Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.3 Cape Town Sep. 2022
http://dx.doi.org/10.17159/2078-5151/sajs3642
SHORT REPORT
A randomised control trial of intraoperative and early outcome in scalpel versus monopolar diathermy for midline abdominal incisions
PO Igwe; A Dodiyi-Manuel; PN Wichendu
Department of Surgery, University of Port Harcourt Teaching Hospital Port Harcourt, Nigeria
ABSTRACT
BACKGROUND: Cutting diathermy is an alternative to scalpel for all layers of abdominal entry despite the perception that it impairs healing, increases infection risk and has worse cosmesis. This prospective, randomised, controlled trial was carried out to compare the intraoperative and early outcome in diathermy to scalpel for midline abdominal incisions in general surgery
METHODS: The study was conducted from 1 October 2014 to 31 May 2016. Ethical approval was obtained. The incision time, wound size or area, and volume of blood loss were determined for each group of diathermy and scalpel. Results were analysed with SPSS version 23.0
RESULTS: Two hundred and thirty-four patients (93.6%) met the inclusion criteria and were successfully randomised to mode of entry incision - group A monopolar diathermy (118 patients), and group B scalpel (116 patients). The mean incision time was 3.9 ± 1.6 minutes, wound size or area was 54.8 ± 24.4 cm2, volume of blood loss was 46.0 ± 25.5 ml and volume of blood loss per area was 0.99 ± 0.7 ml/cm2 for group A, while the mean incision time was 5.6 ± 2.5 minutes, wound size or area was 57.3 ± 27.3 cm2, volume of blood loss was 62.2 ± 30.6 ml and volume of blood loss per area was 1.3 ml/cm2 ± 0.8 for group B, respectively. The differences in these means were statistically significant
CONCLUSION: Incisions made with diathermy resulted in shorter incision time and lesser blood loss when compared to that made with the scalpel. There was no difference in the rate of surgical site infection. These procedural results favour the use of diathermy for abdominal entry
Keywords: intraoperative, early outcome in scalpel, monopolar diathermy, midline abdominal incisions
Introduction
Skin incisions have traditionally been made using a scalpel.1,2 The alternative is cutting diathermy despite the perception that it impairs healing, increases infection risk and has worse cosmesis. This study aimed to compare the intraoperative and early postoperative outcomes of midline abdominal incisions made using scalpel with monopolar diathermy. The primary endpoints were to compare incision time and volume of blood loss, while the secondary endpoint was to compare surgical site infection rates.
Methods
The study was carried out at the Department of Surgery University of Port Harcourt Teaching Hospital (UPTH) Rivers State, Nigeria. The study recruited 234 consecutive adult patients undergoing a midline laparotomy. Using a stratified systematic random sampling technique, patients were allocated to the incision being made entirely with diathermy or by scalpel. Patients who had metal prosthesis implants or a cardiac pacemaker were excluded.
The procedures were done under general inhalation anaesthesia. The skin of the operative site was shaved, cleaned with 5% cetrimide containing 0.5% chlorhexidine. Then 70% isopropyl alcohol was applied. The abdominal midline incision was closed in each case using mass closure technique with non-absorbable suture (nylon 2). The skin was closed by simple interrupted sutures.
Wound-related blood loss was by gravimetric method3,4 using an electronic digital scale.
The length (L) and depth (D) of incision were measured using sterile tape and a calliper. Depth of incision (cm) was measured from skin to peritoneum. The area covered was by incision = L x D cm2.
Prophylactic antibiotics were given only for clean-contaminated operations. A blinded assessor documented the outcomes, time to wound healing and duration of hospital stay using a guide.5
Statistical analysis
The data collected was analysed using SPSS version 23.0. Continuous variables were compared by student t-tests. Results were presented as mean ± standard deviation (SD), percentages and tables, while proportions or categorical parameters were analysed with the chi-square test or two-tailed Fisher's exact test as appropriate. A p-value of 0.05 or less was considered statistically significant. A student t-test was used to determine the mean difference between the two groups.
Results
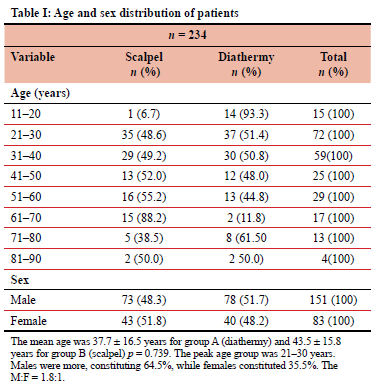
Of the 250 patients who had midline abdominal incisions during the study period, 234 patients (93.6%) met the inclusion criteria and were randomised. Group A (118 patients) - monopolar diathermy, group B (116 patients) - scalpel. Eighty-six patients (36.8%) had elective and 148 patients (63.2%) had emergency surgeries. Group A consisted of 45 elective, 73 emergency cases. Group B consisted of41 elective, 75 emergency cases. The age and sex distribution of the patients studied are shown in Table I.
Penetrating abdominal injuries were the most common (51; 21.8%), followed by intestinal obstruction (48; 20.5%). Clean-contaminated wound was the most common (145; 61.9%). The xiphisternum to pubic symphysis incision was the most common type of incision (127; 54.3%).
The mean incision area, time, length and blood loss with level of significance, are summarised in Tables II-IV.
The overall surgical site infection rate was 10.7%. The rate of infection in group B (scalpel) was 11.2%, while the rate of infection in group A (diathermy) was 10.2%. This difference in rates was not statistically significant (p = 0.797). The rates of infection were 2.0%, 9.7%, 27.6% and 18.2% in clean, clean-contaminated, contaminated and dirty wounds, respectively. The corresponding rates in the scalpel group were (0.0%, 9.6%, 42.9% and 0.0%) and in the diathermy group (3.8%, 9.7%, 13.3% and 40.0%) for each of the wound classes.
The wound culture result showed that Escherichia coli was the most commonly isolated organism from contaminated and dirty wounds. It constituted 44%, followed by Pseudomonas aeruginosa (20%).
Proportions of secondary wound healing was higher in scalpel (10.3%) than in diathermy (7.6%). This difference of proportion in secondary wound healing was, however, not statistically significant (p = 0.467).
Other complications such as oedema, seroma and hae-matoma formation did not differ markedly between the two groups. Table IV shows the summary of all the results.
Discussion
Incision time was longer in scalpel patients compared to diathermy patients. This observation was statistically significant (p = 0.0001), thus highlighting the advantage of diathermy over scalpel when making surgical incisions. This is similar to other studies in the literature.5-7 A statistically significant difference in mean area was incised within a unit shorter time (16.0 ± 8.5 cm2/minute) when using diathermy compared with a lesser mean area per unit time (12.8 ± 9.5 cm2/minute) while using scalpel. This means that incisions made with diathermy were faster to cover larger area per unit time compared to scalpel. Similar findings were reported by Sheikh.8 This may be attributed to the fact that as diathermy cuts during incisions, it secures haemostasis at the same time.
There was less incision blood loss (46.0 ± 25.5 ml) while using diathermy compared to scalpel (62.2 ± 30.6 ml), and this was statistically significant (p = 0.0001). This same finding was applicable also to incision blood loss per area. This finding may be due to advantage of diathermy in haemostasis (cutting and coagulation). This was similar to findings reported by some authors.5-7,9,10 For example, comparing the present study with the study by Kearns et al.,6 the mean blood loss per area in this present study in the diathermy group was 0.99 ± 0.7 ml/cm2, while theirs was 0.8 ± 0.1 ml/cm2, as against significant blood loss per area in scalpel of which this present study was 1.3 ± 0.8 ml/cm2 and their study reported 1.7 ± 0.3 ml/cm2.
Wound oedema was the most common complication, accounting for 23 (51.1%), followed by seroma and haematoma. No burn injury and wound dehiscence were noted.11 The rate of wound infection in this study for clean, clean-contaminated, contaminated and dirty wound are similar to findings in literature,12 except for dirty wounds which was lower. The overall rate of infection for clean-contaminated was similar to that reported in literature.12 This may be due to large sample size seen in this cadre as most of the cases operated were clean-contaminated. The dirty category reported in this study is in keeping with reports in animal studies13 contrary to human reports.12
The implicating organism showed that E. coli was the most common organism followed by Pseudomonas aeruginosa and Klebsiella spp, similar to findings in literature.14
There was no untoward effect observed. The use of diathermy was considered to be safe.5,15
Conclusion
Incisions made with monopolar diathermy had a shorter incision time and less blood loss when compared to scalpel entry. However, there was no significant difference in the rate of surgical site infection or other early wound complications. On the basis of these periprocedural findings, monopolar diathermy can be recommended as the preferred method for abdominal entry incision.
Acknowledgements
Professor Jacob Molai Adotey and Dr Monday Komene Sapira were supervisors of the project. We thank Profs Agbakwuru, Odigie and Ibrahim for proofreading the manuscript.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Ethical approval was obtained from the University of Port Harcourt Teaching Hospital Ethical Committee UPTH/ AMD/90/511/VOL X657.
ORCID
PO Igwe https://orcid.org/0000-0001-6107-7173
ADodiyi-Manuel https://orcid.org/0000-0003-3528-6523
PN Wichendu https://orcid.org/0000-0002-1238-0608
REFERENCES
1. Edward J, Fitzgerald F, Malik M, Ahmed I. A single-blind controlled study of electrocautery and ultrasonic scalpel smoke plumes in laparoscopic surgery. Surg Endosc. 2011;26(2):337-42. https://doi.org/10.1007/s00464-011-1872-1. [ Links ]
2. Vilos GA, Rajakunmar C. Electrosurgical generators and monopolar and bipolar electrosurgery. J Minim Invasive Gynecol. 2013;20(3):279-87. https://doi.org/10.1016/j.jmig.2013.02.013. [ Links ]
3. Vitello DJ, Ripper RM, Fettiplace MR, Weinberg GL, Vitello JM. Blood density is nearly equal to water density: a validation study of the gravimetric method of measuring intraoperative blood loss. J Vet Med. 2015;2015:152730. https://doi.org/10.1155/2015/152730. [ Links ]
4. Schorn MN. Measurement of blood loss: review of the literature. J Midwifery Womens Health. 2010;55(1):20-7. https://doi.org/10.1016/j.jmwh.2009.02.014. [ Links ]
5. Ayandipo OO, Afuwape OO, Irabor D, Oluwatosin OM, Odigie V. Diathermy versus scalpel incision in a heterogeneous cohort of general surgery patients in a Nigerian teaching hospital. Niger J Surg. 2015;21(1):43-7. https://doi.org/10.4103/1117-6806.153193. [ Links ]
6. Kearns SR, Connolly EM, McNally S, McNamara DA, Deasy J. Randomised clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg. 2001;88(1):41-4. https://doi.org/10.1046/j.1365-2168.2001.01625.x. [ Links ]
7. Shamim M. Diathermy vs. scalpel skin incisions in general surgery: double-blind, randomised clinical trial. World J Surg. 2009;33(8):1594-9. https://doi.org/10.1007/s00268-009-0064-9. [ Links ]
8. Sheikh B. Safety and efficacy of electrocautery scalpel utilization for skin opening in neurosurgery. Br J Neurosurg. 2004;18(3):268-72. https://doi.org/10.1080/02688690410001732715. [ Links ]
9. Charoenkwan K, Chotirosniramit N, Rerkasem K. Scalpel versus electrosurgery for abdominal incisions. Cochrane Database Syst Rev. 2012;(6):CD005987. https://doi.org/10.1002/14651858.CD005987.pub.2. [ Links ]
10. Chalya PL, Mchembe MD, Mabula JB, Gilyoma JM. Diathermy versus scalpel incision in elective midline laparotomy: a prospective randomised controlled clinical study. East Central African J Surg. 2013;18(1):71-77. [ Links ]
11. Ziv Y, Brosh T, Lushkov G, Halevy A. Effect of electrocautery vs. scalpel on fascial mechanical properties after midline laparotomy incision in rats. Isr Med Assoc J. 2001;3(8):566-8. [ Links ]
12. Ahmad NZ, Ahmed A. Meta-analysis of the effectiveness of surgical scalpel or diathermy in making abdominal skin incisions. Ann Surg. 2011;253(1):8-13. https://doi.org/10.1097/SLA.0b013e3181ff461f. [ Links ]
13. Sinha UK, Gallagher LA. Effects of steel scalpel, ultrasonic scalpel, CO2 laser, and monopolar electrosurgery on wound healing in guinea pig oral mucosa. Laryngoscope. 2003;113(2):228-36. https://doi.org/10.1097/00005537-200302000-00007. [ Links ]
14. Prakash LD, Belgi N, Kumar KK, Kate V. Comparison of electrocautery incision with scalpel in midline abdominal surgery - a double blinded randomised control trial. Int Surg J. 2015;19:78-82. https://doi.org/10.1016/j.ijsu.2015.04.085. [ Links ]
15. Talpur AA, Khaskheli AB, Kella N, Jamal A. Randomised clinical trial on diathermy and scalpel incisions in elective general surgery. Iran Red Crescent Med J. 2015;17(2):e14078. [ Links ]
 Correspondence:
Correspondence:
PO Igwe
Email: igwe_patrick@yahoo.com














