Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.59 n.3 Cape Town Sep. 2021
http://dx.doi.org/10.17159/2078-5151/2021/v59n3a3477
BREAST DISEASE
An audit of patients presenting with clinically benign breast disease to the Helen Joseph Hospital Breast Imaging Unit
NC ChristofidesI; G RubinII; C-A BeimIII
IDepartment of Diagnostic Radiology, University of the Witwatersrand, South Africa
IIDepartment of Radiology, Helen Joseph Hospital, South Africa
IIIBreast Surgical Unit, Helen Joseph Hospital, South Africa
ABSTRACT
BACKGROUND: Benign breast pathology is a common presenting complaint, and its assessment is important to characterise not to miss malignant pathology. At Helen Joseph Hospital (HJH), patients are triaged at the breast clinic according to the clinical suspicion of benign versus malignant disease. The patients are assigned a colour label based on their clinical presentation. This triage system affects waiting times between clinical examination and mammography appointments. This study aims to assess the association between clinical examination and the radiological and pathological findings of disorders deemed clinically benign, and to ascertain the spectrum of benign breast disorders encountered at HJH
METHOD: A retrospective study of imaging results of patients at HJH presenting as clinically benign breast disorders from January to June 2018 was conducted. Assessed Breast Imaging-Reporting and Data System (BI-RADS) score was noted and if core biopsies were performed, their results and patient demographics were documented
RESULTS: Of the 1 263 clinically benign patients presenting from January to June 2018, the radiological assessment was: BI-RADS 1: 158 (12.5%), BI-RADS 2: 685 (54.2%), BI-RADS 3: 292 (23.1%), BI-RADS 4a: 54 (4.3%), BI-RADS 4b: 29 (2.3 %), BI-RADS 4c: 21 (1.7%), BI-RADS 5: 24 (1.9%). There were 133 biopsies (including eight BI-RADS 3 patients), with 46 (3.6%) confirmed malignancies. The combined specificity of mammography and ultrasound was 65.52% (54.56-75.39%) and combined sensitivity 91.30% (79.21-97.58%
CONCLUSION: There is a vast spectrum of benign conditions presenting in this population group with only 3.6% confirmed malignancies, confirming an accurate triage system utilised at the breast clinic. Radiological imaging is highly sensitive but less specific, emphasising the triad of clinical, radiological and histological assessment as the gold standard with regard to diagnosis of breast disease
Keywords: clinically benign breast disease, breast imaging unit, Helen Joseph Hospital
Introduction
Benign breast pathology is a common presenting complaint, with benign diseases more common than malignancies in young women.1 In North America, benign breast disorders account for 90% of breast complaints presenting to hospitals.2 The majority of patients presenting with breast complaints are found to have benign breast disorders, as seen in both developing and developed countries.1,3 Benign breast disorders have various modes of presentation and comprise multiple entities.4 These disorders require adequate diagnosis and monitoring to identify a mis-assessment of malignant pathology and to review for the small increased risk of breast cancer development associated with some benign pathology.5 Benign breast disease, such as phyllodes tumour, can carry an increased risk of progression to malignant phyllodes tumours.5
In order to correctly diagnose these conditions, triple assessment is utilised with the radiological correlation forming an integral part of benign breast disorder diagnosis and monitoring.6 Since breast cancer is the most common cancer in female patients, the diagnosis of a benign breast disorder is a relief to most patients.7,8 It is therefore important to classify the percentage of patients presenting with these conditions and to ascertain the spectrum of benign disorders seen in our community. Triple (clinical, radiological and pathological) assessment is the gold standard in order to achieve a definitive diagnosis.6
Breast Imaging-Reporting and Data System (BI-RADS) is the radiological classification system used for breast imaging to help standardise breast imaging reporting.9 It is also useful in aiding adequate communication of findings to both radiologists and clinicians alike, as well as providing a method to monitor outcomes of patients.9 The BI-RADS classification system and the risk of malignancy is noted in Table I.
At the Helen Joseph Hospital (HJH), patients are triaged at the breast clinic according to a clinical suspicion of benign versus malignant breast disease. The patients are assigned a colour label based on their clinical presentation. Patients who present with a clinical suspicion of an abscess, or high suspicion for cancer are triaged as red (deemed high risk clinically and requiring imaging as soon as possible). Those who present with breast pain or breast asymmetry but with no mass, or any non-suspicious mass, milky/infected nipple discharge, or palpable axillary lymph nodes with no definite palpable breast pathology are triaged as yellow. This triage system affects waiting times between clinical examination and mammography appointments. An assessment was performed of patients triaged as yellow (clinically benign) who received a date for their imaging studies within 6-8 weeks of their clinical examination. Thus, the sensitivity of our triage system as well as radiological and histological correlation is vital to patient management.
This study aims to assess the association between clinical examination and the radiological and pathological findings of disorders deemed clinically benign and to ascertain the spectrum of benign breast disorders encountered at HJH.
Methods
This was a retrospective study of mammographic, sono-graphic and histological (where available) results of all patients group (irrespective of age or gender) presenting to HJH breast unit with clinically benign breast disorders from January to June 2018. This included all patients who were classified as benign by the HJH breast unit, based on certain clinical features: breast pain, breast asymmetry, milky or yellow nipple discharge, possibility of palpable lymph nodes with nothing palpable in the breast, palpable mass with no suspicion for cancer. All reports that were illegible or lost were excluded.
The mammogram and ultrasound reports were collected and from them, BI-RADS scores, core biopsy reports and the demographics were collated on a data sheet.
The frequency of all BI-RADS classifications found was calculated.
All patients who received a biopsy were documented and the results correlated with their clinical and imaging results. Histology results were accessed from the National Health Laboratory Service (NHLS) for all patients who underwent a biopsy. An anonymised database (on Excel) based on demographics, BI-RADS score and histology results was collected and documented.
The study is reliable as it is an audit on the department, based on the radiological reports in a unit with a dedicated breast imaging specialist and thus is repeatable.
The study is valid as all lesions classified as BI-RADS > 4 receive biopsies (gold standard as per BI-RADS) and thus the diagnoses had histological correlation.
Descriptive statics (percentages and frequencies) were calculated for categorical data.
Pearson's chi-squared test to determine the association between radiological and histological findings was performed. The sensitivity and specificity were calculated. Prior to the commencement of this study, ethical clearance was obtained; certificate number M191172.
Results
There were a total of 1 263 patients with a wide variety of ages, and 34 male and 1 229 female patients. Table II demonstrates the demographics of the patients included in the study.
In Figure 1, the percentage of patients per age group within each of the BI-RADS categories is shown.
Of the clinically benign patients presenting from January to June 2018 the spectrum of imaging findings was as follows:
BI-RADS 1: 158 (12.5%), BI-RADS 2: 685 (54.2%), BI-RADS 3: 292 (23.1%), BI-RADS 4a: 54 (4.3%), BI-RADS 4b: 29 (2.3 %), BI-RADS 4c: 21 (1.7%), BI-RADS 5: 24 (1.9%).
In Table III, the BI-RADS category of every patient who underwent biopsy is recorded and their results are supplied. These results are expressed as a percentage of the total sample number, with only 3.6% of all patients classified as clinically benign representing malignant disease.
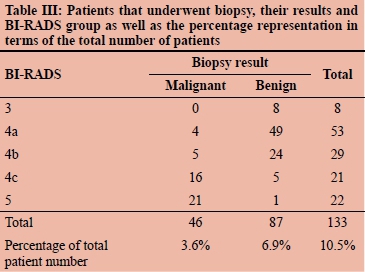
The eight BI-RADS 3 patients who underwent biopsy were to either confirm diagnosis, such as in the case of a giant fibroadenoma or at the request of the patient and all eight were confirmed histologically to be benign.
There were also three patients within the BI-RADS 4 and 5 categories who did not undergo biopsy. The reasons were multifocal: patient refusal, patient too unstable or clinically unwell to undergo biopsy or no stock of biopsy needles (these patients were subsequently rebooked).
An assessment of all biopsies was performed, their results and the patients' distribution among the BI-RADS categories (Table III) documented. From these results, a chi-squared value of 77.307 with a _p-value of < 0.00001 was obtained. This indicates a statistically significant correlation between the radiological findings and the corresponding histological results.
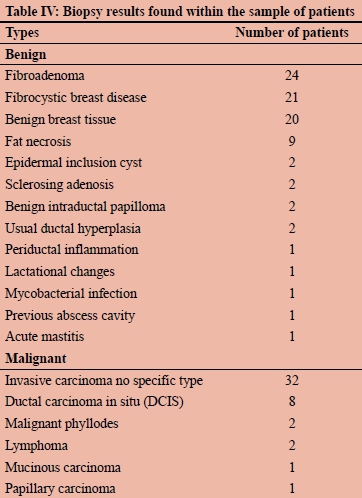
Table IV depicts the spectrum of disease found amongst all the study participants that underwent biopsy. The majority of the patients depicted displayed benign histology in keeping with the clinical findings.
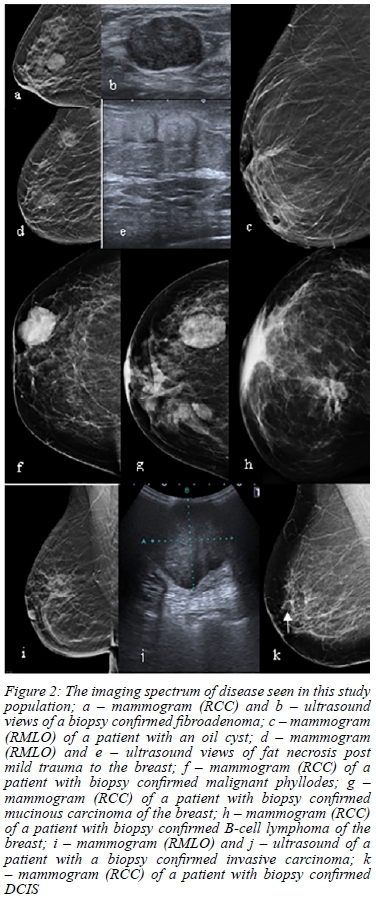
The imaging spectrum of disease within the study population is illustrated in Figure 2.
Discussion
Our results demonstrate a wide distribution of ages amongst all the clinically benign patients presenting at an open access breast clinic. The majority of patients were between the ages of 40 and 70, however, in more developed countries, most patients presenting with benign breast diseases are between the ages of 30 and 50 years.11 This may be related to better access to health care and earlier detection in these more developed countries.
Most of the patients within this clinically benign population fell within the benign or probably benign BI-RADS categories with 1 135 (89.9%) out of a total of 1 263 between BI-RADS 1, 2 and 3. This is in keeping with the literature as clinical examination alone has a sensitivity of 54%, while its specificity is 94%, and as such, some suspicious lesions may be mis-diagnosed as benign pathology.12
There were 128 (10.1%) patients within this clinically benign group who were radiologically suspicious (BIRADS 4-5). This is higher than expected as per the literature. After a single step triage system (as in our case), 52% of patients with malignancies were given non-urgent dates. Subsequently, after a second stage triage, only 4% of patients with malignancies were given non-urgent dates.13
A total of 133 biopsies were performed (some performed on BI-RADS 3 patients for confirmation of diagnosis or at the patient's request). Three of the radiologically suspicious patients did not undergo biopsy due to refusal, inadequate clinical status, or lack of stock of biopsy needles.
Of the 133 patients who underwent biopsies, only 46 were confirmed to have malignancies, representing 3.6% of the total sample (1 263) patients. This is comparable with international triage systems as it is expected that 4% of patients with breast cancer will be triaged as semi-urgent (or yellow labelled as in our case).13
This emphasises that clinical examination is a good screening modality, but cannot be used as a stand-alone investigation in our country or globally.12
From Table IV, one can see that the majority of malignancies were found to be invasive carcinoma of no specific type (69.6% of all malignancies found) with the next most common malignancy being ductal carcinoma in situ (DCIS) (17.4%). This is in keeping with the literature as invasive ductal carcinoma is recognised as the most common subtype of breast cancer.14
Some other malignant lesions seen were malignant phyl-lodes, lymphoma and mucinous breast carcinoma - lesions which can mimic benign disease clinically as well as on imaging. They present as well-defined masses clinically and well-circumscribed masses on both mammogram and ultrasound. It is in these cases that histology becomes very important.
With regards to the benign diseases found on biopsy, Table IV shows that the most common findings were fibroadenomas (27.6% of all benign diseases found) which is in keeping with the literature (found in 25% of women),11 with fibrocystic breast disease (24.1%) and benign breast tissue (23%) being the next most common diagnoses.
From the above results, one can conclude that radiological assessment alone has a high sensitivity of 91.30% (79.2197.58%), however, the specificity in our institution is lower at 65.52% (54.56-75.39%). According to the literature, however, the sensitivity should be 99% with a specificity of 95.2%,15 thus there is room for improvement, and this further emphasises the need for the gold standard of therapy which is the triple assessment.
This study was limited by the population group sampled; this may not be representative of the full population of our country as it represents only a small subset based on the catchment area of HJH.
Conclusion
A vast array of BI-RADS categories were found within this population clinically assessed as presenting with benign disease with a radiological correlation of the majority (89.9%) being benign. Only 3.6% of the total sample were confirmed radiologically and histologically as malignant disease, which is in keeping with international standards.
Radiological imaging alone is highly sensitive but less specific when compared with the histological findings, emphasising that the triad of clinical, radiological and histological assessment is indeed necessary with regards to breast imaging and clinical diagnosis. Of note is the useful application of a triage system at a clinical level to streamline referral for imaging in a resource-limited health care setting.
Acknowledgements
The study was conducted and completed at the University of the Witwatersrand. Our thanks go to the staff at the Breast Imaging Unit at Helen Joseph Hospital for allowing us access to patient records and imaging. And to our families and friends for their support and advice.
Conflict of interest
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Funding source
None.
Ethical approval
Ethical clearance has been approved by Human Research Ethical Committee (Medical) Wits. Ethical Clearance Certificate No. M191172.
ORCID
NC Christofides https://orcid.org/0000-0003-3522-6643
G Rubin https://orcid.org/0000-0001-8435-3521
C-A Benn https://orcid.org/0000-0002-4777-4316
REFERENCES
1. Edge J. Benign breast conditions in young women. CME. 2010;28(11):500-2. [ Links ]
2. Marchant DJ. Benign breast disease. Obstet Gynecol Clin North Am. 2002;29(1):1-20. [ Links ]
3. Vorobiof DA, Sitas F, Vorobiof G. Breast cancer incidence in South Africa. J Clin Oncol. 2001;19(18):125-7. [ Links ]
4. Rungruang B, Kelley JL. Benign breast diseases: epidemiology, evaluation, and management. Clin Obstet Gynecol. 2011;54(1):110-24. [ Links ]
5. Dyrstad SW, Yan Y, Fowler AM, Colditz GA. Breast cancer risk associated with benign breast disease: systematic review and meta-analysis. Breast Cancer Res Treat. 2015;149(3):569-75. [ Links ]
6. Mansel RE, Webster D, Sweetland H, et al. Hughes, Mansel & Webster's. benign disorders of the breast. 3rd ed. Saunders (Ltd); 2009. [ Links ]
7. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424. [ Links ]
8. 2014 National Cancer Registry Tables [Internet]. National Health Laboratroy Service. 2014. Available from: http://www.nicd.ac.za/centres/national-cancer-registry/. Accessed 31 Oct 2019. [ Links ]
9. Lee J. Practical and illustrated summary of updated BI-RADS for ultrasonography. Ultrasonography. 2017;36(1):71-81. [ Links ]
10. D'Orsi C, Sickles EA, Mendelson EB, Morris EA. Breast imaging reporting and data system: ACR BI-RADS breast imaging atlas. 5th ed. American College of Radiology; 2013. [ Links ]
11. Stachs A, Stubert J, Reimer T, Hartmann S. Benign breast disease in women. Dtsch Arztebl Int. 2019;116(33-34):565-74. [ Links ]
12. Jatoi I. Screening clinical breast examination. Surg Clin North Am. 2003;83(4):789-801. [ Links ]
13. Hung WK, Chan SW, Suen DT, et al. Triaging referral to a specialist breast clinic. ANZ J Surg. 2006;76(5):310-2. [ Links ]
14. Sharma GN, Dave R, Sanadya J, Sharma P, Sharma KK. Various types and management of breast cancer: an overview. J Adv Pharm Technol Res. 2010;1(2):109-26. [ Links ]
15. Karim MO, Khan KA, Khan AJ, et al. Triple assessment of breast lump: should we perform core biopsy for every patient? Cureus. 2020;12(3):e7479. [ Links ]
 Correspondence:
Correspondence:
NC Christofides
Email: nicc1988@gmail.com














