Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.3 Cape Town Sep. 2022
http://dx.doi.org/10.17159/2078-5151/sajs3783
REVIEW
Strategies for recovery of a surgical service in the COVID-19 era
D Nel
Division of General Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
ABSTRACT
The COVID-19 pandemic has resulted in a massive backlog of elective cases. Delays in the provision of "elective" surgical care have dire consequences for the patient: progression of disease and comorbidities, higher complication rates, and lower overall survival. Delays in elective surgery also have significant consequences for the health system: added emotional strain on healthcare workers, a reduction in training opportunities, increased costs, and increased inequality in health-service provision. As the virus is likely to become endemic, the recovery of surgical services from the initial shock of the first three waves needs to be carefully planned, in order to mitigate the further loss of elective surgical services. This article presents a narrative review of the latest international guidelines and recommendations pertaining to surgical recovery strategies in the COVID-19 pandemic. To begin with, any recovery plan should be led by a local governance committee, who need to design and implement a number of strategies across the three phases of recovery. The preparation phase includes deciding on a system of case prioritisation, assessing and organising resources, and planning innovative ways to reorganise the service itself. The perioperative phase involves putting measures in place to reduce the risk of COVID-19 transmission. The post discharge phase includes the implementation of telemedicine for follow-up, as well as methods of service audit to enable continuous adjustment and improvement. Surgical service recovery presents many challenges; however, these also present a unique opportunity to reassess and improve the efficiency of surgical care delivery.
Keywords: COVID-19, review, surgical planning, elective surgery, training
Introduction
The elective surgery backlog
The COVID-19 pandemic has brought unparalleled change and challenges to the healthcare system. The surging waves of ill and critically ill patients have necessitated a dramatic redistribution of various resources, including those allocated to the provision of elective surgery. The global backlog of elective cases after the first wave was estimated to be around 30 million, a backlog that would take almost a year to clear if hospitals increased their normal surgical volumes by at least 20%.1 Local data from six Western Cape secondary level hospitals showed that during the first wave, total surgeries decreased by 44% and elective surgeries by 74%. The surgical backlog in these hospitals would take from 4 to 14 months to clear if each hospital performed one additional operation per weekday.2 A tertiary academic centre in the KwaZulu-Natal province reported a deficit of 1 260 cases in the first wave, which would take them 315 days to clear if four additional cases were done per weekday.3 There is no data on the cumulative impact of the second and third waves on elective surgery backlogs, but an estimate from our centre, another tertiary academic hospital in the Western Cape province, is that 1 500 lists were lost, resulting in the cancellation of around 8 000 elective operations. In the unlikely scenario of no further disruption to the regular elective service by further COVID-19 waves, opening an extra theatre to do four cases per weekday would take over 8 years to recover this backlog.
Impact of delaying elective surgery
Elective surgery is not "optional" surgery and delays for diagnostic procedures as well as operations lead to higher complication rates and lower overall survival.4 Many patients will have progression of their disease or comorbidities, necessitating more complex and higher risk procedures, resulting in poorer outcomes.5
The economic implications of delayed interventions, on the patient as well as the health system, are significant.4,5 A number of "benign" conditions that have been repeatedly postponed due to the pandemic have a major impact on patients' quality of life, as well as ability to work and earn an income for themselves and their households. Prior to the pandemic, many healthcare systems, including in South Africa, already had large disparities and inequality in terms of access to healthcare.6 The delay in elective surgery recovery in the state sector will lead to even greater levels of inequality. The consequences of surgical delays will result in greater costs to already financially strained state hospitals, as more advanced and complicated disease will require more intense and expensive therapy.
The surgical workforce has also been significantly impacted, with a number of factors continuing to add to the emotional strain, including juggling childcare and home-schooling, the constant concern of getting COVID-19 and spreading it to family members, financial worries, working in unfamiliar settings, and frequently dealing with frustrated patients who are getting sicker and more desperate to have their operations done.
Cancer surgery
Although elective surgery for benign disease has been the most severely impacted by the pandemic, cancer surgery has also been affected. A survey of 133 surgeons from 85 hospitals in South Africa, revealed that access to elective surgery was reduced at 99% of the represented hospitals, with reduced access to cancer surgery at 28%.7 Apart from delays in surgical and oncological treatment, timely diagnosis has been affected as well; an example being restriction in endoscopy services and delayed detection of gastrointestinal malignancies.8 Although some cancer surgery may be temporarily deferred with or without neoadjuvant therapy, e.g., early-stage breast cancer, most hospitals consider cancer surgery to be "urgent", where patient survival or permanent function may be severely impaired by delay.8,9 Thus, cancer surgery, according to usual management timelines, has continued unabated at many institutions.8,10 An important consideration, however, is that cancer patients are more susceptible to infection in general and have worse outcomes following infection with COVID-19.9 Patients with cancer are also often elderly with multiple medical comorbidities, further increasing the risk of adverse outcomes should they contract COVID-19 perioperatively.
The recommendations that follow are primarily in the context of elective surgery for benign disease. Although many can be applied to urgent surgery for cancer patients, the decision making is often more nuanced and institution-specific, considering the time-sensitive nature of surgical as well as adjuvant and neoadjuvant oncological therapies. Despite individual variations in practice, strategies must be put in place to ensure the continuation of cancer treatment pathways, and to rapidly recover any pre-existing backlogs.
Recovery plan initiation
Since the onset of the pandemic in March 2020, a number of individual strategies and guidelines have been published on how to resume regular services once the pandemic wanes. Unfortunately, the last 18 months have shown that it is very likely the virus will become endemic, with further waves driven by new variants.11 Nonetheless, many of the strategies for "post pandemic" service recovery are applicable to future waves as well. Indeed, the challenge at hand presents a unique opportunity to assess and improve the efficiency of surgical services.
Leadership
The successful implementation of any strategy will rely on cohesive, transparent and flexible leadership. A local governance committee (LGC) is key to coordinate any recovery plan and should be multidisciplinary, with involvement of surgery, anaesthesia and nursing.12,13 Consideration should also be given to including adjunctive departments such as ICU, radiology, pathology, supply chain, administration, housekeeping, engineering and pharmacy. The LGC must be responsible for implementing specific strategies, making real-time decisions, and communicating important messages to staff and patients. As the situation may change very rapidly, the LGC needs to meet regularly to review the various aspects of the recovery process to ensure they remain on track.12,13
Re-escalation trigger
One of the first decisions to be made by the LGC is when to initiate the recovery process. However, before any such decisions can be made, the LGC needs to be aware of the hospital and community COVID-19 incidence rates.12 This is vital, not only for deciding when to initiate re-escalation of services, but also for early detection of the next surge and appropriate de-escalation. The American College of Surgery (ACS) recommends a local decrease in COVID-19 incidence for at least 14 days. Another guideline from the ACS recommends deciding on an available hospital bed capacity percentage, e.g., 25%.12,14 Regardless of the actual chosen trigger, there should be a consistent decline in numbers of new cases, such that the hospital will have the necessary resources to safely accommodate the new surgical admissions.13
The actual recovery plan can be considered in three phases: preparation, perioperative and post-discharge.
Preparation phase
Case prioritisation
Adequate preparation is critical for any recovery plan to succeed. It is important for all surgical specialties to keep an up-to-date list of postponed cases, as well as new cases where surgery booking was deferred. This will allow accurate estimations of waiting lists and enable the prioritisation process.12,13
There are a number of different methods that have been described to decide the priority in which elective cases on the waiting list are performed. It seems logical to prioritise those patients who have waited the longest or have the most serious disease, as per the elective surgery acuity scale.15 Another strategy is to defer to different specialties' own prioritisation for procedures, allowing them to use their re-allocated resources as they see fit.12 Although these methods are simple and give the surgical specialties greater autonomy, the drawback is that they may not be sensitive to the way in which more complex procedures put pressure on already scarce hospital resources.
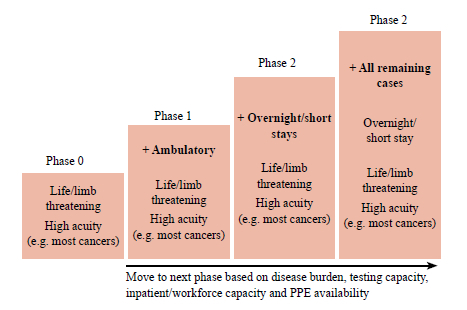
A phased approach has been suggested, whereby ambulatory elective surgery is introduced first, followed by overnight/short stay cases, and finally the remaining cases with longer stays (Addendum A).16 A more sophisticated method is the medically necessary, time-sensitive (MeNTS) scoring system, which was developed with the aim to ethically and efficiently manage the resource scarcity due to the pandemic.17 The advantage of this system is that it is flexible, transparent, objective, and can be applied to all specialties and hospital settings. It takes into account not only the resource usage for the case, but also the risk of COVID-19 transmission to the hospital team. The disadvantage of the MeNTS score is that it is cumbersome to calculate and less suitable for low- and middle-income countries (LMICs). Therefore, a South African adaptation of the MeNTS was developed and validated by Chu et al. (Addendum B).18
Hospital resource assessment and organisation
Another key preoperative component is the assessment of locally available resources, which will be required to support the resumption of elective surgeries. The laboratory needs to be able to manage with the number of new tests required for elective patients, with reliable turnaround times to assist with list planning.13 In addition, surgeons and anaesthetists need to be educated on how to interpret and act on test results in the local setting.12 Adjunctive services need to be communicated with to determine if they have adequate facilities to manage with the resumption of services -this includes ICU, radiology, pathology, engineering and housekeeping.
The ACS recommends that a stored inventory or reliable chain of personal protection equipmen (PPE) for at least 30 days should be in place before commencing with the recovery plan.12 The Centre for Disease Control (CDC) Ebola PPE calculator is a tool that can be used to work out how much PPE will be required. (https://www.cdc.gov/vhf/ebola/healthcare-us/ppe/calculator.html). In addition to PPE, the theatre must take inventory of equipment and stock to ensure that adequate supply is available to meet the new demand. To avoid wastage, available stock must be organised such that items near expiry dates are used first.
Surgical workforce
One of the greatest challenges is to plan adequate staffing to cover routine, as well as extended/expanded hours to recover the backlog. This has to include contingency planning for when staff members are ill.13 Thus, the human resource requirement is significant and likely to be the main barrier to ramping up service provision. A number of creative solutions to this dilemma have been proposed. This includes hiring retired surgeons, anaesthetists and nurses on a contract basis, and involvement of the private sector which usually has more capacity.12 Another suggestion is to revise the job plans of senior clinicians, to reflect an increased proportion of time in theatre versus other commitments.13
A very important aspect to consider regarding the surgical workforce, is the degree of physical and emotional burnout due to the pandemic.12 After the first wave, some groups reported very high rates of psychological harm, including depression, anxiety, with post-traumatic stress disorder (PTSD) rates up to 40%.19 These figures are comparable to those reported by troops returning from active military deployment. Instead of immediately putting staff back into frontline roles, there should be consideration of instituting a 2-3 week "decompression" period. This would involve a formal, structured, monitored programme including debriefing, reflection and psychological support. During this period, the LGC will have the opportunity to do a thorough assessment of resources, perform case prioritisation and put all the structures in place for the recovery plan to function properly once initiated. This planning phase will also provide an opportunity for nurses, anaesthetists and ICU staff to have a brief period of recuperation.19
Service organisation
Both major and minor changes to regional and local hospital organisation structures have been proposed to improve the safety and efficiency of elective surgery. Local strategies include extending elective theatre time to weekends and longer working days in the week, provided there are enough resources including staffing to provide this service.12 Another recommendation is to expand ambulatory or day case surgery capacity as much as possible, as it uses fewer resources and reduces the risk of inpatient COVID-19 exposure.9,14,19 Within the hospital itself, COVID-19 patients should be separated from COVID-19 negative cases by using separate floors, buildings or even hospitals.13,20 A regional strategy that has been proposed is to transfer some of the procedures from a main academic centre to secondary level hospitals. These hospitals may have more capacity at certain phases of the pandemic than major centres, where high care/ICUs are still saturated with COVID-19 cases.21 The surgical expertise of the secondary level centres can be temporarily expanded to cope with the specialised cases.
Another promising local strategy is to set up a dedicated unit for major elective surgery. Huddy et al. described such a unit as a self-contained "cold bubble within a contaminated hospital" with theatres and ward beds located in a single area, separate from the main hospital.22 The ward staff in this unit were excluded from the main hospital and underwent weekly COVID-19 swabs. Not only did this unit report no COVID-19 transmission, but also better postoperative outcomes including reduced length of stay for colonic resections.
Perioperative
COVID-19 testing
The most important part of this phase is to ensure patient and staff safety, by reducing the risk of COVID-19 transmission as much as possible. It is estimated that there will be a substantial proportion of patients who will be asymptomatic, but contagious at the time of surgery.23 The actual testing policy will vary by institution, depending on the availability of tests and the prevalence of COVID-19 in the community. Guidance on drafting such a policy should be sought from the local infectious disease unit. The protocol of COVID-19 testing should also include guidance on the indications for postoperative patient testing, preoperative quarantine requirement, and healthcare worker screening.12,13,15,20,22 If a patient requiring elective surgery has tested COVID-19 positive, surgery should be delayed for 8-12 weeks, provided the patient's outcome is not compromised.24
Preoperative assessment
The preoperative review must include assessing for previous COVID-19 infection and complications thereof. Considering the delay in surgery, the patient may have had progression of disease or comorbidities since the previous review, which may necessitate repeating certain investigations.20 As far as possible, preoperative assessments should take place by means of a folder or telemedicine clinic, to avoid unnecessary visits to the hospital if no new workup is required before surgery.9,12,13,16,20 As part of informed consent for the procedure, clinicians must counsel patients on the risk of COVID-19 infection and its complications, as well as the expectations on them in terms of quarantine, preoperative COVID-19 testing and mask wearing during their stay.18 All patients must be strongly encouraged to get vaccinated at least two weeks prior to admission.
Theatre and postoperative recovery
Laparoscopic surgery, with its associated reduction in length of stay, is generally preferred over open surgery.15,22 From an anaesthetic perspective, much can be done to improve efficiency, reduce the risk of operating room COVID-19 exposure, and facilitate early hospital discharge. Locoregional anaesthesia is advantageous for a number of reasons.23 The first is that it avoids intubation and extubation, which are aerosol-generating procedures. The second is that many nerve blocks can be safely placed in the induction room prior to entry into the theatre. The third is that patients can bypass the often-crowded recovery room and avoid COVID-19 exposure to patients recovering from general anaesthesia. A strategy for rapid turnover lists is to have the anaesthesia and nursing team stagger cases in more than one operating room, which will enable one surgical case to be completed while the other operating room is being cleaned and prepared for the next case.23 Grouping similar cases together may facilitate this process and improve efficiency. Finally, with the restrictions placed on visitation, there should be a system of daily feedback to relatives, especially on the first postoperative day.12
Post-discharge
Logistics of discharge
As early in the process as possible, patients should be made aware that postoperative follow-up may occur virtually, over video or telephone call, unless there is a specific need to return to hospital.16 Upon discharge, patients should be educated on when to visit their local primary care facility, the surgical clinic, when to come to the emergency care (EC), and how to consult remotely if they have any postoperative issues.13 Finally, the treating team must anticipate the patient's postoperative need for a step-down facility, as such facilities have the potential for COVID-19 outbreaks.12 In such cases, the decision to proceed with surgery must be considered carefully in terms of the risks involved.
The backlog will take years to address and should be seen as more of an ultramarathon than a sprint.19 Whatever surgical recovery plan is implemented, it is important to gather data about its outcomes. This will allow for continuous improvement and adjustment, enabling increased efficiency and quality of the service.12 Therefore, tools to prospectively collect data on various aspects of the recovery strategy should be put in place early on by the LGC.
Local application of recommendations
Application of these recommendations in a specific hospital/ region depends on a number of local factors, including: the pre-existing surgical backlog, current COVID-19 prevalence, inpatient and intensive care bed occupancy, laboratory testing capacity, information technology infrastructure, and available human resources. Regardless of the strategy applied at an individual hospital level, a key component to any locoregional response is the role played by the LGC. There needs to be clear lines of communication between LGCs and hospital leaders with their counterparts in neighbouring areas, as well as with provincial and national health management. Any decision to re-escalate service provision must be taken in consultation with the National Department of Health to ensure a low likelihood of resurgence during recovery efforts.25
Conclusion
Surgical service recovery from the COVID-19 pandemic presents many challenges, especially in LMICs. However, the challenges faced also present an opportunity to assess and improve the efficiency of surgical care. There are millions of patients worldwide that continue to suffer pain and disability due to postponed elective lists; the surgical fraternity owes it to them to design and implement both effective and sustainable surgical recovery plans.
Conflict of interest
The author declares no conflict of interest.
Funding source
No funding was required.
Ethical approval
University of Cape Town Research Ethics Committee approval for narrative reviews not required.
ORCID
D Nel https://orcid.org/0000-0002-3265-1049
REFERENCES
1. COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107(11):1440-9. https://doi.org/10.1002/bjs.11746. [ Links ]
2. Chu KM, Marco J, Bougard H, et al. Estimating the surgical backlog from the COVID-19 lockdown in South Africa: a retrospective analysis of six government hospitals. S Afr Med J. 2021;111(7):685-8. https://doi.org/10.7196/SAMJ.2021.v111i7.15686. [ Links ]
3. Laas DJ, Farina Z, Bishop DG. Effect of COVID-19 pandemic decisions on tertiary-level surgical services in Pietermaritzburg, KwaZulu-Natal Province, South Africa. S Afr Med J. 2020;0(0):13182. https://doi.org/10.7196/SAMJ.2020.v110i2.15332. [ Links ]
4. Fu SJ, George EL, Maggio PM, et al. The consequences of delaying elective surgery: surgical perspective. Ann Surg. 2020;272(2):e79-e80. https://doi.org/10.1097/SLA.0000000000003998. [ Links ]
5. Billig JI, Sears ED. The compounding access problem for surgical care: innovations in the post-COVID era. Ann Surg. 2020;272(2):e47-e48. https://doi.org/10.1097/SLA.0000000000004085. [ Links ]
6. Mayosi BM, Benatar SR. Health and health care in South Africa - 20 years after Mandela. N Engl J Med. 2014;371(14):1344-53. https://doi.org/10.1056/NEJMsr1405012. [ Links ]
7. Chu KM, Smith M, Steyn E, et al. Changes in surgical practice in 85 South African hospitals during COVID-19 hard lockdown. S Afr Med J. 2020;110(9):916-9. https://doi.org/10.7196/SAMJ.2020.v110i9.15014. [ Links ]
8. Boffa DJ, Judson BL, Billingsley KG, et al. Pandemic recovery using a COVID-minimal cancer surgery pathway. Ann Thorac Surg. 2020;110(2):718-24. https://doi.org/10.1016/j.athoracsur.2020.05.003. [ Links ]
9. Al-Shamsi HO, Alhazzani W, Alhuraiji A, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) Pandemic: an international collaborative group. Oncologist. 2020;25(6):e936-45. https://doi.org/10.1634/theoncologist.2020-0213. [ Links ]
10. Elanko A, Khan J, Hamady ZZ, Malik H. Cancer surgery sustainability in the light of COVID-19 pandemic. Eur J Surg Oncol. 2020;46(6):1174-5. https://doi.org/10.1016/j.ejso.2020.05.018. [ Links ]
11. Phillips N. The coronavirus is here to stay - here's what that means. Nature. 2021;590(7846):382-4. https://doi.org/10.1038/d41586-021-00396-2. [ Links ]
12. American College of Surgeons - local resumption of elective surgery guidance [Internet]. Published 2020. Available from: https://www.facs.org/COVID-19/clinical-guidance/resuming-elective-surgery. Accessed 6 Sept 2021. [ Links ]
13. Royal College of Surgeons - recovery of surgical services during and after COVID-19 [Internet]. Published 2020 May 26, updated 2020 Dec 16. Available from: https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/. Accessed 6 Sept 2021. [ Links ]
14. American College of Surgeons Joint Statement - roadmap for maintaining essential surgery during COVID-19 pandemic [Internet]. Published 2020 Nov 23. Available from: https://www.facs.org/COVID-19/clinical-guidance/nov2020-roadmap. Accessed 6 Sept 2020. [ Links ]
15. Olson MT, Triantafyllou T, Singhal S. Resumption of elective surgery during the COVID-19 pandemic: what lessons can we apply? Eur Surg. 2020:52(4):190-2. https://doi.org/10.1007/s10353-020-00645-0. [ Links ]
16. Diaz A, Rahmanian A, Pawlik TM. COVID-19: the road to recovery. Am J Surg. 2020;220(3):561-5. https://doi.org/10.1016/j.amjsurg.2020.05.024. [ Links ]
17. Prachand VN, Milner R, Angelos P, et al. Medically necessary, time-sensitive procedures: scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. J Am Coll Surg. 2020;231(2):281-8. https://doi.org/10.1016/jjamcollsurg.2020.04.011. [ Links ]
18. Chu K, Owolabi E, Smith M, et al. Establishing a South African national framework for COVID-19 surgical prioritisation. S Afr Med J. 2021;111(5):426-31. https://doi.org/10.7196/SAMJ.2021.v111i5.15603. [ Links ]
19. Price J, Sheraton T, Self R, Cook TM. The need for safe, stable and sustainable resumption of planned surgery in an era of COVID-19. Anaesthesia. 2021;76(7):875-8. https://doi.org/10.1111/anae.15470. [ Links ]
20. Odejinmi F, Clark TJ, Mallick R. Getting back to business: considerations for restarting non-cancer gynaecological surgery following the COVID-19 peak. Facts Views Vis Obgyn. 2020;12(2):119-27. [ Links ]
21. Aubrion A, Alves A, Helye JP, Roupie E, Guittet L. Maintaining elective surgery capacity while freeing up resuscitation capacity: the challenge of COVID-19 epidemic resumption. Br J Surg. 2021;108(4):e156-7. https://doi.org/10.1093/bjs/znab006. [ Links ]
22. Huddy JR, Freeman Z, Crockett M, et al. Establishing a "cold" elective unit for robotic colorectal and urological cancer surgery and regional vascular surgery following the initial COVID-19 surge. Br J Surg. 2020;107(11):e466-7. https://doi.org/10.1002/bjs.11922. [ Links ]
23. Dexter F, Elhakim M, Loftus RW, Seering MS, Epstein RH. Strategies for daily operating room management of ambulatory surgery centres following resolution of the acute phase of the COVID-19 pandemic. J Clin Anesth. 2020;64:109854. https://doi.org/10.1016/j.jclinane.2020.109854. [ Links ]
24. Kovoor JG, Scott NA, Tivey DR, et al. Proposed delay for safe surgery after COVID-19. ANZ J Surg. 2021;91(4):495-506. https://doi.org/10.1111/ans.16682. [ Links ]
25. Western Cape Government. COVID-19 outbreak response guidelines [Internet]. Published 2020 Apr 30. Available from: https://www.westerncape.gov.za/assets/departments/health/h83_2020_covid-19_covid_critical_care_triage_and_decision_tool.pdf. Accessed 18 Dec 2021. [ Links ]
 Correspondence:
Correspondence:
D Nel
Email: danielnel87@gmail.com
Addendum A: Phased recovery approach16
Addendum B: Adaptation of MeNTS by Chu et al.18
Risk calculator
H ow to use the scoring system:
1. Faculty readiness-pandemic score: to be competed weekly/monthly by designated hospital team to create the Adjustment facility7 scale
2. Adjusted facility scale: guideline for proceeding to surgery based on individual patient risk assessment
3. Individual patient risk assessment: score based on patient, disease and procedure factors















