Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.60 n.1 Cape Town Mar. 2022
http://dx.doi.org/10.17159/2078-5151/2022/v60n1a3430
CASE REPORT
The value of MRCP in children with biliary symptomatology - an essential adjunct for safe cholecystectomy
L WeiI; S-L ZhangII; N XieI; C-M LiI; B-M FuI
IDepartment ofHepatobiliary and Pancreatic Surgery, The Second Affiliated Hospital of Kunming Medical University, China
IIDepartment of Hepatobiliary and Pancreatic Surgery, The First Affiliated Hospital of Kunming Medical University, China
SUMMARY
Congenital abnormalities of the biliary system are a consideration in children with biliary symptomatology. The preoperative diagnosis rate is still not satisfactory, despite progresses made in imaging technology, with the potential of biliary tract injury if surgery is indicated. The double gallbladder is a rare developmental abnormality of the biliary tract with several anatomical variations. This abnormality was accurately delineated in a 7-year-old child by MRI/MRCP, allowing the ductal anatomy to be accurately identified and safe laparoscopic cholecystectomies to be performed.
Keywords: double gallbladder, child, laparoscopic cholecystectomy
Case presentation
A 7-year-old girl presented with a 24-hour history of right upper quadrant pain. She had no significant medical or surgical history. Abdominal ultrasound suggested a bile duct cyst. Examination revealed mild tenderness in the right upper abdomen. Magnetic resonance imaging (MRI) and magnetic retrograde cholangiopancreatography (MRCP) showed a spherical cystic structure with sediment in the proximal portion of the gallbladder (GB) and connected to the common bile duct by a duct (Figure 1) in keeping with double GB. A laparoscopic cholecystectomy was performed. The second moiety was seen over the first and was partially embedded in the liver tissue. Careful dissection allowed safe identification of the fine anatomical structures associated with the GBs, one of which overlayed the proximal portion of the other and was partially embedded in liver tissue. The GBs had independent ducts that emptied into the common bile duct (Figure 2A) that was confirmed after resection was completed (Figure 2B). The pathologist confirmed the diagnosis of a double GB. The patient recovered well after surgery and continues to do well as of the most recent follow-up.
Discussion
The double GB, which occurs in about 1 of 4 000 births,1 was first described by Boyden, a Harvard surgeon, in 1926.2 The phenomenon is caused by abnormal development of the embryo during the fifth and sixth weeks of gestation. An accessory GB with a separate cystic duct is assumed to develop from the bile duct tree or hepatic ducts; two GBs with a common opening into the common bile duct arise from the cystic duct.3 Additionally, a hepatic diverticulum caudal bud that develops into the GB but splits into a separate outpouching and maintains the original connection leads to duplex or bilobed GBs.4
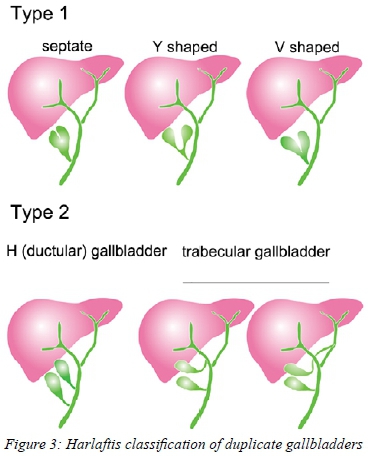
Classifications of the double GB were described by Boyden and Harlaftis. Boyden divided the double GB into three variations: a double GB possessing a common neck, a double GB with independent cystic ducts that merge prior to entering the bile duct tree, or a double GB with separate cystic ducts that merge into the biliary tree separately (accessory GB).2 Harlaftis proposed a more detailed classification: type 1 (the GBs enter the bile duct with a common cystic duct) includes septate, Y-shaped, or V-shaped, while type 2 (accessory GB) consists of an H (or ductular) GB or a trabecular GB.5 Harlaftis' classification is more instructive for clinical use and universally accepted. According to the Harlaftis classification, our case is a type 2 H double GB (Figure 3). The condition presents without any specific symptoms. Due to the multiple variations of the cystic duct connection to the biliary tract, the potential for common hepatic duct or bile duct injury during their removal is higher than in patients with normal anatomy, particularly if the abnormality is only detected at the time of cholecystectomy, which occurs in 50% of the cases. Ultrasound imaging has a high sensitivity for detecting double GBs, but misdiagnosis of an intrahepatic accessory GB as a cystic tumour of the liver is described.6 Ultrasound has lower diagnostic specificity when compared to MRCP. If the abnormality is detected on ultrasound, MRI/MRCP is performed not only to confirm the abnormality, but more importantly, to identify the relationship between the common bile duct, common hepatic duct, and cystic duct.7 If there remains doubt about the relationships of the key anatomical structures, then intraoperative cholangiography should be available rather than performing a preoperative endoscopic retrograde cholangio-pancreatography (ERCP) with its attendant risks.8 The precise role of more complicated inspection methods such as three-dimensional reconstruction may also be of assistance in selected cases.9
Whether a double GB is more prone to gallstone formation and inflammation is still controversial. Ghosh thought a double GB did not increase the chance of disease,8 while others are suspicious that it increases the risk of cholecystitis and cholelithiasis.10 The contractile function of the accessory GB was shown to be decreased, which may contribute to easier gallstone formation and GB inflammation.8
The double GB is a rare mutation of the biliary system. Surgeons and imaging specialists should be aware of the importance of preoperative diagnosis for this condition to avoid ductal injury. This case shows that preoperative examination, precise diagnosis and meticulous dissection of the cystohepatic triangle resulted in a successful uncomplicated resection of both moieties without ductal injury.
Ethical approval
Not applicable. Parents have signed a consent form for this case report and related picture materials to be used for publication.
Conflict of interest
The authors declare no conflict of interest.
Funding source
This study was funded by the Construction Project of the Second Affiliated Hospital of Kunming Medical University, Yunnan Province, Internal Organs-construction Projects (2016NS248, 2017NS281, 2017NS282, and 2017NS283). The funder had no role in the study design, data collection and analysis, the decision to publish, or the preparation of the manuscript.
REFERENCES
1. Ozgen A, Akata D, Arat A, et al. Gallbladder duplication: imaging findings and differential considerations. Abdom Imaging. 1999;24(3):285-8. https://doi.org/10.1007/s002619900496. [ Links ]
2. Boyden EA. The accessory gall-bladder - an embryological and comparative study of aberrant biliary vesicles occurring in man and the domestic mammals. Amer Jour Anat. 1926;38(2):177-231. https://doi.org/10.1002/aja.1000380202. [ Links ]
3. Kim RD, Zendejas I, Velopulos C, et al. Duplicate gallbladder arising from the left hepatic duct: report of a case. Surg Today. 2009;39(6):536-9. https://doi.org/10.1007/s00595-008-3878-4. [ Links ]
4. Kothari PR, Kumar T, Jiwane A, et al. Unusual features of gallbladder duplication cyst with review of the literature. Pediatr Surg Int. 2005;21(7):552-4. https://doi.org/10.1007/s00383-004-1355-8. [ Links ]
5. Harlaftis N, Gray SW, Skandalakis JE. The gallbladder: uncommon gallbladder conditions and unusual presentations of the common gallbladder pathological processes. Surg Gynecol Obstet. 1977;145(6):928-34. [ Links ]
6. Won JH, Choi SY, Lee HK, et al. Accessory gallbladder in an intrahepatic location mimicking a cystic tumour of the liver: a case report. Medicine (Baltimore). 2016;95(44):e5293. https://doi.org/10.1097/MD.0000000000005293. [ Links ]
7. Botsford A, Mckay K, Hartery A, Hapgood C. MRCP imaging of duplicate gallbladder: a case report and review of the literature. Surg Radiol Anat. 2015;37(5):425-9.nhttps://doi.org/10.1007/s00276-015-1456-1. [ Links ]
8. Ghosh SK. Laparoscopic cholecystectomy in double gallbladder with dual pathology. Minim Access Surg. 2014;10(2):93-6. https://doi.org/10.4103/0972-9941.129963. [ Links ]
9. Endo I, Matsuyama R, Mori R, et al. Imaging and surgical planning for perihilar cholangiocarcinoma. J Hepatobiliary Pancreat Sci. 2014;21(8):525-32. https://doi.org/10.1002/jhbp.75. [ Links ]
10. Gigot J, Beers BV, Goncette L, et al. Laparoscopic treatment of gallbladder duplication. Surg Endosc. 1997;11(5):479-82. https://doi.org/10.1007/s004649900396. [ Links ]
 Correspondence:
Correspondence:
B-M Fu
Email: fubimang@163.com














