Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.59 n.4 Cape Town Dec. 2021
http://dx.doi.org/10.17159/2078-5151/2021/v59n4a5321
HOW TO DO IT
Balloon tube tamponade for variceal bleeding: ten rules for safe usage
JEJ Krige; L Perold; EG Jonas
Surgical Gastroenterology and HPB Unit, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, South Africa
Keywords: oesophageal variceal bleeding, Sengstaken-Blakemore tube, balloon tamponade
Acute gastro-oesophageal variceal bleeding can be controlled in most patients by a correctly placed Sengstaken-Blakemore or Minnesota balloon tube if endoscopic intervention fails or the necessary expertise is not immediately available.1 The temporary control of bleeding by balloon tamponade allows time for resuscitation and correction of clotting defects which should be done promptly to limit the duration of balloon tube compression, ideally within 24 hours. As 60% of patients will re-bleed after balloon deflation without further intervention, an experienced endoscopist must be available when the tube is removed. Although newer methods including self-expanding oesophageal stents can be used for bleeding control, balloon tamponade remains the most widely available technique for immediate control, especially in smaller hospitals.2
The original balloon tube devised by Sengstaken and Blakemore had two balloons, three lumens, one for gastric aspiration and two with ports to inflate the balloons. Both the Minnesota and the Boyce modification of the Sengstaken-Blakemore tube have an additional fourth lumen which has holes placed above the oesophageal balloon which allow drainage of accumulated saliva to prevent aspiration (Figure 1). If incorrectly inserted and positioned, serious and life-threatening tube-related complications may occur.3 Several critical sequential steps must be followed to ensure safe balloon tube placement to avoid potential complications and to provide effective bleeding control.4

1. A new balloon tube should be used on each occasion and the integrity of both balloons tested before use by inflation under water to confirm that no air leaks are present.
2. Airway protection is crucial. Before a balloon tube is inserted in a stuporous or encephalopathic patient, the airway must be protected by placing an endotracheal tube to prevent aspiration. Following airway intubation, the patient should be nursed in the supine position with the head of the bed elevated to 45 degrees.
3. After adequate topical pharyngeal anaesthesia, a lubricated and fully deflated balloon tube is inserted orally through a mouth bite-guard placed between the teeth using a technique similar to orogastric tube placement. Awake patients are instructed to swallow to facilitate tube passage as the tube is advanced over the tongue.
In a stuporous patient, placing the index finger in the mouth assists in guiding the tip of the tube over the posterior tongue and through the cricopharyngeus sphincter to prevent coiling of the tube in the pharynx. If there is difficulty in passing the tube, especially when an endotracheal tube is in place, the tube should be passed under direct vision using a McGill's forceps and laryngoscope. The tube is advanced as far as the junction of the access ports.
4. Before inflation, the correct position of the balloon in the stomach must be confirmed by an upper abdominal X-ray showing a straight tube in the oesophagus with the lower end of the tube coiled in the stomach. This is a crucial step that must not be omitted. An alternative method is to pass an endoscope alongside the inserted tube to confirm the correct position of the gastric balloon in the stomach and then to observe inflation of the balloon under direct vision before removing the endoscope. Recommendations of injecting air into the aspirating lumen of the gastric tube and auscultating over the epigastrium or using ultrasound confirmation are unreliable and should not be used.
5. The gastric balloon is carefully inflated with 50 ml increments of air until a total of 250 ml has been inserted. The air should be easy to inject; if the tube is kinked or curled in the oesophagus, resistance to injection is felt and inflation must stop and the balloon deflated. An incorrectly positioned inflated gastric balloon may rupture the oesophagus.5
6. Once inflated, the tube is pulled back until resistance is felt indicating that the inflated gastric balloon is lodged firmly against the oesophagogastric junction, thereby interrupting variceal inflow. The depth of the tube is marked at the bite guard level and must be checked regularly. While the tube may stretch slightly as it warms to body temperature, lengthening of more than 3 cm may indicate a hiatus hernia or balloon migration into the oesophagus. This should prompt re-evaluation of the balloon position with a repeat X-ray.
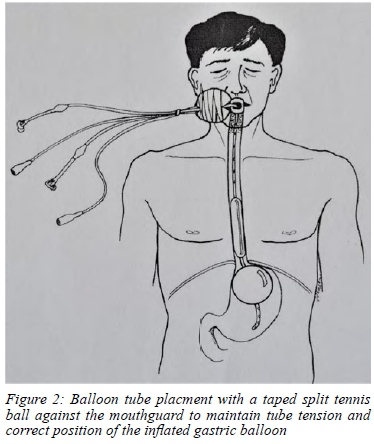
7. The correctly positioned tube is held in place using a split tennis ball strapped to the tube adjacent to the mouth guard with Elastoplast® (Figure 2). The oesophageal portion of the tube is thereby kept taut between the gastric balloon below and the tennis ball above. This method is effective in maintaining balloon tamponade at the oesophagogastric junction.
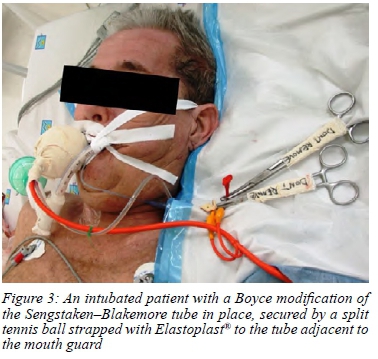
8. Effectively maintained tension on the gastric balloon should be checked regularly at the mouth with the tennis ball snugly opposed to the mouth guard which prevents pressure injury to the patient's lips (Figure 3).
9. Whereas inflow control by the lodged gastric balloon usually controls variceal bleeding, direct longitudinal compression by inflating the oesophageal balloon may be required in some patients. A three-way tap and a blood pressure manometer are used to inflate the oesophageal balloon to 40 mm Hg. The tube port is then clamped, and the pressure checked regularly.
10. The oesophageal and gastric drainage lumens of the balloon tube are placed on free drainage with intermittent flushing to avoid blockage and subsequent aspiration of saliva and blood. The gastric lumen is also used for administering medication, such as lactulose to reduce encephalopathy. Patients with a balloon tube in place should ideally be admitted to an intensive care unit for optimal monitoring and tube management.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
ORCID
JEJ Krige https://orcid.org/0000-0002-7057-9156
L Perold https://orcid.org/0000-0002-3697-5008
EG Jonas https://orcid.org/0000-0003-0123-256X
REFERENCES
1. Sengstaken RW, Blakemore AH. Balloon tamponade for the control of haemorrhage from oesophageal varices. Ann Surg. 1950;131:781-9. https://doi.org/10.1097/00000658-195005000-00017. [ Links ]
2. Rodrigues SG, Cárdenas A, Escorsell À, Bosch J. Balloon tamponade and oesophageal stenting for oesophageal variceal bleeding in cirrhosis - a systematic review and meta-analysis. Semin Liver Dis. 2019;39:178-94. https://doi.org/10.1055/s-0039-1678726. [ Links ]
3. Nielsen TS, Charles AV. Lethal oesophageal rupture following treatment with Sengstaken-Blakemore tube in management of variceal bleeding - a 10-year autopsy study. Forensic Sci Int. 2012;222(1-3):e19-22. https://doi.org/10.1016/j.forsciint.2012.05.024. [ Links ]
4. Krige JEJ, Thomson SR. Endoscopic therapy in the management of oesophageal and gastric varices. In: Nyhus, Baker, Fischer, editors. Mastery of Surgery. 7th ed. Wolters Kluwer: Philadelphia; 2019. [ Links ]
5. Krige JEJ, Bornman PC. Endoscopic therapy in the management of oesophageal varices - injection sclerotherapy and variceal ligation. In: Blumgart L, editor. Surgery of the Liver, Biliary Tract and Pancreas. 4th ed. Saunders, Elsevier: Philadelphia; 2007. p. 1579-93. https://doi.org/10.1016/B978-1-4160-3256-4.50112-5. [ Links ]
 Correspondence:
Correspondence:
JEJ Krige
Email: jej.krige@uct.ac.za














