Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.2 Cape Town Jun. 2022
http://dx.doi.org/10.17159/2078-5151/SAJS3745
TRAUMA
Never to be missed again - an analysis of 55 consecutive cases of traumatic diaphragmatic hernia
VF Kruger; TRA Calderan; RB de Carvalho; ES Hirano; GP Fraga
Division of Trauma Surgery, Department of Surgery, University of Campinas, Brazil
ABSTRACT
BACKGROUND: This report reviews our clinical experience with 55 cases of traumatic diaphragmatic hernia at a Brazilian university hospital. Traumatic diaphragmatic hernia is an uncommon injury and presents diagnostic and therapeutic challenges. Occasionally, it is missed in trauma patients and is usually associated with significant morbidity and mortality. This analysis aimed to improve the diagnostic outcomes of trauma patient care.
METHODS: Retrospective design analysis of database records of trauma patients at HC-Unicamp were performed to investigate incidence, trauma mechanism, diagnosis, herniated organs, associated injuries, trauma score, morbidity and mortality.
RESULTS: Fifty-five patients were analysed. Blunt trauma was two-fold more frequent than penetrating trauma and was associated with high-grade injury; motor vehicle collision was the most common mechanism. Left-sided hernia was four-fold more frequent than that on the right side, although critical injuries were more frequently associated with the right side. The stomach was the most herniated organ in both trauma mechanisms. Preoperative diagnosis was mostly performed using chest radiography (55%). Postoperative diagnosis was mostly performed via laparotomy rather than laparoscopy. Associated injuries were observed in 43 patients (78%) and the mortality rate was 20% for both the sides
CONCLUSION: Isolated injuries are rare, and the presence of associated injuries increases morbidity and mortality. Chest radiography in the trauma bay is useful as an initial examination, although it is not suitable for use as a definitive method. Despite the use of laparoscopy in a few cases, laparotomy is the most common approach.
Keywords: traumatic diaphragmatic hernia, diaphragm, hernia, diaphragmatic injury.
Introduction
Traumatic diaphragmatic hernia (TDH) is defined as the protrusion of the abdominal structures through an injured diaphragm into the thoracic cavity. The relative incidence of blunt and penetrating diaphragmatic injury (DI) reflects differences in geographic regions and socioeconomic characteristics of these regions. Blunt trauma (BT) is often common in developed regions; however, less developed regions have higher rates of penetrating injuries.1
A recent review of 3 783 patients with DI suggested that 67% were diagnosed with penetrating trauma (PT) and 33% with BT.2 PTs are commonly associated with gunshot wounds (GSW) (66%), while BTs are commonly associated with motor vehicle collisions (MVC) (63%).
TDH is more frequently caused by BT (as high as 75% of the time) because it involves more severe kinematics;3 however, its real incidence may be slightly higher than expected because of underdiagnosis. Therefore, it is important to recognise that TDH may arise secondary to diaphragmatic injuries.
The clinical diagnosis of TDH is challenging for trauma surgeons who depend on a high index of suspicion, mechanism of trauma, and interpretation of radiological images. As the diagnosis is contingent on the physician's awareness of these factors, when these go unnoticed in trauma patients, TDH remains unidentified leading to significant mortality and morbidity.
It is essential, therefore, to avoid missed injuries and prevent delays in the diagnosis.
The increase in the number of trauma patients is a challenge for global public health authorities. The aim of this study was to perform a retrospective analysis of the records of our clinical experience, investigate the demographics of incidence, trauma mechanisms, diagnosis, morbidity, and mortality of TDH, and evaluate better outcomes.
Methods
A descriptive retrospective analysis of the medical records of patients from the trauma database of the Division of Trauma Surgery (DCT) at University of Campinas between January 1990 and December 2017 was performed. Since 1987, the DCT has been a team of specialists in trauma and acute care surgery actively working on training residents and promoting trauma prevention programmes. The metropolitan area of Campinas has a population of 3.8 million, encompassing 20 cities. The HC-Unicamp is a referral hospital for the population using the public health system in this region. It is a level 1 trauma centre with approximately 500 beds, specific trauma floor with 16 beds dedicated to low complexity injuries, and a trauma-ICU with 10 beds for patients with high complexity injuries.
The medical records of 3 003 patients who underwent surgery for penetrating or blunt abdominal trauma were reviewed. Patients diagnoses with PT were also screened for diaphragmatic injuries and included in this study. The records of patients with TDH were analysed for demographic data, blunt and penetrating mechanism, haemodynamic status at admission, grade and side of the injury, herniated organs, diagnostic methods, the interval between diagnosis and surgery, length of stay in the trauma floor and ICU, trauma scores, associated injuries, morbidity, and mortality. Trauma scores were calculated using the revised trauma score (RTS), injury severity score (ISS), and trauma injury severity score (TRISS).
Diaphragm injury was graded according to the American Association for the Surgery of Trauma (AAST) injury scale4 as follows: grade I, diaphragm contusion; grade II, laceration less than or equal to 2 cm; grade III, laceration greater than 2 cm and less than 10 cm; grade IV, laceration greater than 10 cm, with tissue loss less than or equal to 25 cm2; and grade V, laceration with tissue loss greater than 25 cm2. Patients with grade I injuries, congenital defects, hiatal hernias, chronic and delayed traumatic hernias for more than 14 days were excluded. Since 2008, with the availability of multi-slice CT scans in HC-Unicamp, trauma patients with a high-energy trauma mechanism, haemodynamic stability, and without the criteria for immediate surgery have been submitted to contrast-enhanced CT scan.
Our institutional protocol for the treatment of TDH entails surgical exploration, which uses laparotomy, laparoscopy or thoracolaparotomy to elucidate associated injuries and haemodynamic status, according to the trauma mechanism involved. After recognising TDH, the injury is treated by repairing defects with an interrupted nonabsorbable suture, such as polypropylene or using a mesh for large ruptures. Further, an ipsilateral chest tube or a nasogastric tube may be placed at the site of the injury for drainage.
Statistical analysis of the research was conducted using RStudio software. Fisher's test was used to compare the data, and statistical significance was set at p < 0.05.
Results
Of the 3 003 reviewed patients, TDH was diagnosed in 55 patients (1.8%). All further analyses were performed in 55 patients. TDH was predominant in young men and was observed in 46 of these 55 patients (83%).
Furthermore, BT was observed in 40 of 55 analysed cases (72.7%). MVC was the most common blunt mechanism (65%), followed by pedestrian vehicle accidents (PVA) (27.5%), assault (5%), and falls (2.5%). Among penetrating trauma, stab wounds (SW) were present in nine (60% of PT) and GSW in six (40%).
Preoperative diagnosis was made in 37 cases (67%), based on chest radiography (CXR) in 30 (55%), and multi-slice CT scan in seven (13%). Common abnormal findings on CXR include elevation of the diaphragm (27 cases, 90%), intrathoracic abdominal structure (18 cases, 60%), pulmonary contusion with rib fractures (15 cases each, 50%), blurring of the diaphragm contour and subcutaneous emphysema (13 cases, 43%), and hemopneumothorax (eight cases, 26%). Common signs of CT scan were herniation of abdominal contents in the chest (seven cases, 100%), collar sign, and dependent viscera sign was found in three cases (43%) and thickening of the diaphragm in one case (14%) (Figure 1).
The remaining patients were diagnosed intraoperatively (33%). Among these, 15 cases (27%) were diagnosed by laparotomy, presenting haemodynamically unstable and associated intra-abdominal injury, and three (5%) by diagnostic laparoscopy, with SW in the left thoracoabdominal injury (Figure 2).

Surgical procedures were performed within 48 hours in 45 cases (82%), of which 33 were BT and 12 were PT. Surgeries were performed after 48 hours but within 28 days in 10 cases (18%), of these, seven in BT and three PT. Our cohort only included patients whose surgeries were performed within the above-mentioned time period (acute phase) to avoid the effects of chronic phase TDH, which is effective if the delay in surgery is more than 28 days.
Laparotomy was the most performed procedure (49 cases, 89%), followed by thoracolaparotomy (five cases, 9%) and laparoscopy (three cases, 5.4%).
Left-sided hernia was the most common (44 cases, 80%), followed by the right side (10 cases, 18%), and bilateral hernia (one case, 2%).
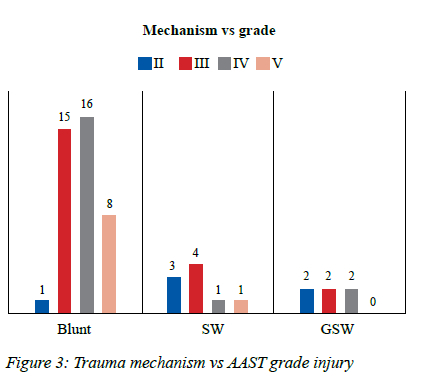
Diaphragmatic grade III injury occurred in 21 patients (38%), grade IV in 19 (34%), grade V in nine (17%) and grade II in six (11%) In SW, grade III injury was the most common, followed by grade II. In GSW, grades II, III, and IV had proportionally equal cases. In BT, grade IV was the most common, followed by grade III BT (Figure 3).
The stomach was the most herniated organ in both trauma mechanisms (39 cases), followed by the spleen (18 cases), colon (17 cases), small bowel (six cases), and liver (six cases). Twenty-five (45.5%) patients had more than one herniated abdominal structure.
A total of 43 patients (78%) presented with associated injuries.
Associated intra-abdominal injuries were observed in 37 patients (67%). The spleen was the most injured in 19 cases (35%), followed by the liver in 16 cases, (29%) and stomach in eight cases (15%). Spleen injury grade I-II (low grade) was observed in six cases (32%) and grade III-IV-V (high grade) in 13 cases (68%). Liver injury grades I-II-III (low grade) were observed in 10 cases (63%), and grade IV-V (high grade) in six cases (37%). In BT, grade I stomach injury was observed in two cases, with only one case showing perforation. In PT, all five injuries were grade II and III. Extra-abdominal injuries were found in 28 cases (51%), where pelvic fractures (12 cases, 22%), long bone fractures (nine cases, 16%), and hemopneumothorax (eight cases, 15%) were the most common injuries. Only one case (2.5%) of traumatic aortic injury was diagnosed. An ISS greater than 25 was found in 21 cases (38.2%) and was observed to be frequently associated with BT (p = 0.0049) using Fisher's test. There were six cases (11%) with TRISS less than 0.5, and 49 cases (89%) having TRISS greater than 0.5. The admission RTS average for BT was 6.4 and that for PT was 7.4.
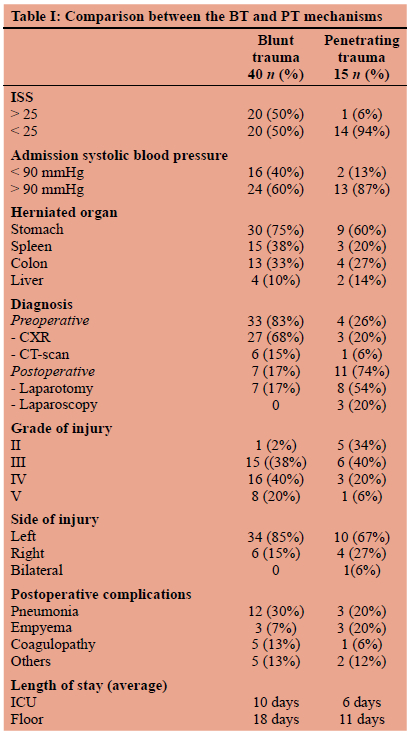
A comparison between the BT and PT mechanisms is shown in Table I.
Postoperative complications occurred in 32 patients (58.2%). Pneumonia was the most frequent complication (15 cases, 47%) in both trauma mechanisms, followed by empyema and acute coagulopathy associated with trauma (six cases each, 19%).
Excluding deaths in less than 24 hours, the length of hospital stay ranged from a minimum of 3 to a maximum of 61 days. The average hospital stay in trauma floor for penetrating wounds was 11 days, whereas that for BT was 18 days, the trauma-ICU average length of stay was 5 days for PT and 11 for BT.
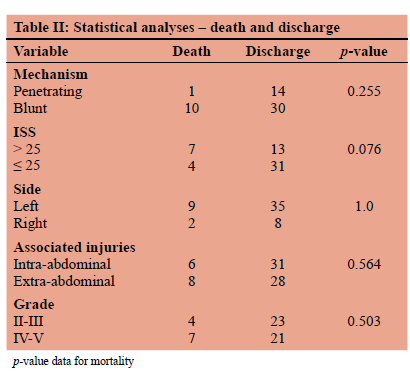
The overall mortality rate was 20% (n = 11). Mortality was similar for left- and right-sided TDH. The statistical analyses are shown in Table II.
Discussion
It is important to distinguish between isolated injury and the occurrence of diaphragmatic hernia that may arise secondary to this injury. It is also essential to highlight the differences between blunt and penetrating diaphragmatic disruptions. Penetrating wounds lead to small defects, with occult injury remaining in the silent period before symptoms. Pomerantz et al.5 reported that 85% of diagnosed cases are within the first three years after the trauma, and acute herniation after PT is uncommon. However, BT is the most common mechanism for the appearance of large linear ruptures with immediate herniation. De la Rocha et al.6 demonstrated that a sharp increase in intra-abdominal pressure can elevate the pressure gradient tenfold during a major abdominal trauma, transferring massive energy and leading to immediate herniation. As identified in our series, BT is associated with 73% of TDH, and 93% of TDH caused by BT is caused by road traffic injuries.
In hospital attendance, 75% of TDH cases occurred on the left as opposed to 25% on the right side; bilateral injuries are uncommon, occurring in only 2% of cases, corroborating the findings of our analysis.3,710 A comparison of injuries on both sides has been explained in some reviews. Lucido and Wall11 demonstrated the existence of muscle weakness at the embryonic fusion point in the posterolateral area of the left diaphragm. Further, the liver also has a protective effect on the right diaphragm during sudden elevations of intra-abdominal pressure.8 It is also notable that the rupture of the right diaphragm is often underdiagnosed in patients.8
Currently, the diagnosis of right-sided TDH in major trauma is possible owing to improvements in the trauma system. Efficient pre-hospital teams, which stabilise and transport the patient to a hospital, trauma surgeons, availability of blood banks 24/7 and the CT-scan technology used to obtain images interpreted by radiologists experienced in trauma centres all contribute to a more efficient diagnosis of right-sided TDH.
Aun et al.12 compared 97 cases of surgically treated TDHs, with 146 cases seen in 12 276 consecutive autopsies of patients who died because they did not receive medical care. Interestingly, the author in their data also observed a higher incidence of diaphragmatic lacerations on the ride side in the autopsy group than in the hospitalised group (50% vs 14%). Furthermore, the main cause of death in the autopsy group was haemorrhagic shock (80%), and it was concluded that trauma victims with right-sided TDH were more severely injured.
In our survey, 70% of right-sided TDH cases were diagnosed by immediate laparotomy due to haemodynamic instability because of major liver injuries.
Boulanger et al.8 reported that in TDH, 100% of the patients had associated lesions of abdominal organs on the right side, whereas 77% of patients carried these lesions on the left side. Our series corroborated these results, which showed that 90% of the injuries were on the right and 75% on the left side.
Meyers and McCabe13 reported the importance of TDH as a marker of serious injury in BT, and the outcome was entirely dependent on these injuries. Our results revealing a statistically significant (p = 0.0049) association between trauma mechanism and ISS greater than 25, demonstrating that in BT, TDH is a marker of serious injury.
Our survey demonstrated that the spleen and liver were the most frequently damaged solid organs, and gastrointestinal injuries were less common, seen more often only in PT. Pelvic fractures that were observed showed dynamics of injury, which were similar to those reported in the literature.2,8,14 As discussed by Rizoli et al.,15 traumatic aortic injury and TDH share similar dynamics of mechanical injury; however, only one patient (2.5%) experienced this complex injury in our cohort.
The stomach is the most herniated organ for the thorax, as its location is free in the upper level of the abdomen and hollow viscus with air contents facilitates herniation when the intra-abdominal pressure increases.13,14,16
Rodriguez-Morales et al.14 theorises that the diagnosis of TDH should be based on both the suspected trauma mechanism and careful physical examination.
Side collisions increase the risk of TDH threefold.17 Reiff et al.18 further suggested that the sensitivity of the diagnostic suspicion increases with the double mechanism of the collision, such as vehicular intrusion of more than 30 cm and speed of more than 40 km/h. In our survey, we were unable to locate the victim position or precise kinematics because of the retrospective analysis of medical records.
Aronoff et al.10 reported that confidence in the physical examination is disappointing, with the capacity to identify only 44% of diaphragmatic injuries after BT and 55% after PT.
The striking problem with TDH is that it is challenging for trauma surgeons to diagnose it. First, TDH remains a largely unfamiliar concept. Second, physical examination has a low specificity. Finally, TDH usually has associated injuries; haemodynamic shock or ventilatory impairment may arise due to other injuries caused by severe trauma and divert the attention of the attending physician from the diagnosis.
In our study, 15 patients (27%) were diagnosed with an immediate laparotomy. These patients presented haemo-dynamic instability despite resuscitation, due to the need for further investigations of associated injuries, such as penetrating wounds in the abdomen or thoracoabdominal region. In fact, the majority of patients had a preoperative diagnosis. Patients with suspected physical examination or trauma kinematics for TDH, without the criteria for immediate laparotomy, underwent confirmatory diagnostic methods, such as imaging and laparoscopy.
Gelman et al.19 showed that the sensitivity of the CXR in diaphragmatic injuries resulting from BT was 64% for the left side and only 17% for the right side.
In the present review, a diagnosis based on CXR was made in 55% of cases.
CXR was evaluated by the most experienced surgeon and radiologist, which increased the diagnostic sensitivity.
As our study is a retrospective analysis, we observed higher rates of CXR diagnoses compared to other methods such as computed tomography (CT). This could be attributed to CXR being the only facility available in our department for many years, its ease of use, and its low dependence on cooperation from the patient.
Despite being considered useful in the initial evaluation of suspected TDH, its low sensitivity is not suitable for use as a definitive method. We consider that, currently, with the availability of CT scans, its use is limited.
Several authors have described CT scan indicative signs for the diagnosis of BT and PT. The sensitivity of CT to diaphragmatic injuries for BT varies from 71% to 82%, and its specificity varies from 75% to 100%. In PT, it has a sensitivity of 86% and specificity of 79%.20 22 Coronal and sagittal multiplanar reformatting contributes to the accuracy of the diagnosis, allowing for better sensitivity and specificity of the examination.21 In our analysis, only 13% of diagnoses were made using CT, with a specificity of 100%. Currently, for a broad assessment of associated injuries, haemodynamically stable patients should undergo a CT scan as the gold standard.
Despite offering excellent images of the diaphragm, magnetic resonance imaging (MRI) is not suitable for acute trauma patients. As we have an evolved multidetector CT scan with 3D reconstruction, MRI is not used in our hospital.
Currently, extended FAST is considered propaedeutic in the diagnosis of cavity injuries, such as pneumothorax, haemothorax, and abdominal or pericardial free fluid; however, there is insufficient evidence of its use in the diagnosis of DI.
Ivatury et al.23 reported that the diagnostic accuracy of laparoscopy was excellent for hemoperitoneum and diaphragmatic lacerations, validating laparoscopy as an excellent tool to evaluate the diaphragm in PT. Thora-coscopy is an alternative option for the diagnosis and allows evacuation of retained haemothorax;24 however, it does not provide peritoneal cavity visualisation or excludes abdominal injury. Our series involved three cases in which diagnostic laparoscopy was used, and only one was diagnostic and therapeutic. This can be explained by inexperienced laparoscopic surgeons, as at the time of the study, most surgeons were experienced in open surgery.
Thus, it is important to highlight that expanding the spectrum of minimally invasive surgery can play an important role in the diagnosis and treatment of patients with DIs, and the evolution of devices that facilitate the execution of sutures does not require intracorporeal knots, hernia clips, extracorporeal knots, or synthetic mesh. However, a minimally invasive approach is highly dependent on the surgeon's expertise and patient stability to achieve better outcomes.
Early diagnosis and surgical repair are mandatory to avoid catastrophic sequelae. We hypothesised that the problem of missed TD injuries is due to three reasons. First, it is underdiagnosed using CXR. Second, it may also be missed due to the delayed rupture of devitalised tissue at the site of the initial injury, originally without herniation. However, this rupture is exacerbated by inflammatory and ischaemic processes, which weaken it and cause herniation. Finally, TDH may also be missed due to the delay in its detection, as it becomes evident only after extubation of a patient on mechanical ventilation, when their thoracic pressure becomes negative.13
Most of our patients underwent laparotomy; this approach is preferred because of high incidence of associated intra-abdominal injuries.
All survivors with BT had a significant length of stay in the trauma floor and intensive care unit, with a longer duration of mechanical ventilation, reflecting the severity and multiplicity of injuries. Mortality was significantly higher in patients with ISS > 25 and BT (10 cases, 90%) than in those with PT (one case, 10%); however, the difference was not statistically significant (p = 0.25). Our study reflects a global mortality rate of 20%. Interestingly, a comparison between the side and trauma mechanism of TDH had similar postoperative outcomes. Although rare, early mortality is mainly related to the associated injuries.
This study has limitations related to its retrospective design. Potential biases may occur because the analysis of established data shows a change in perspectives and tendencies in patient assessment. Data collection also relied on chart review at the participating institution and may contain errors or omissions.
Conclusion
TDH is uncommon; however, efforts should be made for early diagnosis as isolated injuries are rare, and the presence of associated injuries increases morbidity and mortality. CXR in the trauma bay is useful as an initial examination but is not suitable for use as a definitive method to diagnose TDH. CT scan, however, improved the ability to identify associated injuries with high specificity. Despite the use of laparoscopy, laparotomy is the most frequently used approach.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
The research protocol used in this study was approved without any restrictions by the Committee of Research Ethics and Institutional Review Board (IRB), School of Medical Sciences, Unicamp, under number 2.692.996 in May 2018.
ORCID
VF Kruger © https://orcid.org/0000-0001-6246-1898
TRA Calderan © https://orcid.org/0000-0003-4826-0453
RB de Carvalho © https://orcid.org/0000-0002-4171-0899
ES Hirano © https://orcid.org/0000-0001-5872-9353
GP Fraga © https://orcid.org/0000-0002-9524-1186
REFERENCES
1. Reber PU, Schmied B, Seiler CA, et al. Missed diaphragmatic injuries and their long-term sequelae. J Trauma. 1998;44(1):183-8. https://doi.org/10.1097/00005373-199801000-00026. [ Links ]
2. Fair KA, Gordon NT, Barbosa RR, et al. Traumatic diaphragmatic injury in the American College of Surgeons National Trauma Data Bank - a new examination of a rare diagnosis. Am J Surg. 2015;209(5):864-9. https://doi.org/10.1016/j.amjsurg.2014.12.023. [ Links ]
3. Shah R, Sabanathan S, Mearns AJ, Choudhury AK. Traumatic rupture of diaphragm. Ann Thorac Surg. 1995;60(5):1444-9. https://doi.org/10.1016/0003-4975(95)00629-Y. [ Links ]
4. Moore EE, Malangoni MA, Cogbill T, et al. Organ injury scaling. IV - thoracic vascular, lung, cardiac, and diaphragm. J Trauma. 1994;36(3):299-300. https://doi.org/10.1097/00005373-199403000-00002. [ Links ]
5. Pomerantz RM, Rodgers BM, Sabiston DC. Traumatic diaphragmatic hernia. Surgery. 1968;64(3):529-34. [ Links ]
6. De la Rocha AG, Creel RJ, Mulligan GN, Burns CM. Diaphragmatic rupture due to blunt abdominal trauma. Surg Gynecol Obstet. 1982;154(2):175-80. [ Links ]
7. Andrus CH, Morton JH. Rupture of the diaphragm after blunt trauma. Am Surg. 1970;119(6):686-93. https://doi.org/10.1016/0002-9610(70)90240-0. [ Links ]
8. Boulanger BR, Milzman DP, Rosati C, Rodrigues A. A comparison of right and left blunt diaphragmatic rupture. J Trauma. 1993;35(2):255-60. https://doi.org/10.1097/00005373-199308000-00014. [ Links ]
9. Ties JS, Peschman JR, Moreno A, et al. Evolution in the management of traumatic diaphragmatic injuries - a multicentre review. J Trauma. 2014;76(4):1024-8. https://doi.org/10.1097/TA.0000000000000140. [ Links ]
10. Aronoff RJ, Reynolds J, Thai ER. Evaluation of diaphragmatic injuries. Am J Surg. 1982;144(6):571-5. https://doi.org/10.1016/0002-9610(82)90548-7. [ Links ]
11. Lucido JL, Wall CA. Rupture of the diaphragm due to blunt trauma. Arch Surg. 1963;86:989-9. https://doi.org/10.1001/archsurg.1963.01310120107017. [ Links ]
12. Aun F, Lourenção JL, Younes RN, et al. Natural history and risk factors of traumatic diaphragmatic hernia. J Hosp Clin Fac Med. 1982;37(6):265-70. [ Links ]
13. Meyers BF, McCabe CJ. Traumatic diaphragmatic hernia. Occult marker of serious injury. Ann Surg. 1993;218(6):783-90. https://doi.org/10.1097/00000658-199312000-00013. [ Links ]
14. Rodriguez-Morales G, Rodriguez A, Shatney CH. Acute rupture of the diaphragm in blunt trauma: analysis of 60 patients. J Trauma. 1986;26(5):438-44. https://doi.org/10.1097/00005373-198605000-00005. [ Links ]
15. Rizoli SB, Brenneman FD, Boulanger BR, Maggisano R. Blunt diaphragmatic and thoracic aortic rupture - an emerging injury complex. Ann Thorac Surg. 1994;58(5):1404-8. https://doi.org/10.1016/0003-4975(94)91923-2. [ Links ]
16. Brown GL, Richardson JD. Traumatic diaphragmatic hernia -a continuing challenge. Ann Thorac Surg. 1985;39(2):170-3. https://doi.org/10.1016/S0003-4975(10)62559-3. [ Links ]
17. Kearney PA, Rouhana SW, Burney RE. Blunt rupture of the diaphragm - mechanism, diagnosis, and treatment. Ann Emerg Med. 1989;18(12):1326-30. https://doi.org/10.1016/S0196-0644(89)80270-7. [ Links ]
18. Reiff DA, McGwin Jr G, Metzger J, et al. Identifying injuries and motor vehicle collision characteristics that together are suggestive of diaphragmatic rupture. J Trauma. 2002;53(6):1139-45. https://doi.org/10.1097/00005373-200212000-00018. [ Links ]
19. Gelman R, Mirvis SE, Gens D. Diaphragmatic rupture due to blunt trauma - sensitivity of plain chest radiographs. AJR Am J Roentgenol 1991;156(1):51-7. https://doi.org/10.2214/ajr.156.1.1898570. [ Links ]
20. Killeen KL, Mirvis SE, Shanmuganathan K. Helical CT of diaphragmatic rupture caused by blunt trauma. AJR Am J Roentgenol. 1999;173(6):1611-6. https://doi.org/10.2214/ajr.173.6.10584809. [ Links ]
21. Larici AR, Gotway MB, Litt HI, et al. Helical CT with sagittal and coronal reconstructions - accuracy for detection of diaphragmatic injury. AJR Am J Roentgenol. 2002;179(2):451-7. https://doi.org/10.2214/ajr.179.2.1790451. [ Links ]
22. Bergin D, Ennis R, Keogh C, et al. The "dependent viscera" sign in CT diagnosis of blunt traumatic diaphragmatic rupture. AJR Am J Roentgenol. 2001;177(5):1137-40. https://doi.org/10.2214/ajr.177.5.1771137. [ Links ]
23. Ivatury RR, Simon RJ, Weksler B, Bayard V, Stahl WM. Laparoscopy in the evaluation of the intrathoracic abdomen after penetrating injury. J Trauma. 1992;33(1):101-9. https://doi.org/10.1097/00005373-199207000-00019. [ Links ]
24. Ochsner MG, Rozycki GS, Lucente F, Wherry DC, Champion HR. Prospective evaluation of thoracoscopy for diagnosing diaphragmatic injury in thoracoabdominal trauma - a preliminary report. J Trauma. 1993;34(5):704-10. https://doi.org/10.1097/00005373-199305000-00013. [ Links ]
 Correspondence:
Correspondence:
email: fragagp2008@gmail.com














