respectively.5 Even so, positive results by these non-invasive modalities sometimes require tissue confirmation by invasive techniques.
The conventional mediastinoscopy (CM) involves the creation of a suprasternal incision (1-2 cm above the supra-sternal notch) with dissection down to the pre-tracheal fascia and further dissection in that plane to gain access to structures in the anterosuperior mediastinum.6 In the past few years, the video-assisted mediastinoscopy (VAM) has been introduced. Its advantages are said to be enhanced magnification, improved identification of anatomical structures, simplified teaching and documentation, the ability for the surgeon to operate bimanually and a more comfortable surgical working environment.7-9
The complications of mediastinoscopy may include major vascular injury (brachiocephalic, aortic arch), recurrent laryngeal nerve paralysis, pneumothorax, tracheal or oesophageal injury and wound infection.410
Conventional mediastinoscopy is a safe procedure with reported morbidity and mortality rates of (0-5.3%) and 0-0.05% respectively,4,712 and accuracy rates of 83.8-97.2% and negative predictive value (NPV) of 81-95.7%.8·9·11 The morbidity and mortality rates for VAM are 0.83-2.9% and 0% respectively.8,911
The aim of this study was to ascertain the role of mediastinoscopy in the diagnosis of mediastinal lesions and the accuracy of mediastinoscopy diagnosis.
Patients and methods
Study design
The study was a retrospective study performed in a cohort of patients who underwent mediastinoscopy at the Groote Schuur Hospital over 12 years (January 2006-December 2018).
Characteristics of the study population Inclusion criteria were all patients who had cervical medi-astinoscopy as a surgical procedure and were older than 13 years. There were no exclusion criteria.
Recruitment and enrolment
The patients were enrolled from the hospital records (folders, theatre records). The data collected included preoperative data (demographics, comorbidities, previous diagnostic procedures and radiology findings), intraoperative data (indications for mediastinoscopy, cadre of surgeon, success of lesion biopsy and lymph node stations biopsied) and postoperative data (complications, duration of ICU stay/ mechanical ventilation and histology of mediastinoscopy biopsy).
Data analysis
All data was analysed with Stata 14 statistical software. The normality of data distribution was assessed with the Shapiro-Wilk test. Continuous variables were expressed as ranges, median, means and standard deviation (SD). The student's t-test was used for 2-group comparisons of normally distributed continuous variables. The non-parametric data was analysed with the Mann-Whitney U test and 95% confidence intervals (CIs) expressed. Categorical variables were analysed with Pearson's chi-squared test and Fisher's exact test when the variables were less than 5. The sensitivity, specificity, positive predictive value (PPV) and NPV were calculated.
The diagnostic accuracy, specificity and NPV of medi-astinoscopy for lung cancer staging was assessed by the final pathologic results obtained from mediastinal lymph node sampling/dissection performed during thoracotomy and lung resection.
A _p-value of < 0.05 was set as statistical significance.
Results
The records of 115 patients were reviewed. The mean age of these patients was 48.5 years (± 16.8), and 48 patients were females (41.7%). The indication for mediastinoscopy was mainly for mediastinal lymphadenopathy (101, 88%). Some of the patients had undergone a previous endobronchial ultrasound (EBUS) guided transbronchial biopsy (12, 10.4%). The mean preoperative haemoglobin (Hb), international normalised ratio (INR) and creatinine (Cr, μm/L.) were 12.3 ± 2.4 g/L, 1.15 ± 0.17 and 75 ± 22.6 μm/L, respectively. Table I depicts the preoperative data.

Most of the patients had a concomitant procedure with a successful lesion biopsy done in 103 patients (89.6%). The lymph node station biopsied was available for 77 patients, and 61 (79.2%) of these were single-station biopsies. There was no statistical difference in the yield between single- or multi-station biopsy (p = 0.895). There was no statistical difference in the successful lesion biopsy between consultants and trainees (p = 0.378). Table I depicts the intraoperative data.
The intensive care unit (ICU) stay and mechanical ventilation rate were 5% (4 patients) and 2.5% (2 patients) respectively. The morbidity (suprasternal haematoma and brachiocephalic artery injury) and mortality rates in the study were 1.7% (2 patients) and 0% respectively. The median duration of hospital stay was 2 days.
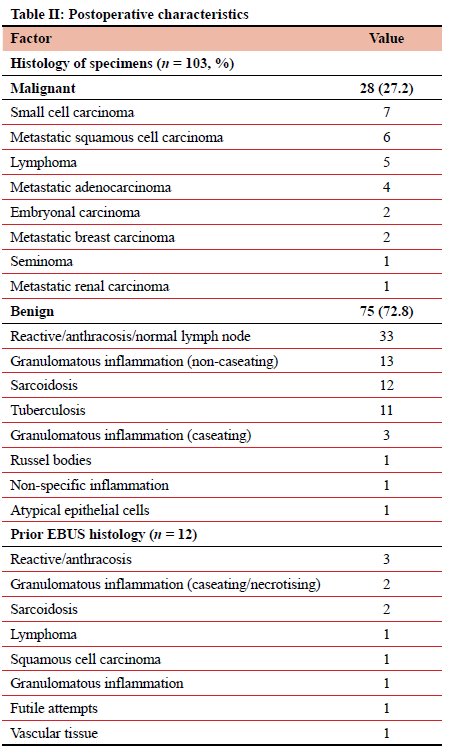
Histopathological results were obtained in 103 patients (89.6%) and were mainly benign diagnoses with reactive/ normal lymph node (33), granulomatous inflammation-non-caseating (13), sarcoidosis (12) and tuberculosis (11) being the major diagnoses. Table II depicts the histopathological diagnoses obtained from the biopsies.
Fifteen patients (13%) had lung resections following mediastinoscopy, and two of these had metastatic N2 disease found during lung resection, thereby giving a false negative rate, specificity and NPV of 13.3%, 100% and 86% respectively. Table III depicts this.
The patients who had prior negative/inconclusive EBUS results had a positive mediastinoscopy result in 83% (10/12 patients).
Discussion
Mediastinoscopy has always played a role in the diagnosis of mediastinal lymphadenopathy from several aetiologies, including benign (sarcoidosis, tuberculosis) and malignant diseases (lung cancer, metastases). It has also been very useful for lung cancer staging and diagnosis of anterior mediastinal masses. In rarer circumstances, mediastinoscopy has been used in trauma, e.g., retrieval of a bullet in the mediastinum.13
Though diagnosis of mediastinal lesions can be made non-invasively, viz a viz CT chest and PET scan, the occasional necessity for tissue diagnosis may be fulfilled by EBUS, which in recent years has served as a viable alternative to mediastinoscopy for obtaining mediastinal tissue diagnosis. There is evidence that EBUS is at least as sensitive as mediastinoscopy in detection of N2 disease.14 However, there are situations where a negative EBUS result is remedied by mediastinoscopy. There has been evidence found in patients with non-small cell lung cancer with an indication for mediastinal staging where an initial negative result from EBUS had a mediastinoscopy and subsequently reduced the number of futile thoracotomies by 50%.15 One study of lung cancer patients showed a mean of 8.8 patients had to undergo an additional mediastinoscopy to find one false negative result of EBUS and EUS-FNA, but when only patients with suspicious mediastinal lymph nodes on FDG-PET are assessed, the number needed to treat (NNT) is reduced to 6.1 patients;15 they further stated that in a case with high probability of mediastinal lymph node metastasis based on imaging and negative EBUS, mediastinoscopy should be done even when the EBUS/EUS-FNA aspirate is representative. Our finding of 10.4% is much less than 18.3% found in another study.16 In our study, the diagnostic yield of 83% was found. This confirms a role for mediastinoscopy in our environment.
Mediastinoscopy has long possessed an excellent safety profile with very low morbidity and mortality rates. The major complications that may bedevil mediastinoscopy include major vascular injury (brachiocephalic artery, azygos vein, pulmonary artery).14 A patient in our cohort sustained brachiocephalic artery injury and needed a median sternotomy for control and repair of the artery. Other complications may include pneumothorax, recurrent laryngeal nerve injury and oesophageal perforation. One study found the most common complication to be recurrent laryngeal nerve injury,11 a finding not seen from this study. The low morbidity (1.7%) and mortality (0%) rates found in our study are similar to 0-3.1% and 0-0.05% found by other authors.2,4,8,11,17,18 Authors have posited that mediastinoscopy should have a morbidity of < 1% and mortality of about 1 in 2 000 when performed regularly.17 Some authors have even leveraged upon the excellent safety profile to attempt mediastinoscopy in the presence of superior vena cava syndrome.19
The procedure has a high efficacy rate for mediastinal tissue diagnosis. Our value of 89.5% compares favourably with those of84-98.6 °% by other authors.2,4,6,7,20 Other studies also showed that most diagnoses from mediastinoscopy were benign (17-81.8%);4,6,21,22 a similar finding was seen in our study (72.8%). For these patients with benign diagnoses, mediastinoscopy may avoid the need for further investigation. Some studies have, however, shown a higher rate of malignant diagnoses (64-81%),4,7 which may be a reflection of the local disease and referral patterns.
The appropriate management and determination of prognosis of lung cancer require accurate staging, especially the determination of involvement of N2 lymph nodes. Our study cohort showed referral for lung cancer staging was 16.5% of all mediastinoscopies done. The role of mediastinoscopy in staging for lung cancer with respect to N2 nodes was confirmed in this study. Our false negative rate was 13.3%, which is much higher than 4.2% reported by Cho et al.11 It is noted that their study sample for only staging mediastinoscopy was 522 (compared to 115 in our study).11 Our specificity and NPV rates of 100% and 86% compare favourably with other authors quoting NPV rates of 90-95%.111415 These rates were calculated from results of lymph nodes within the reach of the mediastinoscopy (2R, 4R, 2L, 4L, 7). It must, however, be noted that the EBUS expertise in other climes has advanced to the point that EBUS has completely replaced mediastinoscopy for mediastinal lymph node (N2) staging in lung cancer.23
The limitations of our study include some loss of pertinent information (number of lymph nodes biopsied, lymph node stations biopsied) associated with retrospective studies. Secondly, our study was performed in a single institution with a single surgical group, which may bias the operative data. Thirdly, our study did not analyse all the mediastinal lymph nodes, but was limited to stations 2R, 4R, 2L, 4L and 7.
In conclusion, mediastinoscopy is safe, accurate in the provision of a confirmatory diagnosis and still relevant in invasive staging for lung cancer in our environment.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
The study was approved by the University of Cape Town Human Research Ethics Committee (UCTHREC-263/2017).
ORCID
CKP Ofoegbu https://orcid.org/0000-0002-7873-1976
Ν Swai https://orcid.org/0000-0003-3902-933X
A Moodley https://orcid.org/0000-0002-4312-2994
R Manganyi https://orcid.org/0000-0002-0135-9408
REFERENCES
1. Carlens E. Mediastinoscopy: a method for inspection and tissue biopsy in the superior mediastinum. Dis Chest. 1959;36(4):343-52. https://doi.org/10.1378/chest.36A343. [ Links ]
2. Chauhan A KS, Ganguly M, Nath P. Cervical mediastinoscopy: re-evaluation of an old technique in era of new imaging technology. Indian J Chest Dis Allied Sci. 2012;54:169-74. [ Links ]
3. Detterbeck FC, Jantz MA, Wallace M, Vansteenkiste J, Silvestri GA. Invasive mediastinal staging of lung cancer: ACCP evidence-based clinical practice guidelines. 2nd ed. Chest. 2007;132(3 Suppl):S202-20. https://doi.org/10.1378/chest.07-1362. [ Links ]
4. Hammoud ZT, Anderson RC, Meyers BF, et al. The current role of mediastinoscopy in the evaluation of thoracic disease. J Thorac Cardiovasc Surg. 1999;118:894-9. https://doi.org/10.1016/S0022-5223(99)70059-0. [ Links ]
5. Um SW, Kim HK, Jung SH, et al. Endobronchial ultrasound versus mediastinoscopy for mediastinal nodal staging of non-small-cell lung cancer. J Thorac Oncol. 2015;10(2):331-7. https://doi.org/10.1097/JTO.0000000000000388. [ Links ]
6. Eldaboosy SAM, Zeinnhom RA, Kanany H, Nour MO. The value of cervical mediastinoscopy in the diagnosis of mediastinal lesions. Egypt J Chest Dis Tuberc. 2015;64(3):755-60. https://doi.org/10.1016/j.ejcdt.2015.03.030. [ Links ]
7. Venissac N, Alifano M, Mouroux J. Video-assisted mediastinoscopy: experience from 240 consecutive cases. Ann Thorac Surg. 2003;76(1):208-12. https://doi.org/10.1016/S0003-4975(03)00164-4. [ Links ]
8. Anraku M, Miyata R, Compeau C, Shargall Y. Videoassisted mediastinoscopy compared with conventional mediastinoscopy: are we doing better? Ann Thorac Surg. 2010;89(5):1577-81. https://doi.org/10.1016/j.athoracsur.2010.02.012. [ Links ]
9. Leschber G, Sperling D, Klemm W, Merk J. Does video-mediastinoscopy improve the results of conventional mediastinoscopy? Eur J Cardiothorac Surg. 2008;33(2):289-93. https://doi.org/10.1016/j.ejcts.2007.10.021. [ Links ]
10. Puhakka HJ. Complications of mediastinoscopy. J Laryngol Otol. 1989;103(3):312-5. https://doi.org/10.1017/S0022215100108795. [ Links ]
11. Cho JH, Kim J, Kim K, et al. A comparative analysis of videoassisted mediastinoscopy and conventional mediastinoscopy. Ann Thorac Surg. 2011;92(3):1007-11. https://doi.org/10.1016/j.athoracsur.2011.02.032. [ Links ]
12. Karfis EA, Roustanis E, Beis J, Kakadellis J. Video-assisted cervical mediastinoscopy: our seven-year experience. Interact CardiovascThoracSurg. 2008;7(6):1015-8.https://doi.org/10.1510/icvts.2008.178111. [ Links ]
13. Bulut T, Brutel de la Riviere A. Mediastinoscopy as a therapeutic tool. Ann Thorac Surg. 2011;91(5):1616-8. https://doi.org/10.1016/j.athoracsur.2010.10.055. [ Links ]
14. Block MI, Tarrazzi FA. Invasive mediastinal staging: endobronchial ultrasound, endoscopic ultrasound, and medi-astinoscopy. Semin Thorac Cardiovasc Surg. 2013;25(3):218-27. https://doi.org/10.1053/j.semtcvs.2013.10.001. [ Links ]
15. Verhagen AF, Schuurbiers OCJ, Looijen-Salamon MG, et al. Mediastinal staging in daily practice: endosonography, followed by cervical mediastinoscopy. Do we really need both? Interact Cardiovasc Thorac Surg. 2013;17(5):823-8. https://doi.org/10.1093/icvts/ivt302. [ Links ]
16. Andrade RS, Podgaetz E, Rueth NM, et al. Endobronchial ultrasonography versus mediastinoscopy: a single-institution cost analysis and waste comparison. Ann Thorac Surg. 2014;98(3):1003-7. https://doi.org/10.1016/j.athoracsur.2014.04.104. [ Links ]
17. Lemaire A, Nikolic I, Petersen T, et al. Nine-year single center experience with cervical mediastinoscopy - complications and false negative rate. Ann Thorac Surg. 2006;82(4):1185-9. https://doi.org/10.1016/j.athoracsur.2006.05.023. [ Links ]
18. Onat S, Ates G, Avci A, et al. The role of mediastinoscopy in the diagnosis of non-lung cancer diseases. Ther Clin Risk Manag. 2017;13:939-43. https://doi.org/10.2147/TCRM.S144393. [ Links ]
19. Dosios T, Theakos N, Chatziantoniou C. Cervical medi-astinoscopy and anterior mediastinotomy in superior vena cava obstruction. Chest. 2005;128(3):1551-6. https://doi.org/10.1378/chest.128.3.1551. [ Links ]
20. Hujala KT, Sipila JI, Grenman R. Mediastinoscopy - its role and value today in the differential diagnosis of mediastinal pathology. Acta Oncol. 2001;40(1):79-82. https://doi.org/10.1080/028418601750071109. [ Links ]
21. Porte H, Roumilhac D, Eraldi L, et al. The role of medi-astinoscopy in the diagnosis of mediastinal lymphadenopathy. Eur J Cardiothorac Surg. 1998;13(2):196-9. https://doi.org/10.1016/S1010-7940(97)00324-2. [ Links ]
22. Graeter TP, Hellwig D, Hoffmann K, et al. Mediastinal lymph node staging in suspected lung cancer: comparison of positron emission tomography with F-18-fluorodeoxyglucose and mediastinoscopy. Ann Thorac Surg. 2003;75(1):231-6. https://doi.org/10.1016/S0003-4975(02)04350-3. [ Links ]
23. Visser MPJ, Van Grimbergen I, Holters J, et al. Performance insights of endobronchial ultrasonography (EBUS) and mediastinoscopy for mediastinal lymph node staging in lung cancer. Lung Cancer. 2021;156:122-8. https://doi.org/10.1016/j.lungcan.2021.04.003. [ Links ]
 Correspondence:
Correspondence:
email: chimaofu@yahoo.com














