Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.2 Cape Town Jun. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3738
HERNIA SURGERY
Chronic groin pain in Desarda versus Lichtenstein hernia repair - a randomised controlled study
AS GaurI; N SharmaII; PK GargIII
IDepartment of General Surgery, University College of Medical Sciences, India
IIDepartment of General Surgery, All India Institute ofMedical Sciences Jodhpur, India
IIIDepartment of Surgical Oncology, Shri Guru Ram Rai Institute of Medical and Health Sciences and Shri Mahant Indiresh Hospital, India
ABSTRACT
BACKGROUND: Chronic pain after inguinal hernia repair is a common complication. This study compared the difference between Desarda repair and Lichtenstein repair for inguinal hernia in chronic groin pain.
METHODS: One hundred patients with unilateral uncomplicated inguinal hernia were randomised to either Desarda repair (n = 50) or Lichtenstein repair (n = 50) under local anaesthesia and were evaluated for pain postoperatively. Operative time, surgical complications, time to return to normal gait and work, and overall patient satisfaction were recorded. The patient was blinded to the procedure. Any pain at three months (numerical rating scale 1 or more) was considered chronic pain.
RESULTS: Mean operation time was approximately 5 minutes less for Desarda (p = 0.33). There was no significant difference in terms of pain level postoperatively between Lichtenstein and Desarda groups. Twenty-two (44%) patients in the Lichtenstein group had chronic pain, and twenty-one (45.7%) patients had chronic pain in the Desarda group (p = 0.871). No significant difference was observed in haematoma formation, wound infection, recurrence rate, seroma, or foreign body sensation. The mean time for patients to return to normal gait was approximately 0.5 day earlier for the Desarda group (p = 0.29). The mean time for patients to return to normal work was comparable (p = 0.99). Desarda group had a slightly higher satisfaction rate than the Lichtenstein group (9.1%).
CONCLUSION: Desarda repair is not inferior to Lichtenstein repair in the short-term concerning complications or pain.
Keywords: herniorrhaphy, hernia, inguinal hernia, numerical rating scale, postoperative pain
Introduction
The incidence and prevalence of inguinal hernia are not precisely known but are estimated at 1.7%. The lifetime risk of a person requiring inguinal hernia surgery is 27% in men and 3% in the case of women.1
In 1987, Lichtenstein described reinforcement of the posterior wall using a mesh resulting in tension-free repair. Today this method is widely used owing to its ease of application and lower recurrence rates.2 However, many mesh-related complications have been noted in clinical practice, including infection, pain, foreign body sensation, seroma, mesh rejection, mesh migration, adhesions, fibrosis, calcification, and thrombosis.3 To prevent these complications, Desarda in 2001 described a technique of tissue repair based on the concept of providing a robust, mobile and physiologically dynamic posterior inguinal wall.4
Some randomised controlled trials (RCTs) have evaluated Desarda repair with Lichtenstein repair and reported promising results.56 This RCT was aimed at comparing the clinical outcomes of the standard open mesh-based Lichtenstein method with the Desarda method for the treatment of inguinal hernia.
Materials and methods
This two-arm parallel-group RCT was carried out in a tertiary care teaching hospital in North India from November 2016 to April 2018 after clearance from the Institutional Ethics Committee and submission of the protocol to the University. The study could not be registered onto a database of randomised studies due to technical problems. All male patients with unilateral reducible inguinal hernia aged between 18 to 65 years with American Society of Anesthesiologists (ASA) score 1-2 and in possession of a mobile phone were considered for inclusion in the study. Patients with BMI > 25 kg/m2 were excluded from the study owing to the anticipated difficulty in performing the procedures under local anaesthesia. Patients with a complicated hernia, i.e., irreducible obstructed or strangulated hernia, patients with coagulopathy, patients who had received analgesic 24 hours before the proposed operation, and patients with contraindication to spinal anaesthesia were excluded.
We recruited 100 patients into two equal groups. Assuming 25% of patients in Lichtenstein mesh hernia repair develop chronic pain compared to 5% patients undergoing Desarda repair, a sample size of 49 in each arm was calculated using G*Power 3.1 to detect a clinically significant difference in chronic groin pain of 20% with type I error of 5% and 80% power.7
The randomisation sequence generated from www. randomization.com was sealed in serially numbered opaque envelopes, and one day before surgery an envelope was opened and the operative procedure was decided. The patient was blinded to the procedure for the first three months. Informed consent was obtained from the patients, and the details of both surgical procedures were informed to the patient before inclusion in the study.
The Desarda repair was done as described by Desarda.5 Through a regular oblique inguinal incision; the external oblique aponeurosis was exposed. The external oblique aponeurosis was cut in line with the upper crux of the superficial ring. That left the thinned-out portion in the lower leaf. The hernia sac was dealt with in the usual fashion. The medial leaf of the external oblique aponeurosis was sutured with the inguinal ligament from the pubic tubercle to the abdominal ring using 1-0 polypropylene interrupted sutures. The first two sutures were taken in the anterior rectus sheath, where the external oblique aponeurosis is fused with it. The last suture was taken to sufficiently narrow the abdominal ring without constricting the spermatic cord. Each suture was passed first through the inguinal ligament, then the transversalis fascia and then the external oblique aponeurosis.
A splitting incision was taken in this sutured medial leaf of the external oblique aponeurosis, partially separating a strip with a width equivalent to the gap between the muscle arch and the inguinal ligament. The splitting incision was extended medially up to the pubic symphysis and laterally 1-2 cm beyond the deep inguinal ring. The medial insertion and lateral continuation of this strip were kept intact. The upper free border of the strip was sutured to the internal oblique or conjoined muscle with 1-0 polypropylene interrupted sutures. This resulted in the strip of external oblique aponeurosis being placed behind the cord to form a new posterior wall of the inguinal canal. The lateral leaf of the external oblique aponeurosis was then sutured to the newly formed medial leaf of the external oblique aponeurosis in front of the cord using 1-0 polypropylene interrupted sutures.
The Lichtenstein repair was carried out using the following steps. Through a regular oblique inguinal incision, the external oblique aponeurosis was exposed. The external oblique was opened and its lower leaf was freed from the spermatic cord. The upper leaf was then separated from the internal oblique muscle until internal oblique aponeurosis was reached. The cord, along with its cremasteric covering, was separated from the inguinal canal floor and the pubic bone for approximately 2 cm beyond the pubic tubercle. The hernial sac was dealt with in the usual manner. The mesh of size 7.5 cm x 15 cm was cut in a footprint tracing fashion. The lower sharper angle was sutured with 2-0 polypropylene suture to insertion of rectus sheath to the pubic bone, overlapping the bone by 1-2 cm avoiding the periosteum of the bone. The lower sharper angle of the mesh was fitted between the rectus and the inguinal ligament.
The upper wider angle was spread over the rectus sheath. The suture was continued up to four passages continuously to attach the patch of the mesh to the inguinal ligament up to a point just lateral to the internal ring. The slit was made onto the lateral part of the mesh to make one wider (upper 1/4th) tail and another narrow (lower 1/4th) tail. With the cord lifted upward, the wider tail was passed beneath the cord. A wider tail was then placed over the narrow tail. The cord thus was positioned between the two tails. The lower end of both the tails was then sutured to the inguinal ligament just lateral to the completion of the continuous suture knot leaving ample space for the cord to pass. With the cord retracted downwards, the wider upper edge was sutured to the internal oblique aponeurosis just lateral to the internal ring and to the rectus sheath with non-absorbable monofilament suture. The excess patch of the mesh 5 cm lateral to the internal ring was trimmed. The external oblique aponeurosis was then closed with an absorbable (2-0 polyglactin 910) suture over the cord.6
The ilioinguinal and iliohypogastric nerves were preserved each time they were encountered. Special attention was paid so as not to include these into sutures or mesh.
The primary outcome measure was chronic groin pain using an 11-point numerical rating scale (NRS 11)8 score at three months postoperatively. Secondary outcome measures comprised operative time, haematoma formation, wound infection, early recurrence within three months, seroma formation, foreign body sensation, days to return to normal gait, days to return to normal work, overall satisfaction using Likert scale,9 and postoperative pain scores using NRS scoring at 6 hours, day 1, day 7 and 1 month postoperatively. The patient was blinded to the procedure for the first three months.
The case definition of chronic pain is "pain lasting for three months or more" as per the International Association of the Study of Pain (IASP).10
Data were analysed using SPSS statistical software. Student t-test was used for comparison of quantitative data with the normal distribution. Mann-Whitney U test was used to compare numerical data without normal distribution. The chi-square test (χ2) test was used to compare the proportion of patients with chronic pain and Fisher exact test to compare the proportion of patients with haematoma, wound infection, early recurrence, seroma, and foreign body sensation postoperative complications between the study groups. A p-value of < 0.05 was taken as significant.
Results
This RCT aimed to compare Desarda and Lichtenstein repair outcomes under local anaesthesia in a teaching hospital in New Delhi from November 2016 to November 2018. Figure 1 shows the study CONSORT flow diagram.
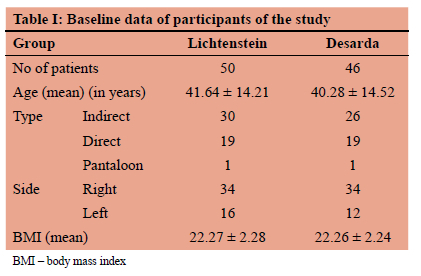
Table I shows the baseline demographic data of participants of the study. The groups were comparable in terms of age, BMI and type of hernia.
In our RCT, 100 cases that met the inclusion criteria were randomly allotted in a 1:1 manner to Desarda and Lichtenstein group. In 50 cases, Lichtenstein repair was performed. Of the 50 patients allocated to the Desarda group, four had a conversion to Lichtenstein repair during surgery because the external oblique aponeurosis being thin was getting cut through on suturing. All cases were successfully performed under local anaesthesia with no intraoperative complications.
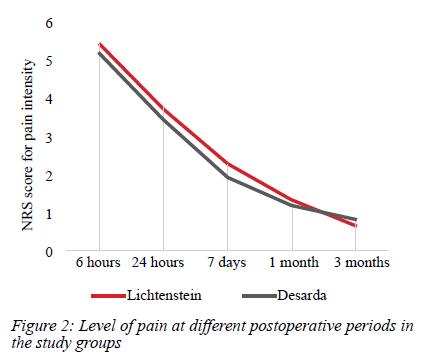
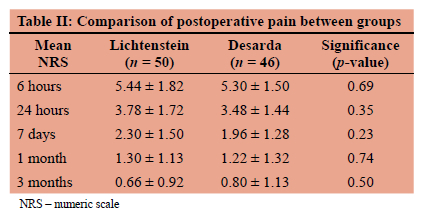
There was no significant difference between the level of pain in the Lichtenstein group and the Desarda group at any time in the postoperative period. However, the pain was
maximal early in the postoperative period and decreased in both groups over the next few months (Figure 2).
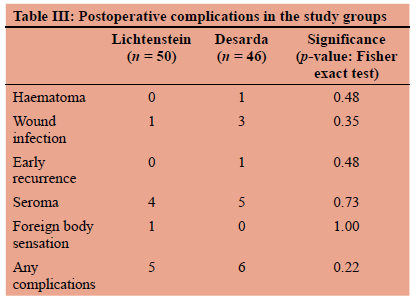
There was no significant difference between the number of patients who developed postoperative complications in the Lichtenstein group and Desarda group (Table II). There was no significant difference in operating time, return to work or return to normal gait in the Lichtenstein group and Desarda group (Table III).
Any patient who had a score > 1 on an 11-point numeric scale (NRS 11) beyond three months of surgery was considered to have chronic pain. Of the 50 patients who underwent Lichtenstein operation, 22 (44%) had some pain at three months, while 21/46 (45.7%) patients who underwent successful Desarda repair had pain. This difference was not statistically different (Table IV). The proportions were comparable even when we analysed at a cut-off NRS of 3/10. Desarda group had a higher satisfaction rate (89.1%) than the Lichtenstein group (80%).
Discussion
Conventional mesh-based inguinal hernia repairs such as Lichtenstein repair provide good outcomes. But mesh-related complications increase the morbidity of the patient and the chance of developing chronic groin pain. Non-mesh repairs prevent these complications but are often reported to be less efficacious. Desarda repair is a new tissue-based repair technique, which is reported to be as good as mesh-based repairs but without complications of mesh and chronic groin pain.
In our study, we found that in the Lichtenstein group, 22/50 (44%) patients had chronic pain, and 21/46 (45.7%) patients had chronic pain in the Desarda group (p = 0.871). In most studies, there was no significant difference in terms of chronic pain between these two techniques.1112 However, Desarda himself reported that there was no chronic pain after Desarda repair.13 It was expected that Desarda repair would have fewer patients with chronic inguinal pain as there is less likelihood of mesh-related complications like nerve entrapments and fibrosis. We also did not find a significant difference between the Lichtenstein and Desarda groups regarding the proportion of patients having chronic pain.
We found that pain intensity was not significantly different at 6 hours, 24 hours, day 7, 1 month, and three months after operation between Lichtenstein and Desarda group. Similar results were reported by Manyilirah et al., Emile et al., and Youssef et al.41114 However, the Desarda group had less pain in a study reported by Gedam et al.15 The hypothesis that pain scores would be higher after Lichtenstein repair due to extensive dissection needed to place mesh was rejected in this study. Although the pain scores were less in the Desarda group, the difference was not significant. The difference in mean pain scores between groups was also not clinically significant.
As more dissection is needed in Lichtenstein repair as compared to Desarda to create space for placing the mesh, it was thought that there would be higher chances of haematoma, seroma and wound infection after Lichtenstein operation. In our study, no significant difference was observed in these complications. Only one (2.2%) patient from the Desarda group had developed a haematoma, and none was seen in the Lichtenstein group (p = 0.48). Various studies reported similar results.11
It was expected that mesh placement would result in the sensation of a foreign body in the inguinal region of patients who underwent Lichtenstein repair. In our study, there was no significant difference in foreign body sensation; only one patient complained of foreign body sensation in the Lichtenstein group. Similar results are shown in studies by Szopinski et al., Youssef et al., and Ge et al.121416
We thought that Lichtenstein repair would have more complications due to more dissection and mesh-related complications than Desarda repair, as reported by Emile et al.11 However, the overall short-term postoperative complication rate for the Desarda group was not different from Lichtenstein. Similar results were reported in other studies.11,16
Many studies reported less operative time for Desarda repair attributed to the lack of extensive dissection needed in the repair.24 Our mean duration of surgery was approximately 5 minutes less for Desarda repair than Lichtenstein repair, but this difference is slight and has neither clinical importance nor statistical difference. This is similar to results reported by Gedam et al. and many others.1115
The mean time for patients to return to normal gait was approximately half a day earlier for the Desarda group than the Lichtenstein group and had no significant difference. Manyilirah et al. and Ge et al. reported similar results.416 Youssef et al. reported a significantly earlier return to normal gait for the Desarda group as it had less pain scores and fewer early complications.1214 In our study, the mean time for patients to return to normal work was similar for the Lichtenstein and Desarda groups. Szopinski et al. and Youssef et al. reported similar results.12,14 Our results contradicted studies that reported that the time taken to return to normal activity was significantly lesser for the Desarda group.11,15 But we observed no difference as there was no significant difference in postoperative pain scores, complication rates and time to return to normal gait in our study.
We observed one recurrence in the Desarda group and none in the Lichtenstein group at three months, which was not significantly different. Similar results were reported in other studies.11,16 However, long-term follow-up is needed to know more about the long-term recurrence following these two techniques.
Desarda group had a 9.1% higher satisfaction rate than the Lichtenstein group, which is not significantly different between the two groups.
Very few studies have described the outcomes of Desarda repair in the emergency setting. Since it is a tissue-based repair, it can be used where contamination is present and chances of mesh infection are high. Desarda repair has less incidence of recurrence than other tissue-based methods in the emergency setting.17
We recruited 100 patients to evaluate if the difference in chronic pain was as large as previously cited. This study had a limitation as it was not powered to detect small differences in chronic pain between groups. It is possible that the small differences in the group could attain statistical significance had the sample size been larger. However, the effect size of the difference is not likely to have been clinically important.
Desarda repair was not considered suitable in all patients. We found that the weak external oblique could not hold the sutures and got torn during our attempts at Desarda repair in four patients, and we decided to perform Lichteinsein repair in them.
Conclusion
We conclude that short-term outcomes of Desarda repair are as good as Lichtenstein repair in patients whose external oblique aponeurosis can hold sutures well. The frequency of chronic pain after Desarda repair is not less than after Lichtenstein repair at 3 months after surgery.
Desarda repair may have a particular advantage in patients undergoing emergency operations, where the risk of mesh infection is considered particularly high since it obviates the need to insert a prosthetic mesh.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Approval for the study was obtained from the Institutional Research Ethics Committee Human Research, University College of Medical Science, University of Delhi.
ORCID
AS Gaur https://orcid.org/0000-0003-3092-7280
N Sharma https://orcid.org/0000-0003-2067-7329
PK Garg https://orcid.org/0000-0001-9760-5484
REFERENCES
1. Kingsnorth A, LeBlanc K. Hernias - inguinal and incisional. Lancet. 2003;362(9395):1561-71. https://doi.org/10.1016/S0140-6736(03)14746-0. [ Links ]
2. Zulu HG, Mewa Kinoo S, Singh B. Comparison of Lichtenstein inguinal hernia repair with the tension-free Desarda technique - a clinical audit and review of the literature. Trop Doct. 2016;46(3):125-9. https://doi.org/10.1177/0049475516655070. [ Links ]
3. Falagas ME, Makris GC. Mesh-related infections after hernia repair. In: Schumpelick VFRJ, editor. Hernia Repair Sequelae. Springer: Berlin, Heidelberg; 2010. p. 97-102. https://doi.org/10.1007/978-3-642-11541-7_13. [ Links ]
4. Manyilirah W, Kijjambu S, Upoki A, Kiryabwire J. Comparison of non-mesh (Desarda) and mesh (Lichtenstein) methods for inguinal hernia repair among black African patients: a short-term double-blind RCT. Hernia. 2012;16(2):133-44. https://doi.org/10.1007/s10029-011-0883-0. [ Links ]
5. Desarda MP. New method of inguinal hernia repair - a new solution. ANZ J Surg. 2001;71(4):241-4. https://doi.org/10.1046/j.1440-1622.2001.02092.x. [ Links ]
6. Amid PK. Lichtenstein tension-free hernioplasty - its inception, evolution, and principles. Hernia. 2004;8(1):1-7. https://doi.org/10.1007/s10029-003-0160-y. [ Links ]
7. Lange JFM, Meyer VM, Voropai DA, et al. The role of surgical expertise with regard to chronic postoperative inguinal pain (CPIP) after Lichtenstein correction of inguinal hernia - a systematic review. Hernia. 2016;20(3):349-56. https://doi.org/10.1007/s10029-016-1483-9. [ Links ]
8. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain - visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S240-S252. https://doi.org/10.1002/acr.20543. [ Links ]
9. Likert R. Public opinion polls. Sci Am. 1948;179(6):7-11. https://doi.org/10.1038/scientificamerican1248-7. [ Links ]
10. The HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22(1):1-165. https://doi.org/10.1007/s10029-017-1668-x. [ Links ]
11. Emile SH, Elfeki H. Desarda's technique versus Lichtenstein technique for the treatment of primary inguinal hernia: a systematic review and meta-analysis of randomised controlled trials. Hernia. 2018;22(3):385-95. https://doi.org/10.1007/s10029-017-1666-z. [ Links ]
12. Szopinski J, Dabrowiecki S, Pierscinski S, et al. Desarda versus Lichtenstein technique for primary inguinal hernia treatment - 3-year results of a randomised clinical trial. World J Surg. 2012;36(5):984-92. https://doi.org/10.1007/s00268-012-1508-1. [ Links ]
13. Desarda MP. No-mesh inguinal hernia repair with continuous absorbable sutures - a dream or reality? (A study of 229 patients). Saudi J Gastroenterol. 2008;14(3):122-7. https://doi.org/10.4103/1319-3767.41730. [ Links ]
14. Youssef T, El-Alfy K, Farid M. Randomised clinical trial of Desarda versus Lichtenstein repair for treatment of primary inguinal hernia. Int J Surg. 2015;20:28-34. https://doi.org/10.1016/j.ijsu.2015.05.055. [ Links ]
15. Gedam BS, Bansod PY, Kale VB, Shah Y, Akhtar M. A comparative study of Desarda's technique with Lichtenstein mesh repair in treatment of inguinal hernia - a prospective cohort study. Int J Surg. 2017;39:150-5. https://doi.org/10.1016/j.ijsu.2017.01.083. [ Links ]
16. Ge H, Liang C, Xu Y, Ren S, Wu J. Desarda versus Lichtenstein technique for the treatment of primary inguinal hernia - a systematic review. Int J Surg. 2018;50:22-7. https://doi.org/10.1016/j.ijsu.2017.11.055. [ Links ]
17. Hussain A, Mehsam S, Ali M, Rasul S, Parveen S, Memon A. Emergency inguinal hernia repair: comparison of Desarda's versus darning technique. J Ayub Med Coll Abbottabad. 2017;29(4):551-3. [ Links ]
 Correspondence:
Correspondence:
email: drabhaygaur@live.com














