Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.4 Cape Town Dec. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3794
TRAUMA
The neglected epidemic of trauma from interpersonal violence against the elderly in South Africa
B LeeI; VY KongII; C CheungIV, V; N RajaretnamVI; V ThirayanVII; JL BruceIII; V ManchevIII; RP MillsVIII; GL LaingIII; DL ClarkeIII
IDepartment of Surgery, University of Auckland, New Zealand
IIDepartment of Surgery, Auckland City Hospital, New Zealand
IIIDepartment of Surgery, University of KwaZulu-Natal, South Africa
IVDepartment of Surgery, University of the Witwatersrand, South Africa
VDepartment of Surgery, Chris Hani Baragwanath Hospital, South Africa
VIDepartment of Surgery, St James's Hospital, Ireland
VIIDepartment of Psychiatry, Waikato Hospital, New Zealand
VIIIDepartment of Surgery, Life Entabeni Hospital, South Africa
ABSTRACT
BACKGROUND: Geriatric injuries comprise a significant burden in the developed world but much less are known in the developing world setting. This study aims to review our experience of geriatric injuries with a focus on interpersonal violence (IPV) managed at a major trauma centre in South Africa.
METHODS: This was a retrospective study on all patients who were aged > 65 years admitted to our trauma centre from January 2013 to December 2020, based in Pietermaritzburg, South Africa.
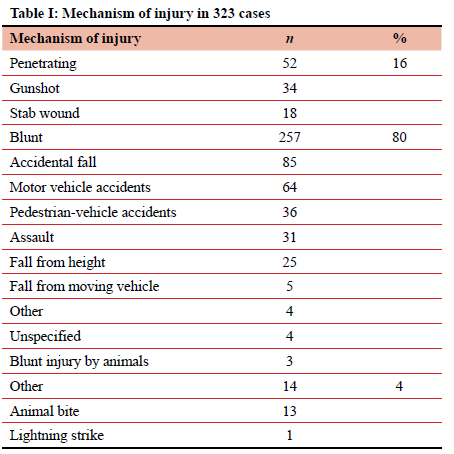
RESULTS: Over the 8-year study period, 323 cases were included (62% male, mean age 72 years). Mechanism of injury: 80% blunt, 16% penetrating and 4% others. The median injury severity score (ISS) was 9. The median Charlson comorbidity index (CCI) for all 323 cases was 3. Diabetes (n = 53) was the most prevalent comorbidity which was followed by pulmonary disease (n = 23), cerebral vascular accidents (n = 16) and myocardial infarction (n = 15). Fifteen patients were on antiretroviral therapy (5%). Twenty-four per cent required surgical intervention. Eight per cent of cases experienced one or more complications. Twenty-five per cent (80/323) were related to IPV, 61% (49/80) of these were penetrating injuries and the remaining 31 cases were blunt injuries. Of the 49 cases of penetrating injuries, 33 were gunshot wounds (GSWs) and 16 were stab wounds (SWs) (1 GSW and 2 SWs were self-inflicted and were not included in IPV). Those cases that resulted from IPV were significantly more likely to require operative intervention, experience complications and longer lengths of hospital stay. Geriatric patients had poorer outcomes than non-geriatric patients and rural geriatric patients had worse outcomes than urban geriatric patients.
CONCLUSION: Although the burden of geriatric trauma in South Africa appears to be relatively low, it is associated with significant morbidity and mortality. Trauma from interpersonal violence is especially common and is associated with significantly worse outcomes than that of non-interpersonal violence-related trauma. Elderly rural trauma victims have worse outcomes than their urban counterparts.
Keywords: trauma, geriatric, interpersonal violence
Introduction
The world is facing a divergent demographic future. Globally, the geriatric population will more than double, from 900 million in 2015 to about 2 billion by mid-century.1 Most developed countries experience an ageing population and an alarming reduction in fertility rates. This is in stark contrast to the developing world where there is a burgeoning population. Countries such as Nigeria are set to have an excess population of 400 million people by mid-century.2 Trauma is a significant cause of preventable mortality and morbidity in the elderly worldwide.3 In high-income countries (HICs), geriatric trauma currently accounts for up to 25% of all trauma admissions.4,5 The management of geriatric trauma patients is made challenging by the presence of concurrent comorbidities, the use of polypharmacy, and decreased functional reserve.6,7 Mortality also increases substantially with age, even adjusting for injury severity score when compared to younger adults, which reflects the vulnerability of this special patient population.46
South Africa is a middle-income country (MIC) beset by huge discrepancies in wealth and access to healthcare.8 The unique socio-political history of South Africa means that it encompasses both an ageing population, as experienced in HICs, and a burgeoning young population as encountered in the rest of Africa.7,9 The current life expectancy in South Africa is sixty-five years, which is below that of HICs, but higher than other countries in Africa.10 Over and above this, South Africa experiences a disproportionately high rate of trauma and injury.3 Geriatric trauma in South Africa is almost certainly overshadowed by trauma in the young, and consequently under-reported in the literature.11 Interpersonal violence (IPV) against the elderly is common and frequently under-reported. Paradoxically, there is very limited literature in South Africa that specifically focuses on this area. This study aims to redress these imbalances.
Materials and methods
A retrospective study was undertaken at the Pietermaritzburg Metropolitan Trauma Service (PMTS), Pietermaritzburg. The regional trauma registry, known as the hybrid electronic medical registry (HEMR) was reviewed for the 8-year period from January 2013 to December 2020.12
The study
All patients admitted to our trauma centres from January 2013 to December 2020 were included. Basic demographic details were reviewed. Injury mechanism, clinical progress and clinical outcome were analysed. Specific subgroup analysis was performed focusing on cases of physical assault and comparison between geriatric and non-geriatric populations, urban and rural geriatric trauma patients and victims of IPV and non-IPV-related trauma patients.
Statistical analysis
Statistical analysis was completed using IBM SPSS version 27 for Windows (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). Normality of data was investigated using the Shapiro-Wilk test and by graphical inspection. Normally distributed continuous variables were compared using an independent, two-tailed t-test, whereas categorical data groups were compared using chi-squared or Fisher's exact test where appropriate. Non-normally distributed continuous variables were compared using Mann-Whitney U. A /rvalue of < 0.05 was taken as statistically significant.
Results
Overview
Over the eight-year study period, a total of 12 779 trauma patients were admitted of which (83%) were males and the median age was 29 years. Sixty per cent sustained blunt trauma, whilst the remainder sustained penetrating trauma. Fifty-five per cent of all trauma was secondary to assault either, in the form of a stab wound (SW), gunshot wound (GSW), or blunt assault. The overall mortality rate for all trauma admissions was 4%. Of the total number of admissions, 323 (3%) were aged over 65 years.
Geriatric patient cohort
Of the 323 patients over the age of 65 years, there were 201 males (62%) and the mean age was 72 years (range 65-97).
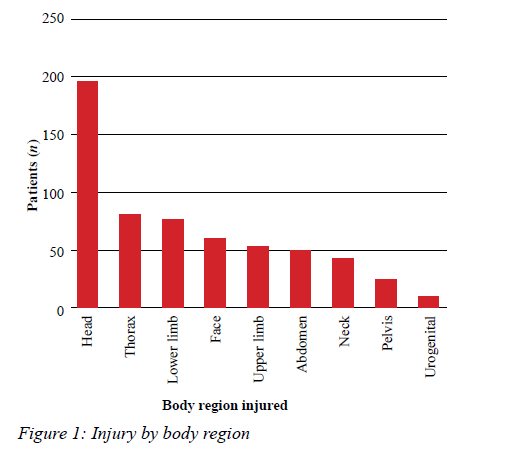
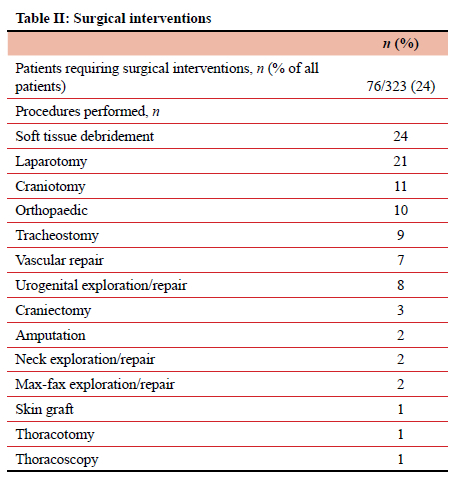
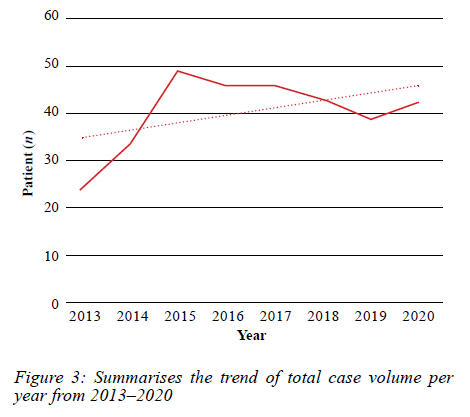
There were 257 cases of blunt trauma (80%), 52 cases of penetrating trauma (16%) and 14 cases of other types of trauma (4%). The median ISS was 9. The mechanism of injury for all 323 cases is summarised in Table I. The body region injured is summarised in Figure 1. The median Charlson comorbidity index (CCI) for all 323 cases was 3. Diabetes (n = 53) was the most prevalent comorbidity, followed by pulmonary disease (n = 23), cerebrovascular accident/transient ischaemic attack (CVA/TIA) (n = 16) and myocardial infarction (n = 15). Fifteen patients were on antiretroviral therapy (5%) and 144 patients had hypertension (45%) (Figure 2). A total of 76 patients (24%) required surgical intervention and these interventions are listed in Table II. During the 8-year period, there was a trend of increase in the total number of cases per year, shown in Figure 3.
Clinical outcomes
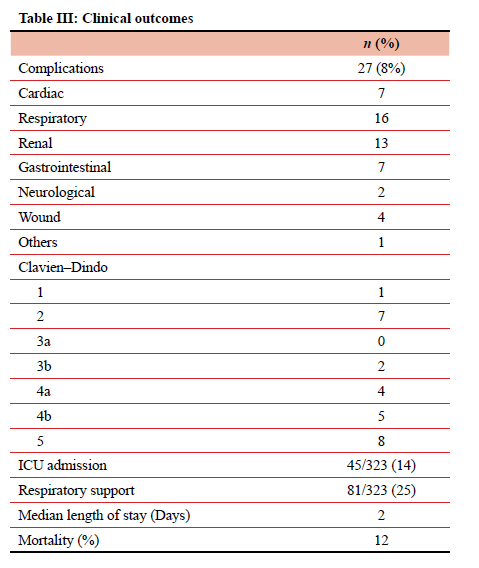
A total of 27 (8%) patients experienced one or more complications during their stay. Respiratory (n = 16), renal (n = 13), cardiac (n = 7) and abdominal (n = 7) complications were most frequent. A total of 81 patients required respiratory support at some time during their admission (25%). A total of 45 patients (14%) required admission to intensive care unit (ICU). The median length of hospital stay was 2 days with the range of 1 to 52 days. The overall mortality was 12% (Table III). The mortality for admission of all ages below 65 during the same period was 4%.
Non-geriatric population vs geriatric population
Direct comparisons were made between patients aged less than 65 years (non-geriatric group) and those aged 65 years and above (geriatric group). There were 12 456 cases of non-geriatric cases (median age 28) and 323 cases of geriatric cases (median age 70). The non-geriatric group had a significantly higher proportion of males (83%) than that of the non-geriatric group (62%). Both groups had similar ISS and operative intervention. However, the geriatric group had significantly higher rates of postoperative complications, ICU admissions, and increased lengths of stay. There was a three-fold difference between the mortality rates of the geriatric group (12%) and the non-geriatric group (4%) (Table IV).
Sub-group analysis
Further sub-group analysis was performed comparing urban and rural geriatric trauma patients and between patients over 70 and those between 65 and 70. Of the 323 cases in the study, 68% (219) were from urban areas and the remaining 32% (104) were from rural areas. Rural patients were more likely to require operative intervention (p = 0.001), ICU admission (p = 0.042), have longer hospital stay (p < 0.001), and higher mortality rates (p = 0.007) than urban patients. The crude odds ratio (OR) for death in rural vs urban was 2.51 (95 CI 1.27-4.94). Table V compares the patients aged 65-70 (174) with those 70 and older (149). There was no difference in outcome between these two cohorts.
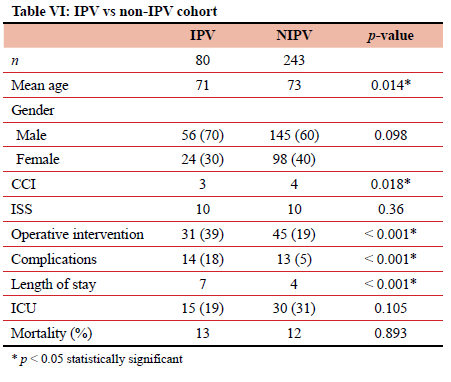
Interpersonal violence
Twenty-five per cent of geriatric trauma patients (80/323) sustained IPV, and 61% (49/80) of these were penetrating injuries. Of the 49 cases of penetrating injuries, 33 were GSWs and 16 were SWs. In 26 cases (32.5%) there was a record of the perpetrator. In 12 cases (15%), the assault was inflicted by a single perpetrator known to the victim, of which nine were family members and three were neighbours. In the other 14 cases (18%), the perpetrators were intruders who were unknown to the victim (Table VI). Sub-group analysis comparing IPV patients and non-IPV patients showed that although both groups had similar gender distributions and ISS, IPV victims were significantly more likely to require operative intervention, experience complications and have a longer length of hospital stay than non-IPV victims (Table VI).
Discussion
The developed countries of the world are experiencing population decline as fertility rates decrease. In addition, the population in these high-income countries is steadily aging as life expectancy increases. Unlike the situation in HICs, Africa is estimated to experience demographic growth of 2.7% a year. The majority of the population in Africa will be young. This results in a stark contrast between an ageing rich world and a young poor world.1,2,9,10 The number of geriatric patients (> 65 years of age) is set to increase dramatically in the HICs of the world.13 Additionally, with the increase in life expectancy in the low-income countries, it is expected that the low- and middle-income countries will have 80% of the world's older people by 2050.1
Geriatric trauma makes up a very small proportion of the overall trauma burden in South Africa. However, outcomes for geriatric trauma are far worse than the equivalent outcomes for younger patients. The mortality rate for trauma in geriatric patients is three times the rate for younger trauma patients, and geriatric patients have significantly higher rates of postoperative complications, ICU admission and increased lengths of stay.
The massive epidemic of IPV, which South Africa has been unable to reduce, also contributes to this increased vulnerability.14 A significant proportion of geriatric trauma in South Africa is secondary to IPV and frequently the perpetrator is known to the victim. Geriatric victims of IPV have worse outcomes than geriatric trauma victims in general and are significantly more likely to require operative intervention, experience complications and have a longer length of hospital stay than non-IPV victims. Rural trauma victims have worse outcomes than urban trauma victims and are more likely to require operative intervention (p = 0.001), ICU admission (0.042), have longer hospital stay (p < 0.001), and higher mortality rates (p = 0.007) than urban patients. The above demonstrates the concept of intersectionality. Intersectionality implies that risk factors and vulnerabilities are cumulative and can combine to deliver worse outcomes for already vulnerable patients.15
Conclusion
Although the burden of geriatric trauma in South Africa appears to be relatively low, geriatric trauma is on the rise and is associated with high morbidity and mortality. Trauma from interpersonal violence is especially common in our environment and is associated with significantly worse outcomes than that of non-interpersonal violence-related trauma. Elderly rural trauma victims have worse outcomes than their urban counterparts.
Conflict of interest
The authors declare no conflict of interest.
Funding source
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethical approval
Ethical approval for this study and maintenance of the registry was obtained from the Biomedical Research Ethics Committee (BREC) of the University of KwaZulu-Natal (reference: BE 207/09 and BE215/17).
ORCID
Β Lee https://orcid.org/0000-0003-3628-1054
VY Kong https://orcid.org/0000-0003-2291-2572
C Cheung https://orcid.org/0000-0002-4471-2822
Ν Rajaretnam https://orcid.org/0000-0001-9809-6896
V Thirayan https://orcid.org/0000-0002-4528-8445
JL Brucehttps://orcid.org/0000-0001-8666-4104
V Manchev https://orcid.org/0000-0001-9152-0092
RP Mills https://orcid.org/0000-0001-8678-8422
GL Laing https://orcid.org/0000-0001-8075-0386
DL Clarke https://orcid.org/0000-0002-8467-1455
REFERENCES
1. World Health Organization. Ageing and health. 4 October 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed 7 Oct 2021. [ Links ]
2. United Nations. World Population Prospects (2019) -Highlights. Department of Economic and Social Affairs, Population Division. ST/ESA/SER.A/423. [ Links ]
3. Hardcastle T, Oosthuizen G, Clarke D, et al. Chapter 15. Trauma a preventable burden of disease in South Africa: review of the evidence with a focus on KwaZulu Natal. SAHR; 2016. p. 179-89. [ Links ]
4. Burstow M, Civil I, Hsee L. Trauma in the elderly: demographic trends (1995-2014) in a major New Zealand trauma centre. World J Surg. 2019;43(2):466-75. https://doi.org/10.1007/s00268-018-4794-4. [ Links ]
5. Jiang L, Zheng Z, Zhang M. The incidence of geriatric trauma is increasing and comparison of different scoring tools for the prediction of in-hospital mortality in geriatric trauma patients. World J Emerg Surg. 2020;15(1):59. https://doi.org/10.1186/s13017-020-00340-1. [ Links ]
6. Braun B, Holstein J, Fritz T, et al. Polytrauma in the elderly: a review. EFORT Open Rev. 2017;1(5):146-51. https://doi.org/10.1302/2058-5241.1.160002. [ Links ]
7. Benedict M, Adefuye A. Profile of geriatric presentations at the emergency department of a rural district hospital in South Africa. Pan Afr Med J. 2020;36:245. https://doi.org/10.11604/pamj.2020.36.245.22530. [ Links ]
8. Gordon T, Booysen F, Mbonigaba J. Socio-economic inequalities in the multiple dimensions of access to healthcare: the case of South Africa. BMC Public Health. 2020;20:289. https://doi.org/10.1186/s12889-020-8368-7. [ Links ]
9. Guengant J, May J. Africa 2050 African Demography. Washington, DC: Centennial Group for Emerging Market Forum; 2013. Available from: https://horizon.documentation.ird.fr/exl-doc/pleins_textes/divers13-07/010059333.pdf. [ Links ]
10. World Health Organization. Life expectancy at birth (years) [Internet]. Available from: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/life-expectancy-at-birth-(years). Accessed 7 Oct 2021. [ Links ]
11. Gallaher J, Haac B, Geyer A, et al. Injury characteristics and outcomes in elderly trauma patients in Sub-Saharan Africa. World J Surg. 2016;40(11):2650-7. https://doi.org/10.1007/s00268-016-3622-y. [ Links ]
12. Donovan MM, Kong VY, Bruce JL, et al. The hybrid electronic medical registry allows benchmarking of quality of trauma care: a five-year temporal overview of the trauma burden at a major trauma centre in South Africa. World J Surg. 2019;43(4):1014-21. https://doi.org/10.1007/s00268-018-04880-1. [ Links ]
13. Gray L, Peel N, Costa A, et al. Profiles of older patients in the emergency department: findings from the interRAI Multinational Emergency Department Study. Ann Emerg Med. 2013;62(5):467-74. https://doi.org/10.1016/j.annemergmed.2013.05.008. [ Links ]
14. Seedat M, Van Niekerk A, Jewkes R, et al. Violence and injuries in South Africa - prioritising an agenda for prevention. Lancet. 2009;374(9694):1011-22. Erratum in: Lancet. 2009;374(9694):978. https://doi.org/10.1016/S0140-6736(09)60948-X. [ Links ]
15. Gkiouleka A, Huijts T, Beckfield J, Bambra C. Understanding the micro and macro politics of health: inequalities, intersectionality & institutions - a research agenda. Soc Sci Med. 2018;200:92-98. https://doi.org/10.1016/j.socscimed.2018.01.025. [ Links ]
 Correspondence:
Correspondence:
email: victorywkong@yahoo.com














