Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.60 no.1 Cape Town Mar. 2022
http://dx.doi.org/10.17159/2078-5151/2022/v60n1a3672
TRAUMA
Brachial artery injuries - the impact of the anatomical site of injury on postoperative outcomes
S MansorI, II; K AlshariefI; A AlmadanyI; A BuzajaI; A EltarhoniIII
IGeneral Surgery Department, Al-Jalaa Teaching Hospital, Benghazi University, Libya
IIDepartment of Surgery, Libyan International Medical University, Libya
IIIDepartment of Family and Community Medicine, Benghazi University, Libya
ABSTRACT
BACKGROUND: The start of the armed conflicts in Libyan society in 2011 led to a dramatic increase in the incidences of unusual types of brachial artery injuries, which were previously uncommon. In this study, the postoperative outcomes have been compared prospectively between patients who have had injuries at the proximal anatomical half of the brachial artery with those who suffered injuries at the distal anatomical half
METHODS: A cohort study was undertaken to compare patients who had an injury at the proximal anatomical half of the brachial artery (considered as the first group) and patients who had an injury at the distal anatomical half of the brachial artery (considered as the second group). This was undertaken to analyse the influence of the anatomical site of injury on the postoperative outcomes in patients who underwent urgent surgical repair procedures at the hospital from February 2011 to December 2016
RESULTS: Out of fifty-one patients, 31 (60.8%) patients had gunshot injuries, 12 (23.5%) had explosive injuries, four (7.8%) had stab wounds and four (7.8%) were victims of road traffic accidents. There were 13 (25.5%) patients in the first group and 38 (74.5%) patients in the second group. Three patients (5.9%) had postoperative arterial occlusion due to thrombosis, while two (3.9%) had postoperative graft occlusion due to thrombosis; the other two (3.9%) had compartment syndrome
CONCLUSION: Based on the anatomical background, critical limb ischaemia and postoperative ischaemic complications, as well as delayed limb amputation, are more associated with the injuries to the proximal anatomical half of the brachial artery due to poor collateral circulation at this level
Keywords: brachial artery, gunshot injury, arterial repair, limb ischaemia, venous graft
Introduction
Brachial artery injuries were previously uncommon in Libyan society and were mainly caused by industrial and road traffic accidents. However, during the past decade, due to the political changes in the country, there has been widespread acquisition of weapons in the hands of unauthorised individuals, which has led to the start of armed civilian conflicts. All these circumstances have resulted in a dramatic increase in the incidences of brachial artery injuries as part of vascular injuries, with gunshots and explosives as the current main causes. Previous literature had reported that only 3.3% of patients admitted to hospitals with upper-extremity trauma had suffered a concomitant arterial injury.1 In general, we can classify limb trauma into two types: blunt trauma, which mainly leads to partial or complete intimal disruption of the artery, usually occurring in a road traffic accident; and the penetrating injury which may occur as a result of either low energy trauma, such as glass or stab wound injuries or high energy trauma, such as gunshots and explosive injuries. In comparison to penetrating injuries, blunt traumas are more frequently associated with concomitant neurological and orthopaedic injuries that lead to significant rates of limb disability.2,3 In upper-limb traumas with concomitant vascular injuries, approximately half of the cases had an injury in the brachial artery.4
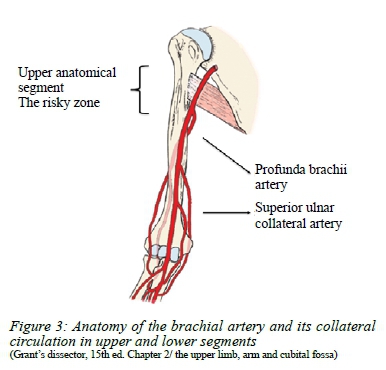
The brachial artery is considered the main blood supply for the arm; it begins at the lower border of the teres major muscle. It is wholly superficial, covered by skin and deep fasciae, which explains the high risk of injury, as well as the easy clinical diagnosis of the injury. The upper segment of the artery lies on the triceps brachii muscle. The standard surgical approach is between the biceps and triceps brachii muscle, formed on the medial aspect of the arm, and it can proximally extend to the deltopectoral groove for more proximal control on the axillary artery. In the middle segment, the brachial artery runs along a line from the medial lip bicipital groove and overlaps from the lateral side by the coracobrachialis, biceps muscle, and the bicipital aponeurosis that crosses its lower segment. The profunda artery arises from the upper anatomical segment of the brachial artery and follows the radial nerve into the spiral groove of the humerus, while the superior ulnar collateral artery arises near the middle of the upper arm, and the inferior ulnar collateral artery arises near the termination of the artery and becomes part of the anastomosis around the elbow joint.
In the current cases, it has been noted that the different anatomical sites of the injury result in different rates and severity of postoperative complications. Therefore, in this study, we have prospectively compared the postoperative outcomes between patients who have had an injury at the proximal anatomical half of the brachial artery with those who have had an injury at the distal half. This has helped to analyse the influence of the anatomical site of injury on the short-term postoperative outcomes in fifty-one consecutive patients who underwent urgent surgical repair procedures of the brachial artery at the hospital from February 2011 to December 2016.
Material and methods
A cohort study was conducted to compare patients who had an injury at the proximal anatomical half of the brachial artery (the first group) and patients who had an injury at the distal anatomical half of the brachial artery (the second group). Subsequently, it was possible to analyse the influence of the anatomical site of brachial artery injuries on the short-term postoperative outcomes in all consecutive patients who had undergone urgent vascular reconstruction procedures following brachial artery injuries from 17 February 2011 to 31 December 2016 in the Department of Surgery. Table I demonstrates the baseline characteristics of the patients in both groups included in the study.
All patients were resuscitated following the protocols of the advanced trauma life support of the American College of Surgeons. The diagnosis of brachial artery injuries depends mainly on clinical examinations - all injuries within the arm or cubital fossa are associated with active arterial bleeding, in addition the absence of distal pulses was diagnosed as a brachial artery injury. Further investigations also revealed decreased oxygen concentration on the pulse oximeter, absent pulse sound on a bedside Doppler test and a significant decrease or absent arterial systolic flow on an arterial duplex ultrasound. In some selected cases computed tomography angiography findings were also used. All these findings were considered to be diagnostic for brachial arterial injuries. All the patients who had crushed limb injuries and required immediate limb amputation as a life-saving procedure were excluded, together with multi-trauma patients with massive bleeding and high mortality rates within the first 48 hours.
The arterial reconstruction operation is divided into three steps. The first step is to control the bleeding by artery exploration and clamping of both injured ends. This step is preceded by the intravenous administration of heparin 5 000 I.U. to reduce the risk of thrombosis arising from the stasis of blood post-clamping. The second step is an open reduction and external fixation procedure of the fractured bones by the orthopaedic team, if there are any concomitant bone fractures. The third step is the reconstructive procedure of the injured artery in order to enable the return of normal limb perfusion, and necrotic tissue debridement; washing of the injured field is performed after the arterial injury repair. This method of management was adopted with the intention to reduce the manipulation of the freshly repaired artery when performing the bone fixation procedure. The arterial reconstruction and return of blood supply to the injured arm in all cases occurred in a time of six hours, with the average time for installing the external fixator in our cases was 32 minutes. Although it has been suggested that arterial repair should be conducted before skeletal stabilisation to prevent prolonged tissue ischaemia,5,6 our management method has proven to produce high success rates in this study.
Ligation of injured veins was carried out in the vast majority of cases, while the fasciotomy decision was dependent on the intraoperative situation, with the aim of avoiding compartment syndrome. The primary repair of the injured peripheral nerve was completed when possible. Meanwhile, in the postoperative time, the patients received intravenous heparin as anticoagulant therapy, which was then replaced with an aspirin tablet to reduce the risk of postoperative thrombosis in narrow diameter blood vessels, along with antibiotic coverage and pain therapy. Patients were placed under high observation measures of limb viability through repeated evaluation of the limb by clinical examinations, pulse oximeter, a bedside Doppler test, and arterial duplex ultrasound.
Patients' data were also collected, such as age, gender, past medical history, type of injury, associated injured organs, methods of diagnosis, surgical procedures, postoperative complications, the indication of re-operation and procedures in re-operation. Later, all patients were under postoperative follow-up for morbidity and disabilities. The primary target was to note any short-term postoperative complications, and consequently, to confirm the degree of the long-term postoperative functional disabilities of the limb through neurological examination. All continuous variables were expressed as mean ± standard deviation (SD), with the categorical data expressed as frequency and percentage. Comparisons between groups were made using the X2 test or Fisher's exact test for categorical variables, as appropriate. Statistical analyses were performed using the SPSS v21 statistical software, and p-values < 0.05 were considered statistically significant.
Informed consent was also necessary in order to conduct the study, as the hospital is a teaching university hospital. Written informed consent was routinely obtained from all admitted patients or legally authorised representatives during hospital stays and prior to their inclusion in the study. This enabled the use of patients' data, as well as their operative photos, and for the findings to be published in academic activities and research. Ethical approval was obtained from the Institutional Review Board (IRB) of the Al-Jalaa Teaching Hospital, Benghazi University.
Results
In the current study, out of 51 patients, 50 (98%) were male and one (2%) was female, with a mean age of 29.49 years. Brachial artery injuries were caused by gunshots in 31 (60.8%) patients, explosive injuries in 12 (23.5%) patients, stab wounds in four (7.8%) patients and road traffic accidents in four (7.8%) patients. Thirteen (25.5%) patients had brachial artery injuries at the upper anatomical half (the first group); while the second group comprised of 38 (74.5%) patients who had injuries to the lower anatomical half of the brachial artery. Forty-six (90.2%) operations were conducted as limb-saving procedures to return limb perfusion; three of them (5.9%) had preoperative angiography to confirm the diagnosis of the injuries. Separately, five operations (9.8%) were carried out as life-saving procedures due to the active bleeding in the upper-part of the injured artery, and one operation (2%) was completed as debridement without vascular repair.
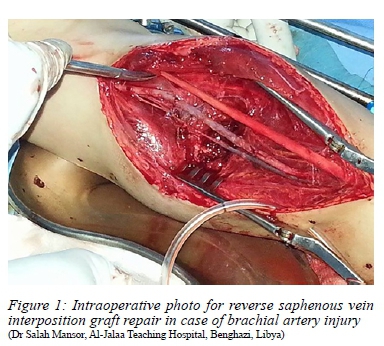
Arterial reconstruction was performed in 24 (47.1%) operations as reverse saphenous vein interposition grafts (Figure 1), primary end-to-end anastomosis in 16 (31.4%), simple repair in four (7.8%), and a Dacron interposition graft in three (5.9%). The synthetic graft was used only when the great saphenous vein from both sides was unsuitable because of its narrow diameter. Arteriotomy with thrombectomy was evident in two (3.9%), and false aneurysm excision with a simple repair in one (2%) operation. Debridement of necrotic tissue without vascular repair was undertaken in only one operation (2%), as that particular patient was admitted to the hospital after more than 48 hours following the onset of injury with a viable limb and associated long segment thrombosis at both ends of the injured artery.
Venous concomitant injuries are usually suspected in penetrating trauma of the arm, due to relatively small arm tissue volume, and the close proximity of organs, and discovered during surgical exploration. In the current study, a concomitant venous injury was seen in 37 (72.5%) patients, with one case treated by brachial vein primary end-to-end anastomosis, while three patients were treated by venous simple repair, and the rest of the 33 (64.7%) patients were treated by ligation of the injured vein. Other concomitant soft tissue damage was also seen in 40 (78.4%) patients, 22 (43.1%) of whom had humerus bone fractures. Peripheral nerve tissue injuries contributed to permanent upper-limb disabilities of a significant percentage (79%) of the injured patients.7
Postoperative complications were observed in seven (13.7%) patients; three (5.9%) had postoperative arterial occlusion due to thrombosis; two (3.9%) had postoperative graft occlusion due to thrombosis; and two (3.9%) patients had postoperative compartment syndrome. Re-operations were reported in seven (13.7%) patients in both groups. Five patients were from the first group, and two of them had postoperative arterial occlusion due to thrombosis, which was treated with re-exploration and reverse saphenous vein interposition graft repair. Nevertheless, one of them still had delayed limb amputation. The other two patients in the same group had postoperative compartment syndrome treated with an emergency fasciotomy; similarly, one of them had to receive delayed limb amputation. The last patient in the group had postoperative venous graft occlusion due to thrombosis treated with re-exploration and Dacron interposition graft repair; this complication ended with a delayed limb amputation. In the second group, one patient had postoperative venous graft occlusion due to thrombosis, while the other patient had postoperative arterial occlusion due to thrombosis, and both were treated with re-exploration and thrombectomy (Table II).
Disability of the limbs was significantly evident throughout the long-term follow-up in 43 (84.3%) patients. The limbs were amputated in three patients and weak limbs were evident in the remainder of the patients due to permanent damage of the peripheral nerve. This was detected by clinical neurological examinations and further confirmed by electromyography.
Discussion
Vascular injuries due to upper-extremity trauma were considered to be uncommon;1,8,9 while the brachial artery was the most affected artery in upper-extremity trauma.4,8,10,11 In Libyan society, there is clear evidence from collected data that the incidence of vascular injuries to the upper extremities has increased rapidly in the last ten years. Figure 2 shows the rate of brachial artery injuries in the period 2007-2016 at Al-Jalaa Hospital. Further, the type of the brachial artery injury and its outcome had previously been considered dependent on the mechanism of injury, such as penetrating injuries in industrial settings, or blunt injuries caused by road traffic accidents, as well as in supracondylar fractures or dislocation of the humerus bone, resulting in the injury of the brachial artery.12 Recently, the widespread use of weapons and multi-conflict spots in the world has led to the appearance of other types of penetrating injury mechanisms with high volume energy due to gunshots and injuries caused by explosions. Hence, penetrating injuries are now considered the most common cause of vascular injury in upper-extremities, even among civilians.13
Brachial artery injuries can be easily diagnosed by clinical examinations in the majority of cases, due to the superficial position of the artery. Active arterial bleeding at the injured site, weak or absent radial pulses, a pale cold limb, reduced oxygen concentration in the pulse oximeter and a significant decrease or absence of sound signs in a bedside Doppler test were all considered signs of brachial artery injuries. With the clinical signs, the diagnosis and decision are supported by arterial duplex ultrasound examination, as many previous international studies have concluded that arterial duplex ultrasonography is a non-invasive, cost-effective, and easy bedside test; it reported 99% sensitivity and 98% accuracy in the diagnosis of brachial artery injuries.14,15 Computed tomography angiography was used in only three cases with occlusive non-bleeding injuries to confirm the diagnosis, despite the controversial discussion in previous research studies regarding the limited role of angiography in the diagnosis of brachial artery injuries in upper-arm traumas.1,4,16
To provide a clear explanation of the mechanism and pathophysiology of the penetrating gunshot injuries of the upper-extremities, a good understanding of the anatomical background and its features is required. Because of the relatively small surface area of the arm and close anatomical relationship of the brachial artery, vein, and median nerve, a high volume of trauma, in addition to the arterial injury, is caused by a bullet passing through the arm tissue; it produces a high risk of venous nerve injuries and fractures of the bone with widespread muscular destruction that may lead to functional disabilities with permanent neurological deficits of the upper-limbs. This is relevant even after maintaining the viability of limbs by successful arterial repair16,17 as well as peripheral nerve tissue repair.18,19
In the current study, we have observed that the outcome of penetrating brachial artery injuries is strongly dependent on the anatomical site of arterial injuries. This fact is also related to the anatomical background of the brachial artery. The brachial artery has a good size branch arising at the middle third of the artery, as well as the profunda brachii artery together with the other branches. Superior ulnar collateral and inferior ulnar collateral artery forms very good collateral anastomosis around the elbow joint (Figure 3). This explains the very low risk of limb ischaemia and amputation, due to its rich collateral circulation in the lower part of the arm in most patients.9,20,21
We have also observed that all the patients who suffered postoperative limb-threatening complications with various ischaemic changes had an injury to the upper-anatomical half of the brachial artery. All those patients had emergency limb-saving surgical re-exploration, and two of them ended with delayed limb amputation. Meanwhile, all the complications that occurred in patients who had injuries at the lower anatomical half of the brachial artery, including postoperative graft occlusion, showed no effect on limb viability. A patient came to the clinic after more than 48 hours of suffering a penetrating injury of the brachial artery in the lower third at cubital fossa with a viable limb. In the operative exploration of the artery in this patient, the intraoperative finding was a good viable muscle and soft tissue, with complete transection of the brachial artery, with non-bleeding constricted both ends, and a long segment of old thrombus in both arterial segments. As a result, superficial debridement, tissue washing, and open wound management were undertaken.
The viability of the limb was totally dependent on the appropriate arterial anastomosis and collateral, which in turn supplies the distal part of the limb. The data from the current study confirmed that the risk of ischaemic postoperative complications following brachial artery injuries, which ended with delayed upper-limb amputation, depended on the injury site located at the level of the origin of the profunda brachii artery and the anatomical segment above the proximal half of the arm. Figure 3 shows the anatomy of the proximal segment of the brachial artery with poor collateral circulation. Separately, at the anatomical level below this point, with the presence of good collateral circulation around the elbow joint, the risk of limb ischaemia is very low, even in case of injury to the lower-anatomical segment of the brachial artery. In the current study, there was a significant clinical and statistical difference between the anatomical site of brachial artery injuries and the rate of ischaemic postoperative complications (p = 0.003). Moreover, there was a significant statistical difference between the anatomical site of brachial artery injuries and the risk of delayed postoperative upper-limb amputation (p = 0.002).
Due to concomitant venous injuries, there is widespread soft tissue damage and fractures of the humerus bone in cases of gunshots and injuries caused by explosions; there is clear evidence of a high incidence of irreversible functional disability of the limbs, even after the successful arterial repair within six hours of injury.1,16 Previous international studies have reported that the rates of long-term functional disability of the upper limbs after penetrating injuries range from 27 to 44%,22 while in the current study, the rates were 72.9%. The relatively high percentage of long-term functional disability in this study was due to the fact that the aetiology in most of the cases was high energy trauma by gunshot and explosion injuries. There is still controversy regarding the timing of nerve tissue repair, due to the different mechanisms of injuries and the wide range of tissue injuries.18,19
In addition, in the current study, there were no significant clinical and statistical differences between the site of the brachial artery injury in the proximal or distal anatomical segment and the degree of postoperative functional disability (p = 0.396) due to the permanent neurological deficit. All cases of the study are still in the follow-up stage to observe and compare the long-term postoperative outcomes and final state of functional disability after the operative management of peripheral nerve injuries.
Conclusion
Based on the anatomical background, critical limb ischaemia, postoperative ischaemic complications, as well as delayed limb amputation, are more associated with the injury to the proximal anatomical half of the brachial artery due to poor collateral circulation at this level.
Acknowledgements
We would like to thank the Radiology, Anaesthesia and Biostatistics Department, Al-Jala Teaching Hospital, Benghazi University.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Ethical approval was obtained from the Institutional Review Board (IRB) of the Al-Jalaa Teaching Hospital, Benghazi University (C15/21).
ORCID
S Mansor https://orcid.org/0000-0001-9878-4277
K Alsharief https://orcid.org/0000-0002-2615-0766
A Almadany https://orcid.org/0000-0001-5582-0784
A Buzaja https://orcid.org/0000-0002-1875-9862
A Eltarhoni https://orcid.org/0000-0002-0237-0692
REFERENCES
1. Pillai L, Luchette FA, Romano KS, Ricotta JJ. Upper extremity arterial injury. Am Surg. 1997;63(3):224-7. [ Links ]
2. Brown KR, Jean-Claude J, Seabrook GR, Towne JB, Cambria RA. Determinates of functional disability after complex upper extremity trauma. Ann Vasc Surg. 2001;15(1):43-8. https://doi.org/10.1007/BF02693799. [ Links ]
3. Manord JD, Garrard CL, Kline DG, Sternbergh WC, Money SR. Management of severe proximal vascular and neural injury of the upper extremity. J Vasc Surg. 1998;27(1):43-7. https://doi.org/10.1016/S0741-5214(98)70290-3. [ Links ]
4. Fingerhut A, Leppaniemi AK, Androulakis GA, et al. The European experience with vascular injuries. Surg Clin North Am. 2002;82(1):175-88. https://doi.org/10.1016/S0039-6109(03)00147-6. [ Links ]
5. Hunt CA, Kingsley JR. Vascular injuries of the upper extremity. South Med J. 2000;93(5):466-8. https://doi.org/10.1097/00007611-200093050-00004. [ Links ]
6. McHenry TP, Holcomb JB, Aoki N, Lindsey RW. Fractures with major vascular injuries from gunshot wounds - implications of surgical sequence. J Trauma. 2002;53(4):717-21. https://doi.org/10.1097/00005373-200210000-00016. [ Links ]
7. Rich NM, Spencer FC. Vascular trauma. Philadelphia: WB Saunders; 1978. p. 125-56. [ Links ]
8. Franz RW, Goodwon RB, Hartman JF, Wright ML. Management of upper extremity arterial injuries at an urban level 1 trauma centre. Ann Vasc Surg. 2009;23(1):8-16. https://doi.org/10.1016/j.avsg.2008.04.012. [ Links ]
9. Sparks SR, DeLaRosa J, Bergan JJ, Hoyt DB, Owens EL. Arterial injury in uncomplicated upper extremity dislocations. Ann Vasc Surg. 2000;14(2):110-3. https://doi.org/10.1007/s100169910020. [ Links ]
10. Joshi V, Harding GE, Bottoni DA, Lovell MB, Forbes TL. Determination of functional outcome following upper extremity arterial trauma. Vasc Endovascular Surg. 2007;41(2):111-14. https://doi.org/10.1177/1538574406291338. [ Links ]
11. Kohli A, Singh G. Management of extremity vascular trauma - Jammu experience. Asian Cardiovasc Thorac Ann. 2008;16(3):212-24. https://doi.org/10.1177/021849230801600307. [ Links ]
12. McCready RA. Upper extremity vascular injuries. Surg Clin North Am. 1988;68(4):725-40. https://doi.org/10.1016/S0039-6109(16)44582-2. [ Links ]
13. Orcutt MB, Levine BA, Gaskill HV, Sirinek KR. Civilian vascular trauma of the upper extremity. J Trauma. 1986;26(1):63-7. https://doi.org/10.1097/00005373-198601000-00012. [ Links ]
14. Bynoe RP, Miles WS, Bell RM, et al. Non-invasive diagnosis of vascular trauma by duplex ultrasonography. J Vasc Surg. 1991;14(3):346-52. https://doi.org/10.1016/0741-5214(91)90087-B. [ Links ]
15. Shanmugam V, Velu RB, Subramaniyan SR, Hussain SA, Sekar N. Management of upper limb arterial injury without angiography - Chennai experience. Injury. 2004;35(1):61-4. https://doi.org/10.1016/S0020-1383(03)00237-7. [ Links ]
16. Ergünes K, Yilik L, Özsöyler I, et al. Traumatic brachial artery injuries. Tex Heart Inst J. 2006;33(1):31-4. [ Links ]
17. Visser PA, Hermreck AS, Pierce GE, Thomas JH, Hardin CA. Prognosis of nerve injuries incurred during acute trauma to peripheral arteries. Am J Surg. 1980;140(5):596-9. https://doi.org/10.1016/0002-9610(80)90037-9. [ Links ]
18. Nichols JS, Lillehei KO. Nerve injury associated with acute vascular trauma. Surg Clin North Am. 1988;68(4):837-52. https://doi.org/10.1016/S0039-6109(16)44589-5. [ Links ]
19. Cikrit DF, Dalsing MC, Bryant BJ, et al. An experience with upper-extremity vascular trauma. Am J Surg. 1990;160(2):229-33. https://doi.org/10.1016/S0002-9610(05)80313-7. [ Links ]
20. Zellweger R, Hess F, Nicol A, et al. An analysis of 124 surgically managed brachial artery injuries. Am J Surg. 2004;188(3):240-45. https://doi.org/10.1016/j.amjsurg.2004.02.005. [ Links ]
21. McCroskey BL, Moore EE, Pearce WH, et al. Traumatic injuries of the brachial artery. Am J Surg. 1988;156(6):553-5. https://doi.org/10.1016/S0002-9610(88)80551-8. [ Links ]
22. Hardin WD Jr, O'Connell RC, Adinolfi MF, Kerstein MD. Traumatic arterial injuries of the upper extremity - determinants of disability. Am J Surg. 1985;150(2):266-70. https://doi.org/10.1016/0002-9610(85)90134-5. [ Links ]
 Correspondence:
Correspondence:
S Mansor
Email: salah.mansor@uob.edu.ly














