Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.2 Cape Town Jun. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3750
BREAST
Impact of COVID-19 on breast cancer diagnostic and surgical services at a South African academic hospital
T van WyngaardI; L CairncrossI; S MaswimeII; L RoodtI; F MalherbeI
IBreast and Endocrine Unit, Division of General Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
IIDivision of Global Surgery, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: The purpose of the study was to describe the impact of the COVID-19 pandemic on diagnostic and surgical breast cancer services at Groote Schuur Hospital (GSH) and affiliated hospitals.
METHODS: All patients, newly diagnosed, awaiting surgery, and listed for neoadjuvant chemotherapy (NACT) by the breast surgical service from 23 March-23 June 2020 were included. A historic control was used where appropriate consisting of patients presenting in the same period in 2019. Clinic attendance records and surgical waiting lists were used to identify patients in the three months and data were extracted from hospital records including hospital admission records and surgical operative notes.
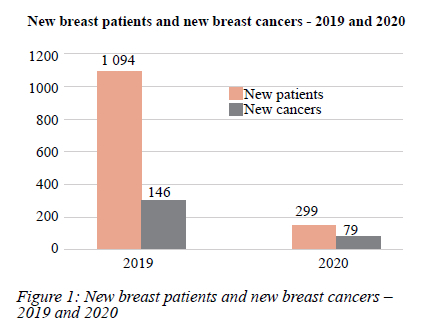
RESULTS: The number of patients who presented with a new breast symptom to the diagnostic breast clinic decreased from 1 094 in 2019 to 299 in 2020, representing a 72.6% decrease. Telemedicine use as a function of the total follow-ups increased from 53% (n = 1 350) in 2019 to 75% (n = 735) in 2020. The overall number of new breast cancers diagnosed decreased from 146 in 2019 to 79 in 2020, but the proportion of patients seen with a new breast symptom who were diagnosed with breast cancer increased from 13% (n = 1 094) in 2019 to 26% (n = 299) in 2020. Eighteen per cent (n = 105) fewer breast cancer surgeries were performed in 2020 compared to 2019, with immediate breast reconstructive procedures representing the largest decrease of 40%.
CONCLUSION: The impact of COVID-19 on breast cancer services has been both at the diagnostic level and in delays to surgery. A new online referral system improved referral efficacy translating to more cancers being diagnosed as a function of total referrals. The drop in absolute numbers of cancer diagnoses, however, represents an unmet health need. An expansion of our telemedicine service mitigated COVID risk in the outpatient setting. The greatest impact on our treatment decisions was seen in the cohort of patients placed on neo-adjuvant endocrine therapy (NET). We saw a global decrease in breast surgeries performed, with the greatest decrease being in reconstructions.
Keywords: breast cancer, COVID, breast diagnostic services, pandemic, breast cancer management during COVID
Introduction
Breast cancer is the most common cancer amongst women worldwide and the leading cause of cancer-related death. Women from low- to middle-income countries (LMIC) are particularly affected by resource limitations.1 Maintaining an optimal breast cancer service whilst mitigating the risks associated with COVID-19 in already strained clinical services has been a challenge for health systems throughout the world. Recommendations for the prioritisation of breast cancer care during the pandemic as well as strategies for the resumption of breast cancer services have been published.23 These recommendations are focused on balancing individual cancer risk against COVID-19 risk by stratifying patients according to tumour size and tumour biology. Although these recommendations do suggest strategies for prioritising cancer care in a resource-limited setting, there is a scarcity of data published from LMICs where this balance is particularly challenging.14-6
The impact of COVID-19 on breast cancer services has been both at the diagnostic level and in delays to surgery. Health seeking behaviour of patients has changed mainly due to fear of contracting COVID-19, and this has led to delays in diagnosing breast cancer. The impact on outpatient services, the primary portal of entry for women with symptoms of breast cancer into the health system, has been significant.78
In our setting, access to diagnostic clinics was limited, both by travel restrictions imposed by hard lockdowns and by the restriction of patient numbers in a bid to limit the spread of the infection. In many centres, outpatient department (OPD) staff were re-allocated to non-patient contact areas according to risk profile or placed in self-quarantine due to exposure or infection, leading to significant staff shortages. Diagnostic procedures were limited due to restrictions placed on radiological investigations. Elective operative procedures for cancer patients were delayed in many centres to prioritise resources.9
Like many other clinical services, it was necessary to implement significant and rapid changes to our breast diagnostic and surgical service at the start of the COVID-19 pandemic and associated lockdown. Our diagnostic service changed from a walk-in clinic to a website-based referral system and our existing telemedicine service was expanded to meet the social distancing requirements of the lockdown restrictions to ensure patient safety. With significant pressure on our surgical theatre slates, decisions about triage and prioritisation were necessary (for example, postponement of reconstructive surgery) and the individual COVID-19 risk for elderly patients and those with comorbidities had to be factored into clinical management decision making. These decisions were made with the best available knowledge and health resources at the time.
Our study describes the impact these decisions had on diagnostic and surgical breast cancer services at Groote Schuur and affiliated hospitals as well as the strategies implemented to mitigate the impact on quality patient care.
Methods
The study was conducted at Groote Schuur Hospital (GSH) a large tertiary academic complex with 893 beds located in Cape Town, South Africa.
The impact of the COVID-19 pandemic on diagnostic and surgical breast cancer services at GSH and affiliated hospitals was assessed by comparing 3 months in 2019 with a corresponding 3-month period during COVID-19 lockdown in 2020. The effect on the breast diagnostic services included the difference in the number of women presenting to the clinic with new onset of breast symptoms (new patients); changes to the number of women diagnosed with breast cancer (new cancers) and differences in the use of telemedicine for follow up of patients (follow-up visits). The number and types of breast cancer operations as well as the number of breast reconstructions performed were noted. Attention was paid to and the changes in clinical management for individual patients including increased surgical delays and increased use of neoadjuvant therapy.
Clinic attendance records and surgical waiting lists were used to identify patients in the relevant three-month periods in 2019 and 2020. Data were collected by reviewing hospital records including hospital admission records and surgical operative notes. Operative waiting time was reported in weeks and defined as the time from the decision to operate to the date of the surgical procedure. Surgical procedures were recorded as breast-conserving surgery (BCS); mastectomy; sentinel lymph node biopsy (SLNB) and axillary lymph node dissection (ALND). BCS included all procedures with a partial breast excision including therapeutic mammaplasty. Mastectomy was defined as the complete removal of all breast glandular tissue.
Inclusion criteria: All patients managed by the breast surgical service between 23 March-23 June in 2019 and in 2020. New cancers diagnosed during this period, patients awaiting surgery at the start of the period and patients listed for neoadjuvant chemotherapy (NACT) at the beginning of the period were included.
Exclusion criteria: Patients not eligible for surgery due to metastatic disease and patients assessed as unfit for breast cancer surgery due to anaesthetic concerns.
Results
Impact on the breast diagnostic service
For the three months assessed, the number of patients who presented with a new breast symptom to the breast diagnostic clinic decreased from 1 094 in 2019 to 299 in 2020, representing a 72.6% decrease. There was also a decrease in the overall number of new breast cancers diagnosed, dropping from 146 in 2019 to 79 in 2020 (45.8% decrease). However, the proportion of new patients seen who were then diagnosed with breast cancer increased from 146/1 094 (13%) in 2019 to 79/299 (26%) in 2020 (Figure 1).
The proportion of patients whose follow-up appointment was through telemedicine increased significantly between 2019 and 2020. Telemedicine use as a proportion of the total follow-ups increased from 53% (718/1 350) in 2019 to 75% (539/735) in 2020 (Figure 2).

A total of 105 patients were operated on in 2019 compared to 86 in 2020, representing 18% fewer breast cancer operations performed. There was a 9% increase in the number of mastectomies performed as a function of the total oncologic breast procedures during 2020, (72/86) as compared to 2019 (79/105) and a 9% decrease in BCS in 2020 (14/86) versus 2019 (26/105). There was an increase of 6% in ALNC numbers (50/98 in 2019 and 49/86 in 2020) and a decrease of 6% in SLNB numbers compared to 2019 (48/98 in 2019 and 37/86 in 2020) (Figure 3). Immediate breast reconstructive procedures decreased by 40% between the 2019 and 2020 study periods.
Impact on clinical management of individual patients
Sixty-two per cent of patients (89/143) had a clinical management course that deviated from standard local protocol. Of these 89 patients, 21 had their surgery expedited, 12 had operations postponed due to their COVID risk; five were delayed due to a lack of theatre time, 23 received NACT, and 28 received neoadjuvant endocrine therapy (NET). NET was prescribed for patients with early-stage luminal breast cancers either as part of a triage process in the face of limited theatre access or because they were deemed to be at high risk of severe disease if exposed to COVID-19 in the perioperative period. Twenty-three luminal B patients received NACT as a change in treatment. Of these, 11 were luminal B HER2 negative patients with a high Ki67 level and 12 were luminal B HER2 positive. At the start of the pandemic, our NACT protocol was changed to include all HER2 expressed patients and not just non-luminal HER2 positive and triple-negative patients. (We do not have HER2 antibody therapy available in our setting.) Non-luminal HER2 expressed and triple-negative patients also received NACT.
According to pre-COVID protocols, NACT was administered to 34/36 patients. Two patients were excluded from NACT based on age and comorbidities.
The waiting time between the multidisciplinary team (MDT) decision and surgery was comparable to 2019 waiting times and the length of time between completion of NACT and surgery was unchanged. However, overall, the time to surgery from MDT decision to operate increased by 33% from 10 weeks in 2019 to 15 weeks in 2020. This was partly mitigated by the postponement of non-cancer surgery which allowed 21 breast cancer operations to be done in the first month of the lockdown period.
Discussion
Impact on diagnostic services
Very little data is available thus far regarding the quantitative impact that the COVID-19 pandemic has had on the diagnosis and management of breast cancer in LMICs.
In our breast diagnostic service, we saw significantly fewer patients (73%) during the hard lockdown period than pre-pandemic. There was also a significant (45%) reduction in the number of new breast cancers diagnosed. The fact that new cancer diagnoses did not decrease as steeply is due to our referral criteria for entry into the clinic becoming much stricter. Older patients with breast lumps were prioritised over younger patients with symptoms suggestive of benign disease such as mastalgia. As a result, the proportion of new patients diagnosed with breast cancer rose from 13% in 2019 to 26% in 2020, which represents a potentially better use of health resources if the total number of new cancers is seen to return to pre-pandemic levels. However, the almost 50% reduction in the diagnosis of breast cancer represents a significant unmet health need. An outpatient breast cancer clinic in Lombardy, Italy, reported a significant reduction in access for outpatient therapy during the period 24 February to 30 April 2019 compared to 2020 (2 974 in 2019 versus 2 590 in 2020). In this study, 63 patients delayed treatment: 38% for "pandemic fear", 18% due to travel restrictions, 13% due to self-isolation, 18% for flu syndrome other than COVID-19, and 13% for worsening of clinical conditions and death.8 We did not capture reasons for the decrease in clinic number visits in our setting, but postulate that travel restrictions, limited available transport and pandemic fear contributed.
Telemedicine, an encompassing term referring to the exchange of medical information through electronic com-munications,2 was employed as a way of reducing in-person meetings and accommodating social distancing practices. The use of our already existing telephone clinic service linked to the diagnostic breast clinic was expanded during this time.
As telephonic follow-ups increased as a function of the total number of follow-ups, in-person follow-ups were limited to those patients without a reliable contact number and those who needed clinical review.
The European Society for Medical Oncology (ESMO) recognises telemedicine as an "efficient delivery platform for deferrable healthcare services" focused on the follow-up of the stable, chronic patient.3 Its use as part of essential service provision in oncology during the pandemic is supported by the Society of Surgical Oncology.2 ESMO suggests that telemedicine should be approached in a formal fashion and form part of structured clinical work. They see telehealth as remaining part of health care in the long term and filling a service delivery niche.3
Impact on the number and types of breast surgical procedures
The risk of contracting COVID whilst in hospital should be offset by the fact that delaying oncologic surgeries may lead to disease progression and possibly irresectability. The risk-benefit ratio should be borne in mind and all decisions for delayed surgery and a shift to neoadjuvant therapies taken in the setting of MDTs.10
Almost a third of patients faced a delay to surgery with some enrolled in alternative treatment pathways to mitigate the risk of surgery and concomitant COVID-19 infection, and in others delayed due to restricted access to theatre. Overall delay to surgery increased by 33% (10 to 15 weeks).
Simple, fast operations were prioritised over more complex procedures. In 2019, the ratio of BCS to mastectomy was 1:3 and decreased to 1:5 in 2020. Much of the BCS is usually done at the tertiary hospital, yet during the pandemic, patients who were eligible for BCS were more frequently referred to peripheral hospitals and received a mastectomy due to the reduced operative capacity at GSH.
BCS lends itself to same-day discharge more so than do mastectomies.11 Enhanced recovery after surgery (ERAS) principles in breast surgery support the implementation of day-case surgeries.12 Most of the patients were admitted the day before surgery and discharged the day after surgery. We had a significant reduction in length of stay (LOS) (2 days) in 2020 compared to (5 days) in 2019 This is most likely because patient discharges were expedited as patients were discharged with their wound drains in situ. It was not our routine practice to send patients home with drains before the COVID-19 pandemic.
It is recommended that immediate reconstructive surgery during the pandemic be limited to expander placement only.2 At the peak of the pandemic, all breast reconstructions were cancelled, even the placement of expanders. This was mainly due to the plastic surgery outpatient clinic being closed, which would have made inflation of the expanders difficult.
Impact on treatment decisions: NET
The American Society of Breast Surgeons (ASBS), French Saint Paul-de-Vence (SPDV) group and the International RT network recommended early in the pandemic that luminal cancers (early or locally advanced) be treated with primary endocrine treatment and to delay surgery for 3-6 months.2 In our series, the greatest impact on treatment decisions was seen in the cohort of luminal patients placed on NET.
We used tamoxifen (a selective oestrogen receptor modulator [SERM]) due to availability and used it as a bridge to delayed surgery, as recommended by the ESMO Guidelines.3
Treatment response was monitored by clinical evaluation at the MDT as it was not feasible to monitor response using ultrasound, a more sensitive tool to assess treatment response,13 during the pandemic. By maintaining more patients on NET in the post-pandemic re-escalation period, further relief on the overburdened operating lists may be achieved. A good response to NET leads to tumour downstaging, which in turn allows for more BCS to be performed.
Study limitations
The study attempts to compare the impact of the pandemic on diagnostic and surgical services during a three-month period at the start of the pandemic in 2020 with the 2019 data collected retrospectively from clinic records. The time period was short and reflected the most severe time of the lockdown period. Some data may not have been captured making it difficult to draw firm conclusions regarding certain aspects.
Extending the study period may have given a better picture of the full impact of the pandemic.
The stage of presentation between the two years was not compared, which may have further evidence of unmet health needs during the pandemic.
The impact on broader breast oncology services would add further critical dimensions to the assessment of the effect on breast cancer patients.
Conclusion
The impact of COVID-19 on breast cancer services has been both at the diagnostic level and in delays to surgery.
We saw a relative doubling in the number of new cancers partially explained by our more efficient referral system. The lower absolute numbers of cancer patients diagnosed during the period in 2020 represents an unmet health need requiring further follow-up in the months to come.
We mitigated the risk of virus exposure in the diagnostic clinic by expanding the use of our existent telemedicine service in-line with international recommendations.
The greatest impact on treatment decisions was in the patients placed on NET. By maintaining more patients on NET in the re-escalation period, one may allow further prioritisation on overburdened operating lists. A good response to NET with tumour downstaging may allow for more BCS to be performed.
ERAS principles support the implementation of day case surgeries to which BCS lends itself. We saw a slight decrease in BCS numbers relative to mastectomies in our setting. However, supporting more BCS by upskilling surgical trainees may allow for a further decrease in LOS of individual patients and unburdening of ward capacity. We increased hospital turn-over by sending patients home with drains in situ.
In breast cancer, preventing disease progression and ensuring optimal long-term clinical outcomes should remain the standard of care. We tracked diagnostic rates and developed practical systems improvements to aid in managing patient outcomes despite dramatic changes in external circumstances.
Conflict of interest
The authors declare no conflict of interest.
Funding source
The SA MRC Midcareer scientist grant contributed to the funding of TvW and SM.
Ethical approval
Permission to conduct the study was attained from the University of Cape Town Human Research Ethics Committee (HREC REF: 594/2020). Data were entered into a password-protected database.
ORCID
TvanWyngaard https://orcid.org/0000-0001-8487-9259
L Cairncross © https://orcid.org/0000-0001-5368-9882
S Maswime © https://orcid.org/0000-0003-4013-5164
L Roodt https://orcid.org/0000-0002-0545-5413
F Malherbe © https://orcid.org/0000-0001-8910-6925
REFERENCES
1. McKenzie F, Zietsman A, Galukanda M, et al. Drivers of advanced stage at breast cancer diagnosis in the multicountry African breast cancer - disparities in outcomes (ABC-DO) study. Int J Cancer. 2018;142(8):1568-79. https://doi.org/10.1002/ijc.31187. [ Links ]
2. Hwang ES, Balch CM, Balch GC, et al. Surgical oncologists and the COVID-19 pandemic - guiding cancer patients effectively through turbulence and change. Ann Surg Oncol. 2020;27:2600-13. https://doi.org/10.1245/s10434-020-08673-6. [ Links ]
3. De Azambuja E, Trapani D, Loibl S, et al. ESMO management and treatment adapted recommendations in the COVID-19 era: Breast Cancer. ESMO Open. 2020;5(Suppl 3):e000793. https://doi.org/10.1136/esmoopen-2020-000793. [ Links ]
4. Deshmukh S, Naik S, Zade B, et al. Impact of the pandemic on cancer care - lessons learned from a rural cancer center in the first 3 months. J Surg Oncol. 2020;122(5):831-8. https://doi.org/10.1002/jso.26144. [ Links ]
5. Lombe DC, Mwaba CK, Msadabwe SC, et al. Zambia's National Cancer Centre response to the COVID-19 pandemic - an opportunity for improved care. Ecancermedicalscience. 2020;14:1051. https://doi.org/10.3332/ecancer.2020.1051. [ Links ]
6. Moustakis J, Piperidis A, Ogunrombi A. The effect of COVID-19 on essential surgical admissions in South Africa - a retrospective observational analysis of admissions before and during lockdown at a tertiary healthcare complex. S Afr Med J. 2020;110(9):910-5. https://doi.org/10.7196/SAMJ.2020.v110i9.15025. [ Links ]
7. Kruger EC, Banderker R, Erasmus RT, Zemlin AM. The impact of COVID-19 on routine patient care from a laboratory perspective. S Afr Med J. 2020;110(12):1201-5. https://doi.org/10.7196/SAMJ.2020.v110i12.15294. [ Links ]
8. Quaquarini E, Saltalamacchia G, Presti D, et al. Impact of COVID-19 outbreak on cancer patient care and treatment -data from an outpatient oncology clinic in Lombardy (Italy). Cancers (Basel). 2020;12(10):2941. https://doi.org/10.3390/cancers12102941. [ Links ]
9. Chu KM, Smith M, Steyn E, et al. Changes in surgical practice in 85 South African hospitals during COVID-19 hard lockdown. S Afr Med J. 2020;110(9):916-9. https://doi.org/10.7196/SAMJ.2020.v110i9.15014. [ Links ]
10. Belkacemi Y, Grellier N, Ghith S, et al. A review of the international early recommendations for departments organisation and cancer management priorities during the global COVID-19 pandemic - applicability in low- and middle-income countries. Eur J Cancer. 2020;135:130-46. https://doi.org/10.1016/j.ejca.2020.05.015. [ Links ]
11. Marla S, Stallard S. Systematic review of day surgery for breast cancer. Int J Surg. 2009;7(4):318-23. https://doi.org/10.1016/j.ijsu.2009.04.015. [ Links ]
12. Wahab TA, Uwakwe H, Jumah M, et al. A modified enhanced recovery after surgery (ERAS) - use and surgical outcome in breast cancer patients. J Biosci Med (Irvine). 2018;6:15-25. https://doi.org/10.4236/jbm.2018.63002. [ Links ]
13. Martí C, Sánchez-Méndez JI. Neoadjuvant endocrine therapy for luminal breast cancer treatment - a first-choice alternative in times of crisis such as the COVID-19 pandemic. Ecancermedicalscience. 2020;14:1027. https://doi.org/10.3332/ecancer.2020.1027. [ Links ]
 Correspondence:
Correspondence:
email: tirsavanwyngaard@yahoo.com














