Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.60 no.1 Cape Town Mar. 2022
http://dx.doi.org/10.17159/2078-5151/2022/v60n1a3192
CARDIAC SURGERY
A South Africa tertiary centre experience with redo mitral valve replacement
D KistanI; M BooysenI; G AlexanderII; TE MadibaI
IDepartment of General Surgery, University of KwaZulu-Natal, South Africa
IIDepartment of Cardiothoracic Surgery, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: Severe cardiac failure from mechanical mitral valve thrombosis due to poor warfarin control is a major cause of emergency redo mitral valve replacement (MVR) in South Africa. This study aimed to review the outcomes of redo MVR in patients presenting with mitral valve failure to a tertiary South African centre
METHODS: Retrospective chart review of patients undergoing redo MVR over a 10-year period (2005-2014). Patient demographics, aetiology of valve dysfunction, preoperative clinical assessment and outcomes were analysed
RESULTS: Sixty-four patients had 80 mitral valve procedures. The M:F ratio was 1:2.8 and the median age was 18 (IQR 14-28.5) and 25 (iQR 18-40) at initial surgery and at redo surgery, respectively. Median interval between original and redo MVRs was 47.5 (IQR 7.5-124) months. Rheumatic valve disease was the original pathology in 58 patients (90.6%). Fifty-two patients underwent a single redo MVR and 12 patients had multiple redo MVRs. Fifty-eight (72.5%) were emergency redo procedures. Prosthetic valve thrombosis was present in 73.8%. Ten patients (15.6%) developed postoperative complications. The median hospital stay and ICU stay were 19 (IQR 12-27.5) days and 4 (IQR 3-7) days, respectively. Two patients died in the postoperative period (3.1%). The mean patient follow-up was 42 months. Three patients died during follow-up
CONCLUSION: The majority of redo MVR procedures were undertaken as an emergency with valve thrombosis being the most common aetiology. The mortality rate was 3.1% and postoperative complication rate was 15.6%
Keywords: mitral valve replacement, mitral valve procedure, redo surgery
Introduction
Acute rheumatic fever and rheumatic heart disease (RHD) remain major public health concerns worldwide, resulting in over 233 000 deaths annually.1 While the incidence has significantly decreased in high-income countries (HICs), it remains a major health burden in low- and middle-income countries (LMICs) and continues to cause significant morbidity and mortality.1,2 In Africa, rheumatic fever and RHD are the most common aetiology of valvular heart disease in patients requiring valve surgery,3 whereas in HICs degenerative disease is the most common aetiology requiring valve surgery.4 The estimated annual incidence of new cases of RHD in Soweto, South Africa, is approximately 23.5 cases per 100 000 people over 14 years of age. In view of these differences between HIC and LMICs, the spectrum of RHD in LMICs and its treatment cannot be generalised to that of HICs.5
One of the commonly utilised procedures for the treatment of severe mitral valve disease is mitral valve replacement (MVR).3 MVRs are at risk for prosthetic valve dysfunction2,6,7 requiring redo valve surgery. There is a deficit in the literature documenting patient outcomes following redo valve procedures in the African setting. In order to add to the existing knowledge of redo MVR, especially in LMICs, we undertook this retrospective observational study in order to benchmark a tertiary South African centre's experience of redo MVR.
Methods
The study was conducted in the Department of Cardiothoracic Surgery at Inkosi Albert Luthuli Central Hospital (IALCH), a tertiary referral hospital located in Durban, KwaZulu-Natal province, South Africa. The department provides the only cardiothoracic unit serving 10 million people in the province. All patients who underwent redo MVR over a 10-year period from January 2005 to December 2014 were included. Patient data at IALCH are kept in a password-protected hospital information management system (Soarian®, Siemens Medical Solutions, Malvern USA). Patients were identified from the cardiothoracic surgery theatre record books. Using the patients' name and hospital number, their files were then accessed from the Soarian® programme. Patients with insufficient and incomplete hospital records were excluded from the analysis.
The study was a descriptive retrospective analysis. STROBE statement was adhered to in this methodology. Information collected included patient demographics, pre-operative clinical assessment, international normalised ratio (INR), albumin, HIV status, operative findings and surgical outcomes. The data were subsequently recorded in a Microsoft Excel spreadsheet and analysed using Microsoft Excel. Since IALCH is a tertiary hospital, patients are followed up at the base hospitals and generally reviewed at IALCH one month postsurgery, then at 6 or 12 monthly intervals or when deemed necessary. Compliance with warfarin therapy was defined as documented therapeutic values of the INR within an acceptable therapeutic range of 2.0-3.0.7 The timing of redo MVR was guided by the clinical symptoms or the severity of valve obstruction as determined following echocardiography at valve screening. Redo surgical procedures as a consequence of valve thrombosis in patients who show haemodynamic compromise are undertaken as an emergency. All patients were managed in the intensive care unit after surgery. Outcome variables included pathology of the valve dysfunction, morbidity and mortality. No statistical analyses were undertaken for this study.
Results
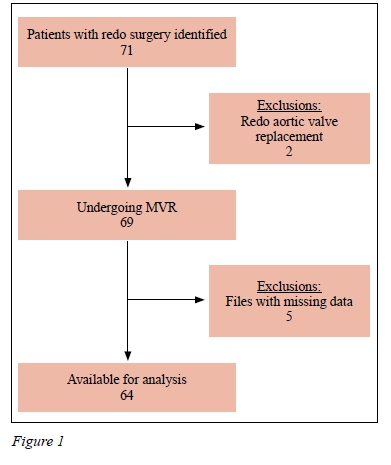
Of the 71 patients initially identified, 64 fulfilled the criteria for inclusion (Figure 1). Forty-seven (73.4%) were females yielding a male to female ratio of 1:2.8. The median age at initial valve replacement was 18 years (IQR 14-28.5) and that at presentation for redo surgery was 25 years (IQR 18-40). Fifteen patients were HIV-positive, 46 were HIVnegative and the HIV status was unknown in three patients. The median CD4 cell count for HIV-positive patients was 478 cells/mm3 (range 173-929). The aetiology of native valve dysfunction was rheumatic valvular heart disease (59; 92.2%) congenital heart disease (3; 4.7%), chordal rupture due to myocardial infarction (MI) (1; 1.6%), and the aetiology was unknown in one patient (1.6%). Mechanical valves were used in all the original MVR.
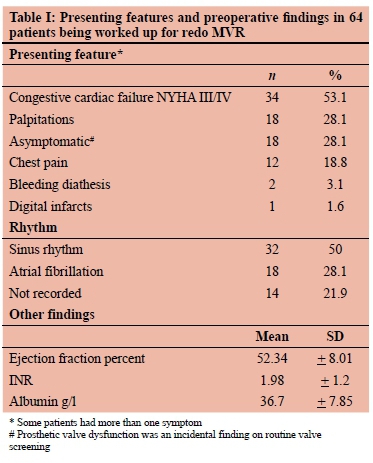
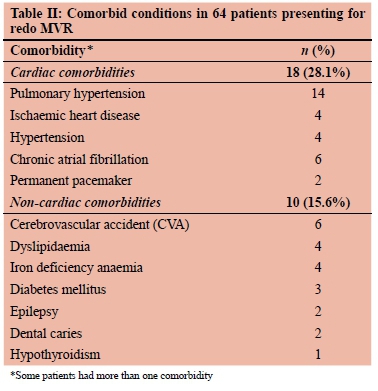
The median interval between the original surgical procedure and the redo procedure was 47.5 months (IQR 7.5-124). Table I shows presenting features, clinical findings and results of investigations. The most common presenting feature for redo surgery was congestive cardiac failure. As shown in Table II, 28 patients had comorbidities of which 18 were cardiac related comorbidities and 10 were non-cardiac comorbidities. The INR was noted to be within the acceptable therapeutic range in 41 patients.
Fifty-two of the 64 patients underwent a single redo MVR. Twelve patients (18.8%) with a median age of 22 years had multiple redo operations (two in 10 patients and three in two patients). Eighty redo procedures were performed. Fifty-five patients underwent 58 emergency redo procedures (72.5%) and 19 patients underwent 22 elective redo procedures (27. 5%).
Pathological findings of the dysfunctional prosthetic valves are shown in Table III. Prosthetic valve thrombosis was the most common finding accounting for 59 of the 80 redo procedures (73.75%). The other prosthetic valve pathologies were less frequent. Thirty-one of the 45 HIV-negative patients (68.89%) and twelve of the 15 HIV-positive patients (80%) had prosthetic valve thrombosis. Prosthetic valve thrombosis accounted for 25 of 26 multiple redo procedures. The 18 patients with prosthetic valve dysfunction were asymptomatic at presentation and the valve dysfunction was an incidental finding on routine valve screening. Table IV shows the types of valves used for replacement.

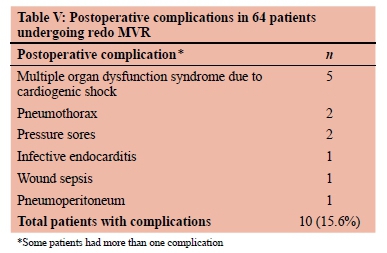
Eleven patients (16.9%) developed postoperative complications (Table V). The median hospital stay was 19 (IQR 12-27.5) days, and the median ICU stay was 4 days. The median patient follow-up was 42 (IQR 11-66) months. Five patients died; two patients in the immediate postoperative period (in-hospital mortality rate of 3.1%) and three patients died following discharge.
Discussion
While this study shares some similarities with the current international literature on MVR surgery, it does highlight a few significant contrasts. The native valve pathology was rheumatic heart valvular disease in the vast majority of the patients, which reflects the early predominance of RHD in the population served. Epidemiological studies from LMIC have shown that RHD remains the major underlying aetiology requiring MVR.1-589 In contrast, studies from the international literature show that the common aetiology for valvular heart disease in HICs is degenerative disease.4,10 The preponderance of rheumatic heart valvular disease in this series reflects the prevailing evidence that RHD remains common in Africa, whereas its incidence is waning in HICs.1,3 Indications for redo MVR in HICs include prosthetic valve endocarditis, paravalvular leaks and valvular degenerative disease,6,711-13 whilst patients requiring valve surgery for RHD tend to be in the minority at 11%.14
The spectrum of clinical presentation for redo procedures was similar to that reported in the literature. The majority of the patients had no general comorbidities and the low rate of 28% is a reflection of a younger population in our setting. Although this study showed a female preponderance, there is no clear trend in the literature, with some studies favouring males,15 others favouring females8,13,14,16 and still more showing an equal sex incidence.7
The median age at the time of initial and redo surgery in this series was 18 years and at 25 years, respectively. This is younger than that reported in an Indian study of 23.6 years for the primary operation and 36 years for re-operation.17 In comparison, international studies report an average age of 42-61 years for the primary operation18 and 54-72 years for the redo operation.7,13,14,18 Evidence suggests that in Africa, RHD has demonstrated a particular prevalence in the younger African population.3,19,20 However, there is no plausible explanation for occurrence of RHD at a younger age in Africa. Studies specifically investigating the reason for the development of RHD at a younger age in Africa are strongly needed. We believe that the young age at presentation in this series reflects this particular trend and supports the findings that there is a large and complex burden of newly diagnosed RHD in young adults in LMICs, warranting urgent attention of the public health and research community in these countries.
The mean duration of 47.5 months between initial MVR and redo surgery was much shorter than the 96-168 month period reported in the literature,7,13,16,17,21 suggesting that the development of valve dysfunction is more rapid in our setting. Valve dysfunction in our setting is predominantly due to valve thrombosis. The 19% rate of multiple redos in this series, again due to thrombosis, is above the 8-17.5% reported in the literature.15,22
The use of tissue valves in the young is somewhat controversial.23 They are not usually a feasible option in the young patient due to the well described incidence of rapid valve deterioration, leading to early redo surgery.24,25
Rheumatic valvular heart disease causes progressive fibrotic thickening of the mitral valve leaflets and subvalvular apparatus. Mitral valve repair in all patients with rheumatic valvular heart disease is preferable and should be undertaken if feasible.26 Unfortunately, expertise is lacking worldwide, and as such, this is usually only undertaken in limited centres of excellence which are non-existent in South Africa.
Of concern in this study was the high number of emergency operations at 86%, which is higher than the 5073% reported from other African countries1216 and markedly higher than the 20-59% seen in series from HICs,4,6,9 Although we did not specifically interrogate the reasons for the high emergency intervention rate, it is possible that this may be related to delayed presentation to our specialist centre due to healthcare-seeking behaviour, as well as the limited access to specialist centres that are remote from their place of domicile.
Prosthetic valve thrombosis was seen in 72.5% of the valve procedures. A similar observation has been made by other studies from Africa and other LMICs which quote prosthetic valve thrombosis at 65-94%.7,16 These figures are much higher than those seen in HICs where prosthetic valve thrombosis is the least common indication for redo MVR, ranging between 0-12%.615 Counter-intuitively the prosthetic thrombosis rate tended to be higher in HIVnegative patients than HIV-positive patients. This finding merits further study as does the overall effect of HIV infection on mechanical valve dysfunction.
The aetiopathogenesis of prosthetic valve thrombosis is based on several mechanisms, including molecular interaction between corpuscular blood components and prosthetic surfaces, the effect of the trans-prosthetic blood flow on local thrombus formation, ineffective anticoagulation and the presence of any other pro-thrombotic factors.27
In addition, the prevalence of atrial fibrillation is significantly higher in patients with RHD when compared to age-matched general population, which in turn increases the risk of thromboembolism and heart failure.28 In LMICs a number of factors have been found to be significantly associated with poor compliance and sub-optimal control of INR, including educational level, and restricted access to medication and healthcare facilities.29 The assessment of warfarin compliance was not objective as it was based on a once-off INR reading at the time of visit to our unit and does not evaluate monitoring at the base hospital.
Therapeutic anticoagulation is a key component of preventing valve thrombosis. Internationally, there is a robust debate regarding specific INR targets in contrast to the one-size-fits-all INR therapeutic range of 2-4.11,30 Monitoring and tight control of anticoagulation treatment reduce the risk of both thrombosis and bleeding,30 and the use of point-of-care coagulation monitors may be helpful in this regard.31 The clinical benefit and risks of warfarin are associated with the proportion of time that INR values are between 2 and 3, meaning the time in therapeutic range (TTR).30 TTR is an important tool to assess the quality of the anticoagulation treatment once satisfactory anticoagulation is obtained postsurgery.30 The use of TTR was not evaluated in this study. However, a more complete evaluation of INR control using the TTR is the subject of prospective study in our department.
A redo MVR is a high-risk operation, but in carefully selected patients with optimal timing of surgery, it can be performed with acceptable results.3,21 This study had a mortality rate of 3.1% which falls within the 3-20.3% reported in the international literature.7,11-18,22 Our follow-up of 42 months is much lower than the 124 months reported by others,17 which highlights the problem of follow-up in LMICs like South Africa.
Conclusion
Despite the limitations of this retrospective cohort, it does serve as comparator and benchmark for future MVR redo studies in LMIC. Mortality and morbidity rates following surgery were excellent when compared to worldwide data. Notably, this study highlights the high frequency of thrombosis and the emergency redo MVR as targets for quality improvement in a very young RHD cohort with mitral valve disease. We recognise that rheumatic fever and RHD should be made notifiable as a measure to ensure control of the disease through prophylaxis programmes.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Ethical approval was obtained from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (Reference: BE442/15).
ORCID
M Booysen https://orcid.org/0000-0002-9889-5839
G Alexander https://orcid.org/0000-0002-8287-3467
TE Madiba https://orcid.org/0000-0002-0155-9143
REFERENCES
1. Seckeler MD, Hoke TR. The worldwide epidemiology of acute rheumatic fever and rheumatic heart disease. Clin Epidemiol. 2011;3:67-84. https://doi.org/10.2147/CLEP.S12977. [ Links ]
2. Carapetis JR. Rheumatic heart disease in developing countries. N Engl J Med. 2007;357(5):439-41. https://doi.org/10.1056/NEJMp078039. [ Links ]
3. Essop MR, Nkomo VT. Rheumatic and nonrheumatic valvular heart disease - epidemiology, management, and prevention in Africa. Circulation. 2005;112(23):3584-91. https://doi.org/10.1161/CIRCULATIONAHA.105.539775. [ Links ]
4. Soler-Soler J, Galve E. Worldwide perspective of valve disease. Heart. 2000;83(6):721-5. https://doi.org/10.1136/heart.83.6.721. [ Links ]
5. Zuhlke LJ, Steer AC. Estimates of the global burden of rheumatic heart disease. Glob Heart. 2013;8(3):189-95. https://doi.org/10.1016/j.gheart.2013.08.008. [ Links ]
6. Suri RM, Schaff HV. Reoperation following mitral valve repair. In Redo - Cardiac Surgery in Adults. Springer: New York; 2013. p. 89-97. https://doi.org/10.1007/978-1-4614-1326-4_11. [ Links ]
7. Vohra HA, Whistance RN, Roubelakis A, et al. Outcome after redo-mitral valve replacement in adult patients - a 10-year single-centre experience. Interact Cardiovasc Thor Surg. 2012;14(5):575-9. https://doi.org/10.1093/icvts/ivs005. [ Links ]
8. Kothari J, Patel K, Brahmbhatt B, et al. Redo mitral valve replacement for prosthetic valve thrombosis - single center experience. J Clin Diagnostic Res. 2016;10(11):PC01-3. https://doi.org/10.7860/JCDR/2016/20209.8913. [ Links ]
9. Nkomo VT. Epidemiology and prevention of valvular heart diseases and infective endocarditis in Africa. Heart. 2007;93(12):1510-9. https://doi.org/10.1136/hrt.2007.118810. [ Links ]
10. Moss RR, Humphries KH, Gao M, et al. Outcome of mitral valve repair or replacement - a comparison by propensity score analysis. Circulation. 2003;108(Suppl 1):II90-7. https://doi.org/10.1161/01.cir.0000089182.44963.bb. [ Links ]
11. Van Doorn C, Yates R, Tsang V, deLeval M, Elliott M. Mitral valve replacement in children - mortality, morbidity, and haemodynamic status up to medium term follow up. Heart. 2000;84(6):636-42. https://doi.org/10.1136/heart.84.6.636. [ Links ]
12. Beierlein W, Becker V, Yates R, et al. Long-term follow-up after mitral valve replacement in childhood - poor eventfree survival in the young child. Eur J Cardiothorac Surg. 2007;31(5):860-5. https://doi.org/10.1016/j.ejcts.2007.02.006. [ Links ]
13. Colkesen Y, Coskun I, Cayli M, Gulcan O. Predictors of in hospital mortality following redo cardiac surgery - single center experience. Interv Med Appl Sci. 2015;7(3):102-7. https://doi.org/10.1556/1646.7.2015.3.3. [ Links ]
14. Maganti M, Rao V, Armstrong S, et al. Redo valvular surgery in elderly patients. Ann Thorac Surg. 2009;87(2):521-5. https://doi.org/10.1016/j.athoracsur.2008.09.030. [ Links ]
15. Fouda T, Gado A, Abul-dahab M, Fathy H. Predictors of morbidity and mortality in redo mitral valve replacement for prosthetic mechanical mitral valve dysfunction. J Egypt Soc Cardiothor Surg. 2014;22:81-92. [ Links ]
16. Matsuyama K, Matsumoto M, Sugita T, et al. Long-term results of reoperative mitral valve surgery in patients with rheumatic disease. Ann Thorac Surg. 2003;76(6):1939-43. https://doi.org/10.1016/S0003-4975(03)01061-0. [ Links ]
17. Kumar AS, Dhareshwar J, Airan B, et al. Redo mitral valve surgery-a long-term experience. J Card Surg. 2004;19(4):303-7. https://doi.org/10.1111/j.0886-0440.2004.4054_11.x. [ Links ]
18. Yau TM, El-Ghoneimi YAF, Armstrong S, Ivanov J, David TE. Mitral valve repair and replacement for rheumatic disease. J Thorac Cardiovasc Surg. 2000;119(1):53-60. https://doi.org/10.1016/S0022-5223(00)70217-0. [ Links ]
19. Zûhlke L, Mirabel M, Marijon E. Congenital heart disease and rheumatic heart disease in Africa - recent advances and current priorities. Heart. 2013;99(21):1554-61. https://doi.org/10.1136/heartjnl-2013-303896. [ Links ]
20. Sliwa K, Carrington M, Mayosi BM, et al. Incidence and characteristics of newly diagnosed rheumatic heart disease in urban African adults - insights from the heart of Soweto study. Eur Heart J. 2010;31(6):719-27. https://doi.org/10.1093/eurheartj/ehp530. [ Links ]
21. Ejiofor JI, Hirji SA, Ramirez-Del Val F, et al. Outcomes of repeat mitral valve replacement in patients with prior mitral surgery - a benchmark for transcatheter approaches. J Thorac Cardiovasc Surg. 2018;156(2):619-627.e1. https://doi.org/10.1016/j.jtcvs.2018.03.126. [ Links ]
22. Dokhan AL, Taher AH, Ibrahim IM, Asfour AM. The short-term outcome of redo-mitral valve surgery - emergency versus elective. Menoufia Med J. 2016;29(3):668-73. https://doi.org/10.4103/1110-2098.198752. [ Links ]
23. Ruel M, Kulik A, Lam BK, et al. Long-term outcomes of valve replacement with modern prostheses in young adults. Eur J Cardiothorac Surg. 2005;27(3):425-33. https://doi.org/10.1016/j.ejcts.2004.12.002. [ Links ]
24. Chikwe J, Chiang YP, Egorova NN, Itagaki S, Adams DH. Survival and outcomes following bioprosthetic vs mechanical mitral valve replacement in patients aged 50 to 69 years. JAMA. 2015;313(14):1435-42. https://doi.org/10.1001/jama.2015.3164. [ Links ]
25. Rahimtoola SH. Choice of prosthetic heart valve in adults an update. J Am Coll Cardiol. 2010;55(22):2413-26. https://doi.org/10.1016/j.jacc.2009.10.085. [ Links ]
26. Lazam S, Vanoverschelde JL, Tribouilloy C, et al. Twenty-year outcome after mitral repair versus replacement for severe degenerative mitral regurgitation - analysis of a large, prospective, multicenter, international registry. Circulation.2017;135(5):410-22. [ Links ]
27. Gûrsoy MO, Kalçik M, Yesin M, et al. A global perspective on mechanical prosthetic heart valve thrombosis - diagnostic and therapeutic challenges. Anatol J Cardiol. 2016;16(12):980-9. [ Links ]
28. Negi PC, Sondhi S, Rana V, et al. Prevalence, risk determinants and consequences of atrial fibrillation in rheumatic heart disease - 6 years hospital based-Himachal Pradesh- Rheumatic Fever/Rheumatic Heart Disease (HP-RF/ RHD) Registry. Indian Heart J. 2018;70(Suppl 3):S68-73. https://doi.org/10.1016/j.ihj.2018.05.013. [ Links ]
29. Chalachew T, Yadeta D, Tefera E. Factors associated with suboptimal control of anticoagulation in patients with prosthetic heart valves taking oral anticoagulants in a sub-Saharan African setting. Cardiovasc J Afr. 2019;30(6):1-5. https://doi.org/10.5830/CVJA-2019-024. [ Links ]
30. Wieloch M, Sjalander A, Frykman V, et al. Anticoagulation control in Sweden - reports of time in therapeutic range, major bleeding, and thrombo-embolic complications from the national quality registry AuriculA. Eur Heart J. 2011;32(18):2282-9. https://doi.org/10.1093/eurheartj/ehr134. [ Links ]
31. Sharma P, Scotland G, Cruickshank M, et al. The clinical effectiveness and cost-effectiveness of point-of-care tests (CoaguChek system, INRatio2 PT/INR monitor and ProTime Microcoagulation system) for the self-monitoring of the coagulation status of people receiving long-term vitamin K antagonist therapy, compared with standard UK practice -systematic review and economic evaluation. Health Technol Assess. 2015;19(48):1-172. https://doi.org/10.3310/hta19480. [ Links ]
 Correspondence:
Correspondence:
TE Madiba
Email: madiba@ukzn.ac.za














