Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.60 no.1 Cape Town mar. 2022
http://dx.doi.org/10.17159/2078-5151/2022/v60n1a3386
CASE REPORT
Double jeopardy avoided by thorough investigation
JJP BuitendagI; J FichardtII; DL ClarkeIII
IDepartment of Surgery, Tygerberg Hospital, Stellenbosch University, South Africa
IIDepartment of Surgery, Ngwelezana Hospital, University of KwaZulu-Natal, South Africa
IIIDepartment of Surgery, Pietermaritzburg Hospital Complex, University of KwaZulu-Natal, South Africa
SUMMARY
Penetrating junctional torso trauma with multiple and complex injuries presents the clinician with many investigational and management decisions.1-3 This situation has been termed double jeopardy in the literature.4-6 The management of this multiple gunshot victim's injuries - massive haemothorax and severe liver and kidney injuries - describes how this pathway can be negotiated with a successful outcome.6
Keywords: liver injury, double jeopardy, penetrating injury
Clinical case
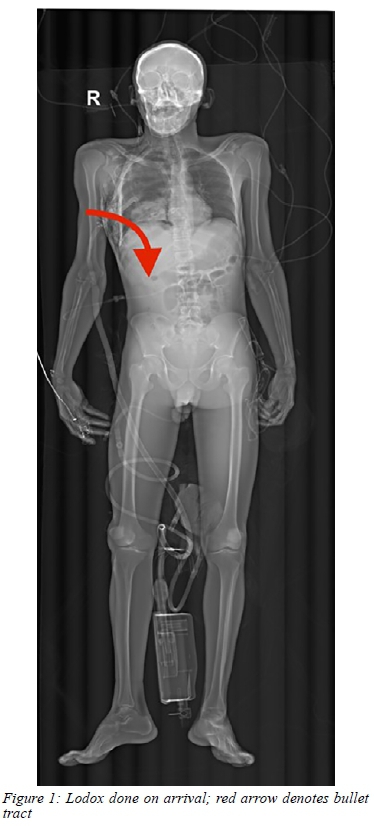
A 35-year-old man with multiple torso gunshot wounds presented to our large trauma unit. The gunshot wounds traversed the right chest and right flank. The patient was resuscitated according to advanced trauma life support (ATLS) guidelines. A right-sided intercostal drain (ICD) had been inserted at the referring clinic. The patient had been severely acidotic at the clinic and had drained 1 300 ml of blood from the ICD prior to arrival. He also had frank blood in his urinary catheter. On presentation, the patient had a good blood pressure, but deteriorated rapidly and drained a further 550 ml of blood from the ICD. The patient complained of abdominal pain and objectively had a tender right upper quadrant on examination. A focused assessment with sonography for trauma (eFAST) was performed. No pericardial effusion was seen. The abdominal views showed fluid in the abdominal cavity.
Based on these findings, a decision was made to open the abdomen first as it was thought that the liver was injured in combination with the diaphragm and that the output in the chest drain originated from a bleeding liver. He was expedited to the operating room (OR), where laparotomy revealed a right-sided lateral retroperitoneal haematoma, an actively bleeding American Association for the Surgery of Trauma (AAST) Grade V liver injury involving segments 5 and 7, and a right-sided diaphragmatic injury. The actively bleeding right kidney was removed and the liver packed. The patient continued to bleed and was re-explored. Significant bleeding from the tract of liver injury was noted. This was controlled by a Pringle manoeuver, and individual bleeding points were over sewn and packs reapplied. At this point, it was noted that the patient was coagulopathic. A temporary abdominal containment device was applied. In the intensive care unit (ICU) the patient was resuscitated using contemporary transfusion strategies guided by thrombo-elastography and was aggressively warmed. Once the patient had stabilised, formal angiography was performed to exclude any arterial extravasation or pseudoaneurysms of the hepatic arterial system. The packs were removed 72 hours after the index laparotomy. The patient had a complex course in ICU with several bouts of sepsis which ultimately required percutaneous drainage under imaging. He improved slowly and was discharged after 3 months.
Discussion
The question of which cavity to open in patients with thoraco-abdominal trauma is important. Three landmark studies on this topic showed an increase mortality if the wrong cavity is opened first and dubbed this double jeopardy.7-9 Thorough investigation should be done to determine all possible organ injuries taking into consideration all the possibilities and trajectories of penetrating injuries. Combined procedures (thoracotomy and laparotomy) are associated with increased morbidity and mortality.7,8 This reiterates the importance of decision making into which cavity to open first. In a study performed by Matsushima et al., they concluded that an eFAST was highly sensitive to determine whether the pericardium must be opened first; similarly, if fluid is present in the abdomen, one should explore the abdomen first. They did, however, reiterate that a negative eFAST of the abdomen does not exclude an abdominal bleeding source.9
The liver is the most commonly injured organ in blunt abdominal trauma and the second most commonly injured organ in penetrating abdominal trauma.1-3
The majority of hepatic injuries can be treated non-operatively.1,4,5 Interventional angiography should be performed if available, and should always be considered in high-grade blunt or penetrating thoraco-abdominal trauma as part of the management algorithm to identify arterial injuries that can be treated with angioembolisation.3 Operative intervention for liver injuries is needed in approximately 14% of patients.2,6 A thorough history and examination will aid in the diagnosis of hepatic injuries, but imaging modalities are the main diagnostic tool. eFAST, diagnostic peritoneal lavage (DPL), computerised tomography (CT) and angiography have been well described in the literature. Recent literature supports operative intervention only in haemodynamically unstable patients, usually as a result of a high-velocity gunshot wound. The only other indication for operative intervention is an associated hollow viscus injury.8 In patients presenting with penetrating right thoracoabdominal wounds in haemorrhagic shock with a right-sided massive haemothorax, there must be a suspicion of potential intra-abdominal pathology.7,9 This makes the surgical decision regarding which cavity to open extremely difficult.

This case highlights several aspects of the double jeopardy dilemma. High-grade liver injuries are associated with increased morbidity and mortality. Postoperative morbidity is mostly associated with the development of biliary leakage and abscess formation. Postoperative imaging with ultrasound and CT scan must therefore be performed if septic markers increase. Bile-leaks and abscesses can be treated non-operatively by percutaneous drainage and follow-up imaging is suggested to evaluate the resolution of these collections before discharge of the patient.5,6
Learning points
1. In patients with a massive haemothorax, the bleeding does not always originate from the thoracic organs.7
2. Performing the wrong initial surgery can lead to severe morbidity and mortality of a patient.8,9
3. Consider the trajectory of penetrating injuries and use eFAST to assist in the decision of which cavity to enter first.79
4. Damage control resuscitation and surgery is the gold standard for patients presenting haemodynamically unstable with massive haemorrhage.4
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding required.
Ethical approval
Patient consent was obtained.
ORCID
JJP Buitendag https://orcid.org/0000-0001-7169-129X
J Fichardt https://orcid.org/0000-0003-1636-6042
DL Clarke https://orcid.org/0000-0002-8467-1455
REFERENCES
1. Tinkoff G, Esposito TJ, Reed J, et al. American Association for the Surgery of Trauma Organ Injury Scale I - spleen, liver, and kidney, validation based on the National Trauma Data Bank. J Am Coll Surg. 2008;207(5):646-55. https://doi.org/10.1016/j.jamcollsurg.2008.06.342. [ Links ]
2. Kozar RA, Moore FA, Moore EE, et al. Western Trauma Association critical decisions in trauma - nonoperative management of adult blunt hepatic trauma. J Trauma. 2009;67(6):1144-9.https://doi.org/10.1097/TA.0b013e3181ba361f. [ Links ]
3. Hurtuk M, Reed RL 2nd, Esposito TJ, Davis KA, Luchette FA. Trauma surgeons practice what they preach - the NTDB story on solid organ injury management. J Trauma. 2006;61(2):243-54. https://doi.org/10.1097/01.ta.0000231353.06095.8d. [ Links ]
4. Malhotra AK, Fabian TC, Croce MA, et al. Blunt hepatic injury - a paradigm shift from operative to nonoperative management in the 1990s. Ann Surg. 2000;231(6):804-13. https://doi.org/10.1097/00000658-200006000-00004. [ Links ]
5. Moore EE, Cogbill TH, Jurkovich GJ, et al. Organ injury scaling - spleen and liver (1994 revision). J Trauma. 1995;38(3):323-4. https://doi.org/10.1097/00005373-199503000-00001. [ Links ]
6. Marr JDF, Krige JEJ, Terblanche J. Analysis of 153 gunshot wounds of the liver. Br J Surg. 2000;87(3):1030-4. https://doi.org/10.1046/j.1365-2168.2000.01487.x. [ Links ]
7. Hirshberg A, Wall MJ Jr, Allen MK, Mattox KL. Double jeopardy- thoracoabdominal injuries requiring surgical intervention in both chest and abdomen. J Trauma. 1995;39(2): 225-31. https://doi.org/10.1097/00005373-199508000-00007. [ Links ]
8. Clarke DL, Gall TM, Thomson SR. Double jeopardy revisited - clinical decision making in unstable patients with thoraco-abdominal stab wounds and potential injuries in multiple body cavities. Injury. 2011;42(5):478-81. https://doi.org/10.1016/j.injury.2010.06.027. [ Links ]
9. Matsushima K, Khor D, Berona K, et al. Double jeopardy in penetrating trauma: get FAST, get it right. World J Surg. 2018;42(1):99-106. https://doi.org/10.1007/s00268-017-4162-9. [ Links ]
 Correspondence:
Correspondence:
JJP Buitendag
Email: johan_buitendag@yahoo.com














