Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.59 n.3 Cape Town Sep. 2021
http://dx.doi.org/10.17159/2078-5151/2021/v59n3a3474
BREAST DISEASE
An audit of patients clinically deemed as high risk for malignant breast pathology at the Helen Joseph Hospital Breast Clinic
H-M BrinkI; G RubinII; C-A BennIII; S LucasIV
IDepartment of Diagnostic Radiology, University of the Witwatersrand, South Africa
IIDepartment of Radiology, Helen Joseph Hospital, South Africa
IIIBreast Surgical Unit, Helen Joseph Hospital, South Africa
IVDepartment of Radiology, Chris Hani Baragwanath Academic Hospital, South Africa
ABSTRACT
BACKGROUND: The Helen Joseph Hospital Breast Clinic has implemented a clinical triage system for patients presenting with a variety of breast concerns. The goal of this system is to expedite the process from initial presentation to radiological assessment of patients with suspected breast malignancy or breast abscess in a resource limited setting. The objective was to assess the clinical, imaging and histological diagnoses of breast disease in these patients with malignancy and sepsis
METHODS: A retrospective audit of patients clinically deemed high risk for malignant breast pathology referred to the breast imaging unit (BIU) in 2018. Patients were triaged based on strict clinical criteria: presence of a breast mass with or without lymph nodes or a breast abscess. Patients that were subsequently referred for mammography/ultrasound were identified using the patient files in the BIU. Results were recorded on Microsoft Excel and analysed using SAS version 9.2
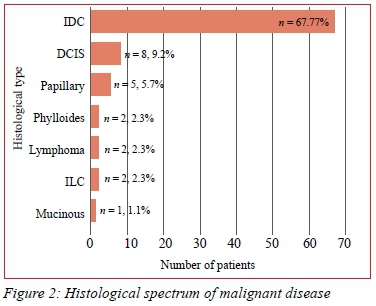
RESULTS: Three hundred and twenty-five patients were included in this study. Eighty-seven (26.8%) were diagnosed with breast cancer and 236 (72.6%) with benign disease. The most common presenting complaint was a palpable mass (n = 227; 69.9%). Ninety-five per cent of patients characterised as BI-RADS 5 had malignant disease. 55.8% of malignancies diagnosed on ultrasound had locally advanced disease. The most common histological diagnosis of malignancy was invasive ductal carcinoma (n = 67, 77%). The most commonly diagnosed benign disease was breast abscess (n = 42, 17.8%
CONCLUSION: BI-RADS findings correspond to similar studies, however, a large number of benign breast disease was diagnosed. This may indicate heightened clinical awareness of breast cancer diagnosis and early detection. A significant percentage of malignancies presented as locally advanced. Except for a lower number of invasive lobular carcinoma, the histological spectrum of malignant disease is similar to comparative studies
Keywords: malignant breast pathology, high risk patient, Helen Joseph Hospital Breast Clinic
Introduction
The Helen Joseph Hospital Breast Clinic has implemented a clinical triage system for patients who present at the breast clinic. This is an open access clinic where any patient with a breast concern is seen. Patients are triaged into three groups according to strict clinical criteria: high-, intermediate-, and low-risk cases.
Low risk includes patients with no clinical suspicion of breast disease - asymptomatic patients presenting for screening. Intermediate risk includes patients with unilateral breast pain, a breast mass deemed clinically benign, non-spontaneous nipple discharge, or palpable lymph nodes but no breast involvement.
High risk includes any patient with a breast mass that has a clinical suspicion of malignancy, with or without palpable axillary lymph nodes, or an acute breast collection/abscess. Even though patient age is not part of the triage protocol, patients with increased age are deemed more likely to have malignant breast disease and are more often referred in this high-risk category. This is at the referring clinician's discretion. These patients are referred to the Helen Joseph Breast Imaging Unit (BIU) for urgent imaging and, if necessary, intervention within seven days from presentation. The goal of this triage system is to expedite the process from initial presentation to diagnosis and the timeous management for any patient with a suspicion of breast malignancy. It also aims to decrease the patient burden on the BIU in a resource limited setting and it standardises the referral criteria for clinicians across varying levels of experience. Breast abscesses and other acute breast collections are added to this group as they require urgent intervention.
The aim of this study was to conduct an audit to assess the spectrum of breast disease clinically deemed high risk for malignant breast pathology, their clinical and imaging features, and their final histological diagnosis.
Context
Even though the incidence of breast cancer in Africa is low in comparison to other countries, the related morbidity and mortality is as high, or even higher, than developed countries.1
A recent Ghanaian study reviewed 330 histologically proven breast cancer patients. The peak incidence of diagnosis of breast cancer was in the age group of 40-49 years.2 This is in keeping with multiple other studies done in sub-Saharan Africa,35 which showed that patients in this region present at the pre- and perimenopausal stage, versus high-income countries where the majority of patients present postmenopausal.67 The different presenting complaints that were subsequently diagnosed as histologically confirmed breast malignancy were also noted. The most common presenting complaint was a breast lump (75.2%).2
Invasive ductal carcinoma (IDC) was the most common histological subtype identified (82.1%). This is in keeping with the trend elsewhere in Africa, Europe and worldwide.8
The Breast Imaging-Reporting and Data System (BI-RADS) system of reporting for breast disease aims to standardise mammography and ultrasound reports.9 An American study done in 2018, which focused on a majority African American demographic, studied the correlation between the mammographic BI-RADS category compared to the histological diagnosis. Breast cancer was diagnosed in 0.03% of patients with a BI-RADS grade of 1-3, 29% of patients reported as BI-RADS 4, and 89.7% of patients reported as BI-RADS 5.10
No previous research has been done to assess this population's specific burden of disease, highlighting the need for the study in this context.
Objective
The primary objective was to analyse the spectrum of imaging findings of the patients clinically deemed as high risk for malignant breast pathology at the Helen Joseph BIU. The secondary objective was to document the associated clinical and relevant laboratory findings.
Materials and methods
Research paradigm
A retrospective audit of imaging findings of patients clinically deemed high risk and for immediate breast imaging.
The patients who were referred to the Helen Joseph BIU from 1 January to 30 June 2018 and who were clinically deemed as high risk for malignant breast pathology and seen at the Helen Joseph Hospital BIU were considered. Patients with illegible records or missing imaging findings were excluded.
Files and records at the Helen Joseph Hospital BIU were accessed. The National Health Laboratory Services (NHLS) online database was accessed in order to obtain the relevant histology/HIV/MC&S results.
The data was collected using a pre-formulated data collection sheet and entered into a Microsoft Excel spreadsheet. Each patient was allocated a study number and only this number was linked to the patient's personal identifiable information.
A triage book is kept at the Helen Joseph Hospital BIU which contains the names and hospital numbers of each patient who is booked at the imaging unit as well as their triage status.
Each patient has a corresponding file that contains their imaging request form, imaging report, history questionnaire and a biopsy information sheet.
The triage book was used to identify the patients seen and triaged as high risk from 1-30 June 2018. The corresponding mammography files were then accessed to obtain their demographics, clinical history, imaging findings and histology results. This unit's practise is that every patient should receive a mammogram, except in the following cases: patients who are younger than 35 years of age start with ultrasound imaging and only if deemed necessary and appropriate are then referred for mammography; patients with painful or ulcerative breast pathology where mammography would cause too much discomfort for the patient; and patients who are physically unable to be positioned for mammography, for instance, bed-ridden patients.
The patient's HIV status was documented either from the request form, the history questionnaire or the NHLS online database. If no results were found for a 6-month window period prior to the patient's clinic date, the patient was determined as HIV "unknown".
Data analysis and statistics
Data was captured electronically in Microsoft Excel. Further analysis was done using SAS Version 9.2. Descriptive statistics namely frequencies and percentages were calculated for categorical data. Means and standard deviations or medians and percentiles were calculated for numerical data. The Shapiro-Wilk test was used to investigate if numerical data followed a normal distribution. A significance level p-value of 0.05 was used.
Results
Seven hundred and sixty patients were identified as high risk from the triage book, however several patient files were not found. The large number of missing patient files could be due to a variety of factors: if patients presented for follow-up appointments subsequent to their initial booking date, they were given a new file number which made the tracing of these patients' information difficult. A large number of patients also defaulted on their appointment dates, and some files were erroneously labelled as high risk, but were, in fact, patients presenting for annual screening - these patients were also excluded. Three hundred and thirty-four (334) patients with imaging were identified during the study period and nine of these patients were excluded from the study due to indecipherable imaging reports. The total number thus included was 325.
Demographics and presenting complaints
Table I depicts the patient demographics. Added are their presenting complaints and type of imaging obtained. Percentages of benign versus malignant disease are given. Two patients were not confirmed to have either malignant or benign disease as there was no histology for correlation, but these patients were suspected to have malignant disease based on their imaging features. These patients are added in the 'unknown' column.
The majority of patients were female (96.6%). All male patients were diagnosed with benign disease. The most common presenting complaint was a palpable mass for both benign and malignant disease. The median age of malignancies was 57, which was higher than for benign disease of 41.
Imaging findings
Tables II and III demonstrate the different imaging findings on mammography and ultrasound with comparison between malignant and benign disease. Of the patients who had masses present on mammography, 58.6% were malignant. This accounted for 78.2% of the total number of malignancies. All of the patients who had malignant masses on mammography (54/87 of malignancies) also presented with identifiable masses on ultrasound. 86/87 of malignancies had masses on ultrasound. The one patient with biopsy proven malignancy who did not have an identifiable mass on ultrasound presented with suspicious microcalcifications on mammography and no mass.
Spiculation was the most common border characteristic of the malignant masses (30.9%) on mammography. Forty (40) (52.6%) of malignancies on mammography had suspicious microcalcifications.
In Table III, we can see that 86 (51.5%) of masses seen on ultrasound proved to be malignant.
Only 65 out of these 86 patients with malignant masses had a size documented on ultrasound, of which 49 (75.3%) were larger than 2 cm and 12 (18.5%) larger than 5 cm. Thus, 61 out of 65 (93.8%) of presenting masses were larger than 2 cm. The majority of poorly circumscribed masses identified on ultrasound were malignant (88.2%).
Axillary adenopathy was present on ultrasound in 57 of the 86 (66.2%) patients presenting with malignancy. Of these 57 patients, 48 had malignant infiltration of their ipsilateral axillary nodes on ultrasound. Thus, 55.8% of patients presenting with breast carcinoma had ipsilateral malignant axillary nodal involvement. Of note is that most patients with malignant lymphadenopathy (35/48; 72.9%) presented with multiple suspicious ipsilateral axillary lymph nodes.
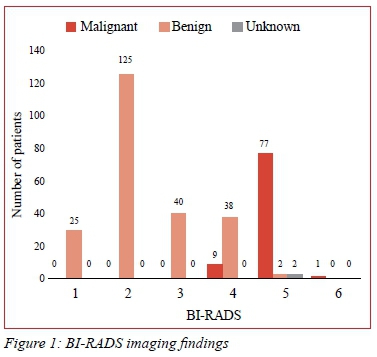
Figure 1 compares the BI-RADS imaging findings with malignant versus benign disease. Ninety-five per cent of breast lesions that were assessed as BI-RADS 5 proved to be malignant. The two patients with BI-RADS category 5 imaging and reportedly benign histology had suboptimal biopsy results with no representative histology of the lesion.
Spectrum of disease
Figure 2 depicts the histological spectrum of malignant disease. IDC formed the majority of the malignancies (77%). The most commonly diagnosed benign breast disease was breast abscesses (n = 42, 17.8%) followed by normal imaging findings (n = 35, 14.8%) and fibroadenomas (n = 29, 12.3%). Of the 42 diagnosed breast abscesses, 19 (45.3%) patients were HIV negative, six (14.3%) patients were HIV positive, and 17 (40.5%) patients had unknown HIV status.
Discussion
The Helen Joseph Hospital Breast Clinic has a triaging system allowing for timeous breast imaging referral and management of patients with suspected breast cancer. This aims to standardise the referral criteria for any clinician examining a patient with a breast concern. We initially expected to see a large majority of malignancies in this study, however, the majority proved to have benign disease. This is likely due to a high concern and awareness of the early diagnostic value of breast cancer as well as an indication of the spectrum of clinical experience in an academic teaching hospital. There is also a large number of patients suspected of having a breast abscess attending the breast clinic, and these are referred for imaging and immediate management.
The majority of patients included in the study were females (n = 314, 96.6%). Only 11 males were included, of which 100% were diagnosed with benign disease. Global and local trends show that male breast cancer comprises less than 1% of diagnosed breast malignancies.11,12 The lower rate in this study may be due to the low number of male patients who were seen during the study period.
The median age of patients diagnosed with breast malignancy was 57, with the largest number of patients presenting between 60-69. Interestingly, this is out of keeping with findings in several other sub-Saharan African studies where the peak incidence of breast cancer was in pre- and perimenopausal patients.3-5 This appears more in keeping with peak incidences in high income countries6,7 where women were of post-menopausal age.
The most common presenting complaint was a breast lump. This included 69.9% of all patients and 92% of malignancies. This is in keeping with a recent study done in Kumasi, Ghana, in which they showed that of 330 patients with histologically proven malignancies, 75.2% presented with breast lump.2
The majority of patients with breast malignancy had a mass present on ultrasound and mammography. It is worth noting that of the 65 malignant masses measured on ultrasound, 49 (75.3%) were greater than 2 cm. Metastatic nodes were seen on ultrasound in 48/86 (55.8%) of malignancies and 35 (40.7%) had multiple ipsilateral metastatic nodes. This would indicate that at least 55.8% of malignancies diagnosed on ultrasound had locally advanced disease based on imaging features.
Ninety-five per cent of patients characterised as BI-RADS 5, and 20.8% of patients characterised as BI-RADS 4 proved to have malignant disease. This is in keeping with an American study that was done in 2018 which focused on a majority African American demographic. The study compared the correlation between the mammographic BI-RADS category given in reports versus the final histological diagnosis. It was found that 29% of patients reported as BI-RADS 4 and 89.7% of patients reported as BI-RADS 5 were diagnosed with malignancy.10 This also corresponds to another recent Ghanaian study, where out of 54 histologically proven malignancies, 85.2% of patients had findings in keeping with BI-RADS 4 and 5.13
IDC (67, 77%) comprised the majority of diagnosed breast malignancies, followed by ductal carcinoma in situ DCIS (8, 9.2%). This is in keeping with the previously mentioned study done in Kumasi, Ghana where the different histological types of breast cancer were given.2 Out of 340 patients, 82.1% proved to have IDC. Another study done in the Central African Republic in 2018 also showed IDC to be the most common tumour at 64.9%, followed by invasive lobular breast cancer (ILC) (9.8%).14 ILC constituted only 2.3% of patients in our study, which was lower than in the above comparison studies.
Breast abscesses were the most common benign condition. This was expected as these patients are referred for immediate intervention. A large number of patients presented with lactational breast abscesses. A recent Zambian study found that HIV infection was a significant risk factor for developing lactational breast abscesses.15 In our study, only 14.3% of the total number of breast abscesses were known to be HIV positive. This could be due to a large number of the patients (40.5%) presenting as HIV unknown. The second most common finding was normal imaging. This highlights the difficulties faced in assessing breast disease if clinical examination alone is used.
Study limitations
A large number of patients had unknown HIV status due to difficulty in tracing results.
The majority of benign breast disease results are not biopsy proven, as BI-RADS 1-3 diagnoses commonly do not require biopsy according to the BI-RADS management guidelines. Some imaging occult malignancies may have been missed.
Self-identified race was not available from the patient files at the BIU - this limits the appropriate comparison to patient groups in comparison studies.
Another limiting factor is the low number of biopsy-proven malignant disease. This could partly be due to the large number of missing files from the initially identified number of high-risk patients.
Future applications
It was interesting to note that all of the masses that were seen mammographically were also identified on ultrasound. This would be valuable for a further study considering ultrasound as a possible screening tool for clinically suspicious masses in resource limited settings.
There were several missing files from the initially identified study sample. A large percentage of this is due to the filing system in the department as new file numbers are given to follow-up patients. This can be further assessed to possibly keep original file numbers regardless of the number of visits to aid future research in this department. Many patients also defaulted on their mammography appointments. Patients should be counselled regarding the importance of follow-up appointments at the initial clinical assessment. A large number of imaging reports did not comment on the relevant BI-RADS imaging categories. This can be highlighted and encouraged in mammography training. This is a study of a single centre breast unit triage system. Subsequent studies, with comparison to other triage systems, are needed and may highlight changes that should be implemented. This triage system does, however, significantly decrease the burden of the radiology department in a resource limited setting and can be considered for implementation in other centres.
Conclusion
This is an index study of a breast clinic triaging system. BI-RADS imaging findings largely correspond to other similar studies, however, a large number of benign breast disease was diagnosed in this study. This requires ongoing evaluation of the triaging system, but highlights that clinical evaluation of breast disease requires imaging and biopsy. Clinical presentation of breast malignancy at our centre corresponds to other comparative studies with the majority of patients presenting with palpable breast masses. A large number of our patients presented with locally advanced breast malignancy based on imaging. The histological spectrum of malignant breast disease is similar to the available literature, however, we saw a lower number of ILC. A large number of imaging reports did not report on the relevant BI-RADS imaging categories. This should be further encouraged during mammography training.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
The study was approved by the Human Research Ethics Committee of the University of the Witwatersrand, approval number M190675.
ORCID
H-M Brink https://orcid.org/0000-0002-8359-6393
G Rubin https://orcid.org/0000-0001-8435-3521
C-A Benn https://orcid.org/0000-0002-4777-4316
S Lucas https://orcid.org/0000-0002-0378-183X
REFERENCES
1. Forouzanfar MH, Foreman KJ, Delossantos AM, et al. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378(9801):1461-84. [ Links ]
2. Ohene-Yeboah M, Adjei E. Breast cancer in Kumasi, Ghana. Ghana Med J. 2012;46(1):8-13. [ Links ]
3. Gakwaya A, Kigula-Mugambe JB, Kavuma A, et al. Cancer of the breast: 5-year survival in a tertiary hospital in Uganda. Br J Cancer. 2008;99(1):63-7. [ Links ]
4. Rahman GA, Olatoke SA, Agodirin SO, Adeniji KA. Socio-demographic and clinical profile of immuno-histochemically confirmed breast cancer in a resource limited country. Pan Afr Med J. 2014;17:182. [ Links ]
5. Mbonde MP, Amir H, Mbembati NA, et al. Characterisation of benign lesions and carcinomas of the female breast in a sub-Saharan African population. Pathol Res Pract. 1998;194(9):623-9. [ Links ]
6. Finnish CR. Cancer stat fact sheets. Helsinki, Finland: Institute for Statistical and Epidemiological Cancer Research; 2011. [ Links ]
7. Cancer RoN. Cancer in Norway: Cancer in Norway 2009 - Cancer incidence, mortality, survival and prevalence in Norway. Oslo, Norway; 2011. [ Links ]
8. Abdulrahman GO Jr, Rahman GA. Epidemiology of breast cancer in Europe and Africa. J Cancer Epidemiol. 2012;2012:915610. [ Links ]
9. Rao AA, Feneis J, Lalonde C, Ojeda-Fournier H. A pictorial review of changes in the BI-RADS 5th Ed. Radiographics. 2016;36(3):623-39. [ Links ]
10. Hu S, Szymanski J, Khairy Z, Lo Y, Wang Y. Breast pathology and mammography BI-RADS category correlation study - a single institute experience. Ann Diagn Pathol. 2018;35:11-5. [ Links ]
11. Ssemmanda S, Katagirya E, Bukirwa P, et al. Breast diseases histologically diagnosed at a tertiary facility in Uganda (2005-2014). BMC Cancer. 2018;18(1):1285. [ Links ]
12. Liu N, Johnson KJ, Ma CX. Male breast cancer: an updated surveillance, epidemiology, and end results data analysis. Clin Breast Cancer. 2018;18(5):e997-e1002. [ Links ]
13. Badu-Peprah A, Adu-Sarkodie Y. Accuracy of clinical diagnosis, mammography and ultrasonography in preoperative assessment of breast cancer. Ghana Med J. 2018;52(3):133-9. [ Links ]
14. Balekouzou A, Yin P, Bekolo CE, et al. Histo-epidemiological profile of breast cancers among women in the Central African Republic: about 174 cases. BMC Cancer. 2018;18(1):387. [ Links ]
15. Kapatamoyo B, Andrews B, Bowa K. Association of HIV with breast abscess and altered microbial susceptibility patterns. Med J Zambia. 2010;37(2):58-63. [ Links ]
 Correspondence:
Correspondence:
H-M Brink
Email: heilabrink@gmail.com














