Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.59 no.3 Cape Town sep. 2021
http://dx.doi.org/10.17159/2078-5151/2021/v59n3a3544
CASE REPORT
Biliary tract anatomical variance - the value of MRCP
C FerreiraI; CB NoelII
IDepartment of Surgery, Faculty of Health Sciences, University of the Free State, South Africa
IIDepartment of General and Hepatopancreaticobiliary Surgery, Universitas Academic Hospital, South Africa
SUMMARY
Duplication of the common bile duct (CBD) is a rare congenital anomaly of the bile ducts that should be diagnosed prior to surgery in order to optimise management and prevent complications. We report a case of a patient presenting with choledocholithiasis and type Va duplicated extrahepatic bile duct that was missed on ultrasonography. The atypical course prompted further imaging with magnetic resonance cholangiopancreatography (MRCP), which identified the aberrant bile duct and assisted in safe preoperative and operative management. This case highlights the importance of accurate pre-interventional imaging and agrees with the reclassification of duplications of the CBD.
Keywords: bile duct, extrahepatic, anomaly, duplicated, injury
Presentation of case
A 35-year-old woman was referred from her base hospital to the specialist healthcare facility with ultrasonographic evidence of choledocholithiasis and a background history of obstructive jaundice, which had resolved. She presented to her base hospital complaining of a three-month history of fluctuating obstructive jaundice, right upper quadrant pain radiating to the back, vomiting and epigastric pain. An abdominal examination revealed a non-distended soft abdomen with mild right upper quadrant pain, epigastric tenderness and a negative Murphy's sign.
The patient's index liver biochemistry was in keeping with cholestasis, total bilirubin (222 mmol/L), conjugated bilirubin (120 mmol/L), alanine and aspartate transaminases (505 U/L and 218 U/L, respectively), alkaline phosphatase (414 U/L) and gamma-glutamyl transferase (1 498 U/L). Her white cell count was 10.50 x 109/L.
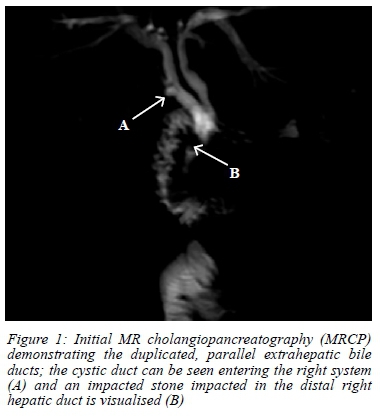
Ultrasonography (U/S) revealed both intra- and extra-hepatic bile duct dilation, a distal common bile duct (CBD) measuring 9 mm and a stone in the distal CBD measuring 10 mm in diameter. Appropriate antibiotics were initiated while awaiting transfer to the specialist healthcare facility where, on arrival, there was persistence of her right upper quadrant pain but complete clinical and biochemical resolution of the patient's cholestasis. In view of the suspected choledocholithiasis, and atypical clinical course, magnetic resonance cholangiopancreatography (MRCP) was performed, which revealed aberrant bile duct anatomy showing a parallel extrahepatic right and left ductal system with a retroduodenal confluence. A single stone impacted in the distal part of the right hepatic duct just proximal to the hepatic duct confluence was noted. The cystic duct entered on the right system (Figure 1). Multiple stones were visualised in the gallbladder, with no signs of acute cholecystitis.
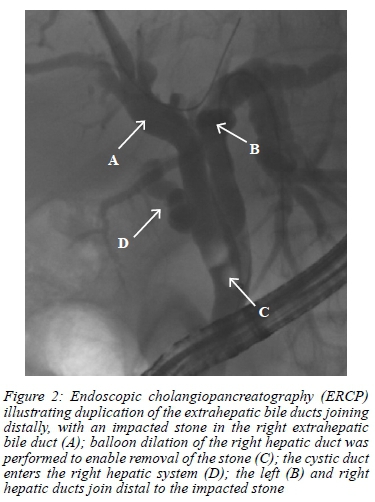
At endoscopic retrograde cholangiopancreatography (ERCP), a sphincterotomy and balloon dilation of the right hepatic duct and distal CBD to 15 mm was performed after which a stone was extracted (Figure 2). A final diagnosis of cholecystolithiasis and choledocholithiasis was made and the patient underwent a laparoscopic cholecystectomy.
Intraoperatively, the low inserting cystic duct was in close approximation to the right hepatic duct with a parallel course at insertion. Normal inferolateral traction on the infundibulum resulted in limited displacement from the right hepatic duct and preoperative MRCP imaging assisted the surgeons in safe dissection. The critical view of safety was achieved intraoperatively, the cystic duct was clipped and divided, and a cholecystectomy was performed. Postoperative recovery was unremarkable.
Discussion
The duplication of the CBD is a rare abnormal anatomical variation of the bile duct. Initially, four types of bile duct variants had been reported until Choi et al.1 described an additional fifth type. Identification of these anatomical variations during U/S can be missed and more accurate imaging with MRCP serves as a vital aspect in the prevention and risk of injury during surgeries, such as laparoscopic cholecystectomy.
Development of the liver and biliary tree occurs at three phases, namely embryonic development, foetal and postnatal growth.2 Anatomical variations in the extrahepatic bile duct, including duplication of the bile duct, are consistent with the embryonic development phase, possibly due to the random subdivision of the hepatic diverticulum during embryogenesis.2
Pancreaticobiliary anomalies are associated with an increased prevalence of biliary pathology.3 In addition, identification of such variations is of clinical importance to surgeons in order to prevent injury during surgery. The most common cause (~95%) of serious biliary injury is thought to be as a result of misidentification of structures.4
This case highlights three important areas. The first is that an atypical clinical course or incongruent clinical and biochemical course should alert the clinician to the possibility of an anatomical aberrancy or complication and should prompt further imaging. With "normal" bile duct anatomy only present in ~50% of the general population, the value of accurate imaging of the biliary tree prior to surgery is important.5
Secondly, this case highlights the value of an MRCP and potential limitation of U/S in cases with bile duct aberrancies. A study by Singh et al.6 aimed at comparing the diagnostic accuracy of MRCP with trans abdominal U/S and computed tomography (CT) in patients with obstructive jaundice. It was found that the overall sensitivity and specificity in diagnosing choledocholithiasis was greater in MRCP (95.83-100%) when compared to that of U/S (79.17-95.83%). Prusty et al.7 reported similar findings in the setting of benign biliary pathology, with transabdominal U/S reporting a sensitivity and specificity of 84% and 100%, while MRCP being 96.55% and 100%, respectively. In the presented case, the anatomical variant was missed on U/S. The atypical clinical course prompted the MRCP that accurately identified the aberrant anatomy which further facilitated both the ERCP and more importantly the laparoscopic cholecystectomy.
Lastly, we agree with Choi et al.1 regarding reclassification of double bile duct configurations. Saito et al.8 proposed the following four double common bile duct (DCBD) configurations: type I, CBD with a septum dividing the bile duct lumen; type II, CBD that distally bifurcates to drain independently; type III, double biliary drainage without extrahepatic communication. Type III is further subdivided into (IIIa) without or (IIIb) with intrahepatic communication; and type IV, double biliary duct drainage with one or more extrahepatic communication channels. Choi et al.1 later proposed an additional double extrahepatic bile duct configuration to the list, namely type V, single biliary drainage of double extrahepatic bile ducts (Va) without (Vb) or with communication channels.
In this case, the patient presented with a type Va double extrahepatic bile duct.1 The ducts were presented parallel to one another before joining distally retropancreatic. A complete absence of the common hepatic duct was noted, as the cystic duct drained only into the right hepatic duct, with no proximal communication. In this case, there was no duplication of the CBD but rather a parallel extrahepatic right and left hepatic duct with a very short single CBD. This double extrahepatic bile duct could explain the atypical clinical presentation and improvement in liver biochemistry, as bile was still able to drain from the Couinaud hepatic segments II-IV. Spontaneous intermittent dis-impaction of the stone, although possible, was less likely, as it would not have accounted for the normalisation of the liver biochemistry at the same time as the ERCP where the stone was found to be impacted in the right hepatic duct when a balloon occluded cholangiogram was performed.
In conclusion, preoperative identification of bile duct aberrancies is essential to clinicians for both effective and safe treatment. Here, we illustrate the effectiveness of performing an MRCP as a non-invasive imaging tool in the case of a parallel extrahepatic bile duct anomaly and propose a low threshold for the use of MRCP pre-intervention in cases with atypical clinical courses or liver biochemistry.
Acknowledgements
The authors would like to acknowledge Professor R Barry and Dr M Pungutche, Department of Surgery, for their contribution; and Dr D Struwig, medical writer/editor, Faculty of Health Sciences, University of the Free State, for technical and editorial preparation of the manuscript.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Ethical approval to report this case was obtained from the Health Sciences Research Ethics Committee (HSREC) of the Faculty of Health Sciences, University of the Free State (ethical clearance number UFS-HSD-2020/0016/2909). Permission was granted by the Head of the Department of Surgery and the Free State Department of Health. Written informed consent to report the case was obtained from the patient.
ORCID
C Ferreira https://orcid.org/0000-0002-7386-0752
CB Noel https://orcid.org/0000-0003-2344-415X
REFERENCES
1. Choi E, Byun JH, Park BJ, Lee M-G. Duplication of the extrahepatic bile duct with anomalous union of the pancreaticobiliary ductal system revealed by MR cholangiopancreatography. Br J Radiol. 2007;80(955):e150-54. https://doi.org/10.1259/bjr/50929809. [ Links ]
2. Knisely AS. Biliary tract malformations. Am J Med Genet. 2003;122A(4):343-50. https://doi.org/10.1002/ajmg.a.20479. [ Links ]
3. Rizzo RJ, Szucs RA, Turner MA. Congenital abnormalities of the pancreas and biliary tree in adults. Radiographics. 1995;15(1):49-68. https://doi.org/10.1148/radiographics.15.1.7899613. [ Links ]
4. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180(1):101-25. [ Links ]
5. Khayat MF, Al-Ammodi MS, Aldaqal SM, Sibiany A. Abnormal anatomical variations of extra-hepatic biliary tract, and their relation to biliary tract injuries and stones formation. Gastroenterol Res. 2014;7(1):12-6. https://doi.org/10.14740/gr596e. [ Links ]
6. Singh A, Mann HS, Thukral CL, Singh NR. Diagnostic accuracy of MRCP as compared to ultrasound/CT in patients with obstructive jaundice. J Clin Diagn Res. 2014;8(3):103-7. https://doi.org/10.7860/JCDR/2014/8149.4120. [ Links ]
7. Prusty SK, Bhagat S, Panda BB. Ultrasonography vs MRCP in evaluation of obstructive jaundice. J Med Sci Clin Res. 2019;7(1):1120-8. https://doi.org/10.18535/jmscr/v7i1.197. [ Links ]
8. Saito N, Nakano A, Arase M, Hiraoka T. [A case of duplication of the common bile duct with anomaly of the intrahepatic bile duct] [Article in Japanese]. Nihon Geka Gakkai Zasshi. 1988;89(8):1296-301. [ Links ]
 Correspondence:
Correspondence:
C Ferreira
Email: ferreirac4@ufs.ac.za














