Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.2 Cape Town Jun. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3679
BREAST
Magseed placement before neoadjuvant chemotherapy to facilitate subsequent breast-conserving surgery – a single-centre audit
F MalherbeI; L RoodtI; F NoorI; R GamieldienII; D ChettyIII; D AndersonIV; Τ ThebeIV; L CairncrossI
IDivision of General Surgery, University of Cape Town, South Africa
IIDivision of Radiology, University of Cape Town, South Africa
IIIDivision of Anatomical Pathology, University of Cape Town, South Africa
IVDivision of Radiation Oncology, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: A radio-opaque clip is placed in all patients planned for breast-conserving surgery (BCS) receiving neoadjuvant chemotherapy (NACT) to localise the tumour bed in case response to chemotherapy makes later localisation impossible. A tumour that was localised with a radio-opaque clip before NACT will then need a second localisation procedure, after the completion of NACT to aid BCS. The two most commonly used methods are hookwire and radio-guided occult lesion localisation. Magseed®, a newly available technology consisting of a small magnetic seed, has now become available. The seed is placed instead of a radio-opaque clip before the start of or during NACT and can remain in place until the time of BCS.
METHODS: A retrospective cohort study was performed, collecting data on patients who had a Magseed placed before or during NACT from December 2018 to February 2020.
RESULTS: Twenty-one Magseed devices were placed into the breasts of 20 patients, 18 under ultrasound guidance, and three under stereotactic guidance. The average breast volume of individuals who had seeds placed was 1 532 g ± 869 g. The duration that the seeds were in situ was 138 days ± 45 days. All preoperatively placed seeds were retrieved at the surgery with no observed migration outside the tumour bed.
CONCLUSION: Magseed placement before NACT is a safe and technically simple technique that can be done under ultrasound guidance in the majority of cases. It has the advantage of being a single procedure with an associated reduction in time off work and travel cost to the patient, as well as flexibility in terms of the time of placement.
Keywords: Magseed, neoadjuvant chemotherapy, breast-conserving surgery, wide local excision
Introduction
Adjuvant or postoperative systemic therapy has been the main form of treatment for early-stage breast cancer for many years and neoadjuvant chemotherapy (NACT), referring to the use of systemic therapy before surgery, was reserved for the treatment of inoperable, locally advanced disease.1 However, recently published guidelines document a shift in practice to using NACT in patients with early breast cancer. Multidisciplinary teams are now using tumour biology rather than stage to guide treatment, with the result that patients with smaller tumours now receive NACT.2 Among the benefits of NACT is an increase in the feasibility of breast-conserving surgery (BCS) among women with early breast cancer who would otherwise require mastectomy due to unfavourable breast-to-tumour ratio, and an increase in the cosmesis of breast-conserving surgery among BCS candidates who might otherwise achieve inferior cosmetic results due to unfavourable breast-to-tumour ratio. With the development of new chemotherapeutic agents, dramatic response rates can be achieved in patients receiving NACT.3 Therefore, clip placement at the time of diagnosis or during treatment once a response to NACT has been established represents the standard of care to locate the original tumour bed during BCS.4 This is done in order to facilitate localisation and excision of the tumour after NACT. Prior to the BCS procedure, a second localisation procedure is then necessary in the event of a significant response to NACT. Hookwire, radio-guided occult lesion localisation (ROLL) or Iodine (125I) radioactive seed localisation are the most commonly used methods.5-7 All these methods have significant disadvantages. In the case of hookwire localisation, the disadvantages include possible displacement of the wire, challenges estimating the distance from the entry point of the wire through the skin to the tip of the wire and the risk of diathermy burns conducted to the skin via the wire. ROLL involves the injection of a radioisotope into the breast. The main drawback is the inability to confirm the correct site of the injection because the radioisotope is not radiopaque. The use of an Iodine (125I) radioactive seed negates this problem because the seed is radiopaque. The use of both ROLL and Iodine (125I) radioactive seed localisation is hampered by the radiation safety precautions required to set up and support a service that requires nuclear isotopes. The three traditional methods have the additional logistical drawback of scheduling close to the time of surgery which can have a significant impact on list scheduling for the surgeon. These disadvantages have prompted the search for a new method of localisation. A small magnetic seed (Magseed®) that can accurately localise impalpable breast lesions without many of the above-mentioned problems has become available.8,9
The study aims to assess the use of Magseed localisation of breast lesions in patients undergoing BCS after NACT. The objectives include assessment of the ease of placement of seeds, measurement of duration of seed placement, seed migration, ease of Magseed detection during surgery, interference of seeds with sentinel node biopsy and assessment of tissue reaction.
Methods
Patients
A retrospective cohort study, which included all patients meeting the inclusion criteria managed by the Groote Schuur Hospital/University of Cape Town Breast Surgery unit from December 2018 to February 2020, was undertaken. The inclusion criteria were female patients, age 18 or older, with a core biopsy-proven invasive breast cancer who had a Magseed placed before or during NACT and underwent subsequent BCS.
Ethical approval for the study was received from the Human Research Ethics Committee at the University of Cape Town. Several variables were collected, including the size of the tumour before and after chemotherapy, type of breast cancer, duration the seed was in situ, method of seed placement, depth of seed from the skin, size of the breast, the weight of the specimen, tissue reaction to the seed, presence of seed migration and postoperative complications. All patients were anonymised before statistical analysis.
Procedure
According to local management policy, a Magseed (Endomagnetics, Cambridge, UK) was placed into the centre of the breast tumour by a radiologist. The procedure is very similar to the placement of an intralesional clip, with which most radiologists are familiar. The seed is introduced via a 12- or 20 cm 18-gauge deployment needle under local anaesthetic with ultrasound or stereotactic guidance. A single view mammogram was performed immediately after the procedure, if the placement was done with stereotactic guidance, to document the seed position. If the seed was placed with ultrasound guidance and the radiologist was satisfied with the position as seen on ultrasound, no additional imaging was performed. Repeat two-view mammography was performed on the preoperative day to confirm the accurate positioning of the seed and to note any migration. The position of the seed was compared to the tumour position on the pre-NACT images. Measurements of the tumour were made on mammography and ultrasound at diagnosis and the largest measurement in millimetres was recorded as the preoperative measurement of tumour size.
BCS was performed under general anaesthesia on all patients and was defined as a procedure with a partial gland removal. Procedures were divided into level I oncoplasty where less than 20% of breast tissue was removed with no skin excision and level II oncoplasty where major volume resection of more than 20% including skin excision based on breast reduction techniques was performed.10
The Sentimag probe, which detects the magnetic signature and uses a tone and count change in relation to the distance of the end of the probe was used the day before surgery to mark the position of the seed on the skin. The skin incision used for BCS was designed taking the marked skin position of the Magseed into account. Intraoperatively the skin was mobilised in the oncoplastic plane and the point of the maximum count was re-marked on the breast parenchyma to aid excision of the tumour. High counts in the specimen and the absence of residual counts in the breast confirmed tumour excision. Specimen X-ray was performed at the discretion of the operating surgeon to confirm seed removal and evaluate the proximity of the tumour or malignant calcifications to the surgical margins.
Patients without clinical or radiological evidence of lymph node involvement underwent sentinel lymph node biopsy (SLNB). Patients with axillary involvement underwent axillary lymph node dissection (ALND).
Data from surgical specimens were included in the study. Tumour maximum diameters were reported in millimetres. Tumour grading was reported according to the Nottingham Histologic Score system (the Elston-Ellis modification of Scarff-Bloom-Richardson grading system). Oestrogen receptor (ER), progesterone receptor (PR), HER2 and Ki67 were studied through immunohistochemistry (IHC). ER and PR were recorded according to the Allred score between 0 and 8 and the Ki67 index was expressed as a percentage of positive cells. Trastuzumab is not available at our hospital, and therefore, routine fluorescent in situ hybridisation (FISH) was not performed. Equivocal HER2 results by IHC were interpreted as HER2 negative.
The standard chemotherapy regime used was sequential anthracycline-cyclophosphamide and taxane (AC-T). Four doses of AC were followed by four doses of taxane at 3-weekly intervals.
The descriptive statistics were evaluated using the Statistical Package for the Social Sciences (SPSS) 21.0 (IBM Corp, Inc, New York, USA) package programme. The complementary statistical methods (mean, standard deviation) were measured in the evaluation of the study data. Numerical variables were assessed for normality using the Shapiro-Wilk test and subsequently analysed by appropriate parametric and nonparametric tests. A two-tail test hypothesis was used with 0.05 as a discriminator for rejection of the null hypothesis.
Results
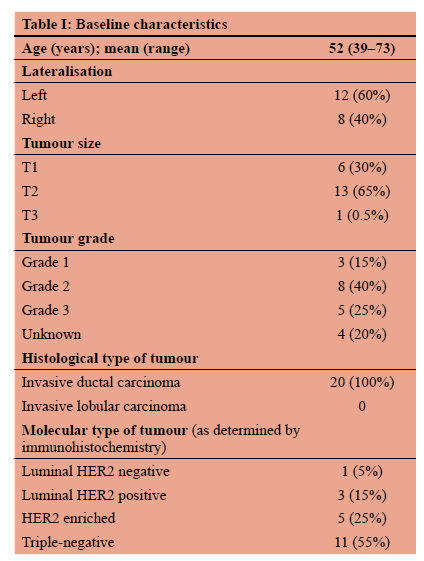
Twenty patient folders were reviewed. Their baseline characteristics are represented in Table I. Twenty-one Magseed devices were placed into the breasts of 20 patients, 18 under ultrasound guidance, and three under stereotactic guidance. The reason for the stereotactic placement was the targeting of extensive calcifications extending beyond the primary tumour in one patient (this patient had two seeds placed to bracket the lesion), and late placement of a seed after six cycles of chemotherapy in the second patient as the tumour was no longer visible on ultrasound due to the chemotherapy effect. Estimated breast size was calculated using mammogram measurements using the breast volume by elliptical cone estimation as described by Fung et al.11 The average breast volume was 1 532 g ± 869 g. The average distance of the seed from the skin as measured on ultrasound was 11 mm ± 6.5 mm. There was no reported difficulty in seed placement from radiology reports. The duration that the seeds were in situ was 138 days ± 45 days (Figure 1).
Surgery
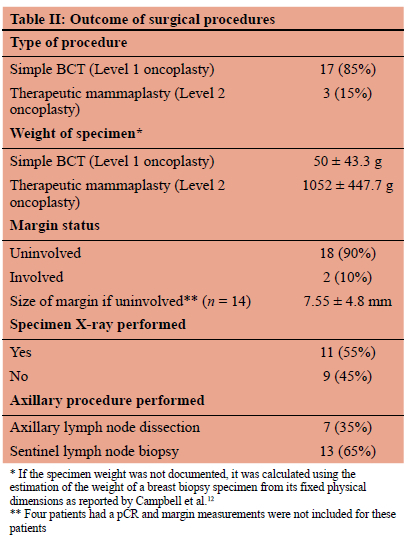
The outcomes of the surgical procedures performed are summarised in Table II. All the seeds placed were retrieved as confirmed by either high on table magnetometer counts or by specimen X-ray. There was no reported interference between the superparamagnetic iron (SPIO) tracer Magtrace® documented in the operative notes. Two patients had involved deep margins which could not be improved with surgery. They had whole breast radiation with a tumour bed boost.
Response to chemotherapy
The mean size of the tumour decreased significantly (9.6 mm) comparing the size of the tumour before chemotherapy (25.7 mm ± 10.5 mm) and after chemotherapy (16.1 mm ± 12.5 mm) (Welch's t-test, p < 0.012). The tumours of eight patients were not palpable at the end of chemotherapy and three patients had only slight thickening left. The remaining nine patients still had palpable tumours at the end of chemotherapy with tumours more than 20 mm in size.
Pathologic reaction to seed
On pathology specimens, the only finding other than expected post NACT tumour response and fibrosis was hemosiderin-laden macrophages in proximity to the seed (Figure 2).

Complications
There was one minor complication reported in a patient who developed a postoperative surgical site infection that resolved on antibiotics.
Discussion
Magseed consists of a small, non-radioactive, paramagnetic steel and iron oxide seed. The seed is visible on both ultrasound and mammogram after placement and a mam-mogram can be used to confirm correct placement. The main advantage of Magseed is that the patient is subjected to a single procedure, there is no need for a repeat localisation before surgery and the seed is not regulated by radioisotope legislation.13
There are currently no published studies where Magseed was placed before NACT in breast cancer patients. The published studies reporting on Magseed use in the NACT setting use Magseed to localise previously clipped nodes to facilitate targeted axillary dissection.1415 To our knowledge, this is the first study documenting the use of Magseed in patients undergoing NACT where Magseeds have been placed before or during NACT for the localisation of breast lesions in BCS. Worldwide the use of NACT for breast cancer is increasing.16 Most of the cases (95%) in this study were either triple-negative (55%) or HER2 positive (40%). A significant response to chemotherapy could be expected in patients receiving NACT with a 50% pathological complete response (pCR) rate in triple-negative and 60% pCR rate in HER2 positive patients treated with dual HER2 blockade.1718 These high response rates to NACT have increased eligibility for BCS with a significant number of tumours becoming impalpable after chemotherapy.19 Studies have reported ease of placement of Magseeds.920 22 None of our radiologists reported any difficulty in placing the seeds. In our patient population, even in patients with large breast sizes averaging 1 532 ± 869 g, the seeds were easy to place into the centre of the tumour with ultrasound guidance, using a technique familiar to our radiologists, in the majority of cases.
The majority of our patients (65%) had tumours larger than 2 cm with an average overall size of 25.7 ± 10.5 mm. The large tumour sizes can be explained by the fact that all the study patients presented with symptomatic breast lumps as South Africa does not have a national population-based mammographic screening programme. The ease of placement could be explained by the large size of the tumours observed in our study with larger size tumours aiding seed placement using ultrasound guidance.
Magseed has regulatory approval in Europe (CE mark) and the USA (FDA) for medical device safety, with long-term use approved by the FDA and CE mark.92324 In our patients, seeds remained in place for an average of 138 ± 45 days before removal, with seeds being placed before the start of chemotherapy or early on during chemotherapy. We have found no decrease in the signal strength at the time of removal of the seeds. Even in the patient with a Magseed in situ for 201 days we had no difficulty in localising the Magseed due to low signal strength.
Harvey et al.9 found no migration in the twenty-nine magnetic seeds that were placed in 28 patients who underwent a total mastectomy. In our study, removal was confirmed either by specimen X-ray or high magnetometer counts in the specimen. The absence of device migration was confirmed by radiologists (preoperative mammography), surgeons (Sentimag probe), and pathologists (specimen analysis). We found no migration of the seeds and all seeds were removed during surgery. The absence of migration was confirmed by the fact that residual tumour or tumour bed was found in all pathology specimens, confirming that the Magseed remained in place close to the original placement site.
A combined technique using a Magseed to localise an impalpable breast tumour and an SPIO tracer to localise sentinel nodes has been described by Hersi et al.25 They found the combined magnetic technique provided accuracy in tumour localisation and SLN detection. Sixty-five per cent of our patients had a combined sentinel node biopsy using an SPIO tracer and Magseed. Our technique involves injecting the SPIO tracer (Magtrace) directly opposite the quadrant where the Magseed is situated. For example, if the seed is situated in the breast at the 2 o'clock position, the SPIO tracer is injected peri-areolar at 7 o'clock. We have found no interference between the SPIO tracer and the Magseed if the SPIO tracer is injected as described. With a lesion directly behind the nipple-areola complex, an alternative sentinel node or lesion localisation technique needs to be considered to avoid interference.
Magseed is known to produce minimal tissue reaction.9 Little is known about the interaction of chemotherapy with the seed if placed before chemotherapy, and currently Magseed is not licensed for use before chemotherapy in both the USA and Europe outside of clinical trials. On histology in this study, we found evidence of haemosiderin-laden macrophages around the seed but all the other histological findings were consistent with post NACT tumour regression. The haemosiderin-laden macrophages resemble what is seen in breast and axillary node histology specimens after injection of the breast with an SPIO tracer.
There are disadvantages to the use of Magseed. The cost of both the seed and the localisation equipment is significantly more compared to wire localisation.9 In our study 9/20 (45%) of the patients had palpable tumours at the end of NACT and one can argue that the seed placement was not necessary to facilitate BCS. A significant cost saving is possible if the seeds are placed only once it is confirmed that the tumour is chemo sensitive. In future, we will only place seeds before the start of chemotherapy if the tumour is impalpable at presentation. Patients with palpable tumours will be assessed at cycle 2, with a Magseed placed once a response to chemotherapy is confirmed. The seed interferes with MRI limiting diagnostic accuracy, as it leaves a significant 4-6 cm signal void artefact, due to the iron content in the seed.23 Breast MRI is not used to assess response to NACT in our unit - we only use clinical and mammographic evaluation after NACT - and therefore was not found to be a negative factor, but this might prove to be a problem in units where routine MRI is used to assess chemotherapy response. Although the seed can be detected at a depth of up to 4 cm, it is less reliable at greater depths. Also, when the magnetometer is in use, metal objects need to be removed from the surgical field.26
There are some limitations to this study, most notably the retrospective nature of the data collection. There was no standardised reporting from the radiologists, surgeons, or pathologists involved in treating the participants, but most of the procedures (> 90%) were performed by a single radiologist and surgeon. Also, results could have been influenced by the small sample size, which needs to be kept in mind when interpreting the results.
Conclusion
To our knowledge, no previous study has been published in which Magseed was placed before chemotherapy to aid tumour removal during BCS. Magseed appears to be safe and effective and can be placed before or during chemotherapy for the localisation and facilitation of BCS in patients undergoing NACT. Magseed placement is a technically simple technique that can be done under ultrasound guidance in the majority of cases. Seed migration did not occur and there was no interference with sentinel node detection at the time of surgery if a combined procedure was done. Magseed localisation before chemotherapy involves a single procedure with advantages for both the patient and health care provider. Larger studies are needed to confirm these findings as well as to provide more information regarding the optimal timing of seed placement.
Conflict of interest
The authors declare that they have no competing known financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding source
The first author received funding, limited to travel support, from Sysmex South Africa, the local distributor of Magseed. Sysmex had no role in the study concept and design, data acquisition, analysis and interpretation, manuscript preparation, or decision to submit for publication.
Ethical approval
Ethical approval for the study was received from the Human Research Ethics Committee at the University of Cape Town [HREC: 200/2019].
ORCID
F Malherbe https://orcid.org/0000-0001-8910-6925
L Roodt https://orcid.org/0000-0002-0545-5413
F Noor https://orcid.org/0000-0003-3985-3660
R Gamieldien https://orcid.org/0000-0002-6814-8699
D Chetty https://orcid.org/0000-0002-5033-2180
D Anderson https://orcid.org/0000-0001-7594-213X
Τ Thebe https://orcid.org/0000-0002-8488-7424
L Cairncross https://orcid.org/0000-0001-5368-9882
REFERENCES
1. Rubens RD, Sexton S, Tong D, et al. Combined chemotherapy and radiotherapy for locally advanced breast cancer. Eur J Cancer. 1980;16(3):351-6. https://doi.org/10.1016/0014-2964(80)90352-7. [ Links ]
2. Korde LA, Somerfield MR, Carey LA, et al. Neoadjuvant chemotherapy, endocrinetherapy, and targetedtherapy for breast cancer: ASCO guideline. J Clin Oncol. 2021;39(13):1485-505. https://doi.org/10.1200/JCO.20.03399. [ Links ]
3. Asaoka M, Gandhi S, Ishikawa T, Takabe K. Neoadjuvant chemotherapy for breast cancer: past, present, and future. Breast Cancer (Auckl). 2020;14:1178223420980377. https://doi.org/10.1177/1178223420980377. [ Links ]
4. Kuehn T. Breast surgery after primary systemic treatment. In: Wyld L, Markopoulos C, Leidenius M, Senkus-Konefka E, editors. Breast Cancer Management for Surgeons: Springer, Cham; 2018. p. 255-61. https://doi.org/10.1007/978-3-319-56673-3_21. [ Links ]
5. Dua SM, Gray RJ, Keshtgar M. Strategies for localisation of impalpable breast lesions. Breast J. 2011;20(3):246-53. https://doi.org/10.1016/j.breast.2011.01.007. [ Links ]
6. Green M, Vidya R. Techniques used to localize occult breast lesions: an update. Clin Breast Cancer. 2018;18(3):e281-e3. https://doi.org/10.1016/jxlbc.2018.01.001. [ Links ]
7. Gunn J, McLaughlin S. Current trends in localisation techniques for non-palpable breast lesions: making the invisible visible. Curr Breast Cancer Rep. 2017;9(2):165-71. https://doi.org/10.1007/s12609-017-0244-9. [ Links ]
8. Price ER, Khoury AL, Esserman LJ, Joe BN, Alvarado MD. Initial clinical experience with an inducible magnetic seed system for preoperative breast lesion localisation. AJR Am J Roentgenol. 2018;210(4):913-7. https://doi.org/10.2214/AJR.17.18345. [ Links ]
9. Harvey JR, Lim Y, Murphy J, et al. Safety and feasibility of breast lesion localisation using magnetic seeds (Magseed): a multi-centre, open-label cohort study. Breast cancer Res Treat. 2018;169(3):531-6. https://doi.org/10.1007/s10549-018-4709-y. [ Links ]
10. Clough KB, Kaufman GJ, Nos C, Buccimazza I, Sarfati IM. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol. 2010;17(5):1375-91. https://doi.org/10.1245/s10434-009-0792-y. [ Links ]
11. Fung JT, Chan SW, Chiu AN, Cheung PS, Lam S. Mammographic determination of breast volume by elliptical cone estimation. World J Surg. 2010;34(7):1442-5. https://doi.org/10.1245/s10434-009-0792-y. [ Links ]
12. Campbell L, Teasdale C, Watkins RJTB. Estimation of the weight of a breast biopsy specimen from its fixed physical dimensions. The Breast. 1998;7(4):229-30. https://doi.org/10.1016/S0960-9776(98)90115-1. [ Links ]
13. Chacko SM, Marshall HN. Implementation of Preoperative magnetic seed localisation for breast and axillary lesions: an alternative to wires and radioactive seeds. J Radiol Nurs. 2018;37(3):154-7. https://doi.org/10.1016/j.jradnu.2018.03.015. [ Links ]
14. Reitsamer R, Peintinger F, Forsthuber E, Sir A. The applicability of Magseed® for targeted axillary dissection in breast cancer patients treated with neoadjuvant chemotherapy. Breast. 2021;57:113-7. https://doi.org/10.1016/j.breast.2021.03.008. [ Links ]
15. Greenwood HI, Wong JM, Mukhtar RA, Alvarado MD, Price ER. Feasibility of magnetic seeds for preoperative localisation of axillary lymph nodes in breast cancer treatment. AJR Am J Roentgenol. 2019;213(4):953-7. https://doi.org/10.2214/AJR.19.21378. [ Links ]
16. Murphy BL, Day CN, Hoskin TL, Habermann EB, Boughey JC. Neoadjuvant chemotherapy use in breast cancer is greatest in excellent responders: triple-negative and HER2+ subtypes. Ann Surg Oncol. 2018;25(8):2241-8. https://doi.org/10.1245/s10434-018-6531-5. [ Links ]
17. Buzdar AU, Valero V, Ibrahim NK, et al. Neoadjuvant therapy with paclitaxel followed by 5-fluorouracil, epirubicin, and cyclophosphamide chemotherapy and concurrent trastuzumab in human epidermal growth factor receptor 2-positive operable breast cancer: an update of the initial randomised study population and data of additional patients treated with the same regimen. Clin Cancer Res. 2007;13(1):228-33. https://doi.org/10.1158/1078-0432.CCR-06-1345. [ Links ]
18. Von Minckwitz G, Untch M, Blohmer J-U, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30(15):1796-804. https://doi.org/10.1200/JCO.2011.38.8595. [ Links ]
19. Spronk PE, Volders JH, Van den Tol P, Smorenburg CH, Peeters M-JTV. Breast conserving therapy after neoadjuvant chemotherapy; data from the Dutch Breast Cancer Audit. Eur J Surg Oncol. 2019;45(2):110-7. https://doi.org/10.1016/j.ejso.2018.09.027. [ Links ]
20. Conversano A, Balleyguier C, De Fremicourt M, et al. Magnetic seed localisation for non-palpable lesions in patients undergoing breast conservative surgery. Eur J Gynaecol Oncol. 2020;41(1):48-53. https://doi.org/10.31083/j.ejgo.2020.01.4985. [ Links ]
21. Micha A, Sinnett V, Wilson R, et al. Interim analysis of an evaluation of clinical outcome and patient and clinician satisfaction with magnetic seeds compared with guide wires for localisation of impalpable breast lesions for surgery. Eur J Surg Oncol. 2019;45(5):884. https://doi.org/10.1016/j.ejso.2019.01.216. [ Links ]
22. Tayeh S, Gera R, Perry N, et al. The use of magnetic seeds and radiofrequency identifier tags in breast surgery for nonpalpable lesions. Anticancer Res. 2020;40(1):315-21. https://doi.org/10.21873/anticanres.13955. [ Links ]
23. Hayes MK. Update on preoperative breast localisation. Radiol Clin North Am. 2017;55(3):591-603. [ Links ]
24. Jeffries DO, Dossett LA, Jorns JM. Localisation for breast surgery: the next generation. Arch Pathol Lab Med. 2017;141(10):1324-9. https://doi.org/10.5858/arpa.2017-0214-RA. [ Links ]
25. Hersi A-F, Eriksson S, Ramos J, et al. A combined, totally magnetic technique with a magnetic marker for non-palpable tumour localization and superparamagnetic iron oxide nanoparticles for sentinel lymph node detection in breast cancer surgery. Eur J Surg Oncol. 2019;45(4):544-9. https://doi.org/10.1016/j.ejso.2018.10.064. [ Links ]
26. Cheang E, Ha R, Thornton CM, Mango VL. Innovations in image-guided preoperative breast lesion localisation. Br J Radiol. 2018;91(1085):20170740. https://doi.org/10.1259/bjr.20170740. [ Links ]
 Correspondence:
Correspondence:
email: francois.malherbe@uct.ac.za














