Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.4 Cape Town Dec. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3670
SURGICAL TECHNOLOGY
Technology alone does not achieve error reduction - a study of handwritten, tick-sheet, ink stamp and electronic medical prescriptions
CH KruseI, II; MTD SmithII, III; DL ClarkeII, IV
IDepartment of Ophthalmology, Grey's Hospital, South Africa
IIDepartment of Surgery, University of KwaZulu-Natal, South Africa
IIIDepartment of Surgery, Grey's Hospital, South Africa
IVDepartment of Surgery, University of the Witwatersrand, South Africa
ABSTRACT
BACKGROUND: Technology in the form of electronic record systems and prescriptions have been touted as a potential solution to human error. In South Africa, a middle-income country where health facilities have large variations in technological capacity, prescription errors can be complex and varied. We evaluated different prescribing methods to find if the increased use of technology in prescriptions will assist in reducing error rates
METHODS: A retrospective, non-randomised study compared prescriptions, error rates and types in four hospitals with different prescribing methods: these were handwritten, ink stamp, tick-sheet and electronic prescriptions. A modern human error theory data collection tool was designed which included patient complexity. Cataract surgery was chosen as the single common procedure
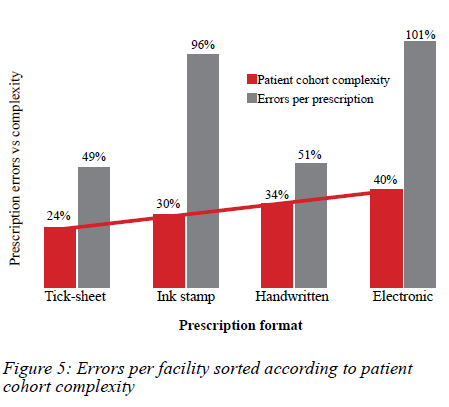
RESULTS: One thousand six hundred and sixty-one individual scripts had 1 307 prescription errors. Increasing patient complexity was not an indicator of error rate. Handwritten and tick-sheet prescriptions had the fewest errors (49% and 51%, respectively). Electronic (96%) and ink stamp scripts (101%) had almost twice as many errors as handwritten scripts (p < 0.001) mainly due to systemic inbuilt errors
CONCLUSION: The application of increasing degrees of technological complexity does not automatically reduce error rate. This is especially apparent when technology is not integrated into human factors engineering and persistent critical assessment
Keywords: prescriptions, medication, orders, error, handwritten, stamp, tick-sheet, electronic, computerised, EHR, CPOE
Introduction
The publication of "To err is human" at the turn of the millennium1 drew attention to the problem of human error in health care. Since then, it has been widely accepted that human error contributes substantially to morbidity and even mortality in health care. The response to this has been to deepen our understanding of human error and to attempt to develop error reduction strategies. These strategies accept that error is endemic and more likely to occur in so-called error-prone environments. Variations in human responses to an external milieu can be both harmful and very positive. On the one hand, they may result in unexpected and undesired events; on the other, human innovation and problemsolving capacity may be key to solving certain unusual and unexpected clinical dilemmas. Clinical algorithms and guidelines are designed for common well understood situations and attempt to direct human behaviour down consistent and proven pathways which are most likely to deliver an optimal result. Examples of such algorithms include early warning systems, clinical guidelines, tick-box clerking sheets and electronic prescriptions. Technology in the form of electronic record systems and prescriptions have been touted as a potential solution to human error.2-5 Technology is used to guide and support human decision making along a pathway most likely to achieve a desirable outcome.
One of the biggest sources of error in contemporary health care is in the writing and filling of prescriptions.1,6 The Departments of Surgery and of Ophthalmology in the KwaZulu-Natal (KZN) public health sector deliver care across a number of centres in the province. Each of these centres uses a different mechanism to prescribe medication. In light of the above, this project set out to compare the prescribing techniques of each institution and to record and quantify the number or errors associated with each technique. It is hoped that this will lead to the development of a more standardised approach to prescribing.
Methods
This is a retrospective, non-randomised study comparing error rates and types for four different methods of prescribing in the public sector: handwritten, ink stamp, tick-sheet and electronic scripts.
The primary care hospital has a paper-based health record system but utilises pre-inked stamps to prescribe medication for common conditions. Besides the name and date, prescribers must also occasionally edit the stamped medications for patient and pathology variations (Figure 1).
The secondary care hospital uses a tick-sheet prescription system where the most commonly prescribed medications are pre-printed. Only minimal writing is involved, such as date and doctor's name. Figure 2 shows a typical prescription pad from the hospital. The tertiary care hospital has a paper-based health record, and all scripts are entirely handwritten (Figure 3). This entirely paper-based system will be used as baseline for comparisons to other prescribing methods. The quaternary care hospital has a fully electronic medical record system (Figure 4). Nothing is handwritten by the prescriber except for a signature.
Male and female patients of all ages and race were included. Cataract surgery was chosen as the single common procedure, which was mutual to all sites, This ensured maximal case homogeneity when comparing hospitals of different levels. Error in prescribing is taken as defined in the 2003 amendments made to the South African Medicines and Related Substances Act 101.7 Patient complexity at each facility was taken into consideration by two methods: enumerating the preoperative risk factors that could have a direct bearing on the procedure and/or outcome, and number of medications per patient.
Data collection
A data collection sheet (see Supplementary Data) was created using modern error theory.89 Errors were classified and tabulated into "prescription aspect" (rows), "error class" (columns), "general errors" and "other". An example of each error was included into each cell to aid categorisation. Errors were evaluated by the authors according to prescribed scripting minimum criteria.7 Ahn error was only entered into one cell according to best-fit principle. Where best-fit was not readily apparent to one author or where legibility was in question, the potential error was discussed among all authors and chosen by majority vote. Errors in omitting vital medication, and including contraindicated medication, were found and confirmed by the senior ophthalmologist. The same team performed data collection and evaluation at all sites. No sampling was used: consecutive prescriptions of postoperative cataract discharges were included for the years 2019 and 2020.
Data analysis
All variables were categorised as categorical variables and placed in a Microsoft Excel spreadsheet. This spreadsheet was imported into R Studio (R Foundation for Statistical Computing). All variables were expressed as frequencies and percentages. The frequencies of all error classes across all prescription aspects of the handwritten scripts were compared to the errors of the ink stamp, tick-sheet and the electronic system, respectively, using the chi-square test. Alpha level was set at 0.05. Odds ratios were calculated for all comparisons.
Results
A total of 1 661 individual scripts were reviewed and 1 307 prescription errors were noted. The 488 ink stamp scripts had 470 errors (96%), 331 tick-sheet scripts had 163 errors (51%), 355 handwritten scripts had 180 errors (49%), and 487 electronic scripts contained 494 errors (101%). The error rate for each prescription can be higher than one, if a single prescription displayed two or more distinct errors (e.g., incorrecl route as well as omitted date). The complexity of the cohort of patients at each facility was evaluated as a percentage: number of preoperative risk foctors to number of scripts. If the hospitals are rearranged according to patient difficulty, it is clear that increasing complexity was not an indicator for more errors (Figure 5). The average number of medications prescribed per patient (line items) ranged from 4.47 to 5.66 between the four hospitals (p = 0.003) and a higher number of prescription items did match with higher error rates. The average line items per prescription, however, varied only 27%, while error variation more than doubled from lowest to highest. Number of medications per prescription thus seems to have a relatively small impact on error rates.
Prescription aspect errors
The rates of the individual prescription aspect errors were calculated, and each compared to the handwritten errors. Each prescription technique seemed to have its own peculiarities with regards to error types and no common thread between them could be identified. (Table I: most extreme rates highlighted).
Ink stamps fared particularly poorly, in terms of lost scripts (p < 0.001) as well as errors in route and laterality (p < 0.001). Tick-sheet prescriptions did worst (p < 0.001) with regards to prescriber name legibility, which happens to be one aspect that had to be handwritten. Handwritten scripts fared substantially worse with errors of quantity/ duration (p < 0.001). Electronic scripts had especially large error rates for both medication strength (p < 0.001) and laterality (p < 0.001) but had very few errors in most of the other categories. These two errors were the chief reasons why electronic scripts fared twice as poorly as handwritten prescriptions.
Error class
The ink stamp prescriptions did particularly poorly in the omission category primarily because the stamps being used had some vital information (route and laterality) missing (Figure 1). Tick-sheet prescriptions did not show a substantial improvement with regards to illegibility (p = 0.053) compared to the handwritten (baseline) scripts. Handwritten scripts did markedly poorer (p < 0.001) with regards to incompleteness compared to all other forms of prescribing (Table II). The only other significant result was that it did worse in incorrectness errors, but only when compared to ink stamp scripts (p < 0.001). The electronic system had one field that was inaccurate which led to a considerable number of errors (p < 0.001); however, most errors in the EMR format were errors of omission (p < 0.001) because the system had not been programmed to accept some vital fields such as laterality (left eye vs right eye). This single system error accounted for more than half of all mistakes.
Discussion
The interaction between a human agent and an external environment or situation produces a result. Often the situation facing the human agent has been previously encountered and there are well-established approaches to managing the situation. Whilst there may be variations and nuances within each situation, by and large, these tend to deviate around a mean, and common clinical scenarios share a degree of similitude.3 This allows for a standardised response, which will in the vast majority of situations produce an acceptable outcome.9 There is also a degree of inherent human variability in the response to any clinical scenario, and this variability may generate human error. Error reduction strategies generally try and eliminate the inherent human variability associated with performing a routine well understood task.3810 Mechanical methods, such as the use of traffic calming outside schools, is an example of such an approach. The speed bump forces motorists to slow down. Such mechanisms do not require any human volition to induce compliance and are hence highly effective. Other mechanisms do require human volition and this interaction creates further room for variability. The use of electronic prescriptions is an example of an interaction between a mechanism designed to promote compliance and a human agent. Modern technology interacts with a human agent to promote compliance. There are many examples of this in the realm of online commerce and online forms.8 This study has demonstrated how human error reduction strategies interact with human factor engineering. The application of increasing degrees of technological complexity did not reduce the error rate and both the handwritten and ink stamp scripts had the lowest rates of error, whilst the tick-box and electronic scripts had the highest error rate. Poorly designed electronic systems which are not integrated into the workflow activity of human users may result in poor compliance and increased levels of human error.
These results stand in stark contrast to other studies in developing countries, such as in west Africa,11 Egypt12 and Indonesia,13 where technology assisted in decreasing error in prescribing. These results are, however, far from universal. A 2018 systematic review of electronic physician orders found medication-prescription errors ranging from 6.1 to 77.7%.14 This duality can also be seen in this study: as the technology increases, the sheer number of types of error seems to decrease, but importantly the number of mistakes within specific types of error often increase. It would appear that technology may be less flexible than human actions. Vigilant review of technology-based systems is required to detect these recurring errors and thus reduce the total number of mistakes.
The current prescribing system in KZN represents a lack of standardisation across a workspace and staff who have to rotate through these institutions during the course of their routine clinical duties will be continually forced to change routine behaviour depending on which institution they are currently working in. This disruption of routine behaviour must also be considered as a potential error promoting environment.
Study limitations
This study is retrospective and observational with non-random sampling. The tools to measure the different methods of prescribing have inherent defects and this limits generalisability in terms of the method of prescribing. The clinics with tick-sheet and stamp prescriptions aid some doctors with particularly poor handwriting which would skew the data significantly. However, the study informs on real-life, local data regarding the impact of these tools with their design problems.
Each hospital where the study was conducted had not only different prescription methods, but also some physical system differences. This can most clearly be seen in the large number of missing patient files in the ink stamp group, whereas the other paper-based institutions (tick-sheet and handwritten) had substantially fewer. However, exclusion of the "missing file" error did not make an appreciable difference in the outcomes.
Conclusion
Human error reduction strategies do not achieve the desired effect of reducing human error if technology alone is not integrated with human factors engineering and persistent critical assessment. None of the facilities in this study have ever audited their prescriptions and no system employs a clinical decision support system.
Implications
Medical institutions should be wary of attempting a reduction in prescription mistakes by merely converting to a system of higher technology, such as electronic records. Each system has its own peculiar set of potential errors, and frequent audits and evaluations are essential in reducing human error.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Biomedical Research Ethics Committee of the University of KwaZulu-Natal (approval number BREC/00002077/2020). The data underlying this article will be shared personally on reasonable request to the corresponding author.
ORCID
CH Kruse https://orcid.org/0000-0002-8805-8383
MTD Smith https://orcid.org/0000-0002-6954-153X
DL Clarkehttps://orcid.org/0000-0002-8467-1455
REFERENCES
1. Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is human: building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, editors. Washington (DC): National Academies Press (US); 2000. PMID: 25077248. [ Links ]
2. Dhillon BS. Human reliability and error in medical system. World Scientific. 2003. https://doi.org/10.1142/5264. [ Links ]
3. Gawande A. The Checklist Manifesto (HB). India: Penguin Books; 2010. [ Links ]
4. Laing G, Bruce J, Skinner D, et al. Using a hybrid electronic medical record system for the surveillance of adverse surgical events and human error in a developing world surgical service. World J Surg. 2015;39(1):70-79. https://doi.org/10.1007/s00268-014-2766-x. [ Links ]
5. Donovan MM, Kong VY, Bruce JL, et al. The hybrid electronic medical registry allows benchmarking of quality of trauma care: a five-year temporal overview of the trauma burden at a major trauma centre in South Africa. World J Surg. 2019;43(4):1014-21. https://doi.org/10.1007/s00268-018-04880-1. [ Links ]
6. Bogner MS. Human error in medicine. 1st ed. CRC Press; 2018. https://doi.org/10.1201/9780203751725. [ Links ]
7. South African Government. General regulations made as amended-Government Notice R510 in Government Gazette No. 24727. [ Links ]
8. Reason J. Human error: models and management. BMJ. 2000;320(7237):768-70. https://doi.org/10.1136/bmj.320.7237.768. [ Links ]
9. Reason J. The human contribution: unsafe acts, accidents and heroic recoveries. CRC Press; 2017. https://doi.org/10.1201/9781315239125. [ Links ]
10. Dorner D. The logic of failure: recognising and avoiding error in complex situations. Basic Books; 1997. [ Links ]
11. Marful WA, Winter A. When information technology meets healthcare in West Africa: a literature review. J Health Inform Afr. 2014;2(2). [ Links ]
12. Kenawy AS, Kett V. The impact of electronic prescription on reducing medication errors in an Egyptian outpatient clinic. Int J Med Inf. 2019;127:80-87. https://doi.org/10.1016/j.ijmedinf.2019.04.005. [ Links ]
13. Nurhaeni N, Suarjana K, Wirawan I. Electronic prescribing reduces prescription errors in Sanglah General Hospital Denpasar. Public Health and Preventive Medicine Archive. 2017;5(2):84-9. https://doi.org/10.15562/phpma.v5i2.19. [ Links ]
14. Korb-Savoldelli V, Boussadi A, Durieux P, Sabatier B. Prevalence of computerised physician order entry systems-related medication prescription errors: a systematic review. Int J Med Inf. 2018;111:112-22. https://doi.org/10.1016/j.ijmedinf.2017.12.022. [ Links ]
 Correspondence:
Correspondence:
ruraleye@gmail.com
Supplementary Data
The supplementary data is available in pdf: [Supplementary data]














