Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.59 n.2 Cape Town Jun. 2021
http://dx.doi.org/10.17159/2078-5151/2021/v59n2a3441
CASE REPORT
Duodenojejunal intussusception due to an inflammatory fibroid polyp: a mimic of acute pancreatitis
H Reiner; I Mia; WC Coetzee; A Lambrechts; S Hofmeyr
Division of Surgery, Tygerberg Academic Hospital, University of Stellenbosch, South Africa
SUMMARY
This report describes an extremely unusual cause of acute pancreatitis. It highlights the value of cross-sectional imaging, in the absence of alcohol and gallstone aetiology, to establish a diagnosis and direct management. Computed tomography (CT) revealed a duodenal jejunal intussusception. A benign inflammatory fibroid tumour, acting as a lead point, was surgically resected and the patient made an unremarkable recovery without further episodes of acute pancreatitis.
Case report
A 37-year-old female presented with symptoms and signs suggestive of mild acute pancreatitis, which included epigastric pain and nausea without vomiting. She had no significant medical or surgical history and denied ethanol abuse. Clinical examination revealed mild epigastric tenderness, with the rest of abdominal and systemic examination being unremarkable.
Laboratory investigations included normal liver function tests, urea, creatinine, electrolytes and full blood count, but the serum lipase level was raised at 1349 U/L. Chest and abdominal plain X-rays revealed no obvious abnormalities. Abdominal ultrasound revealed a dilated common bile duct of 10.8 mm and a main pancreatic duct of 2.3 mm in diameter, with no sonographic features of pancreatitis, no cholelithiasis and no mass lesions. Conservative therapy with intravenous fluids and analgesia did not result in any significant improvement in the patient's symptoms, leading to further investigation with computed tomography (CT).
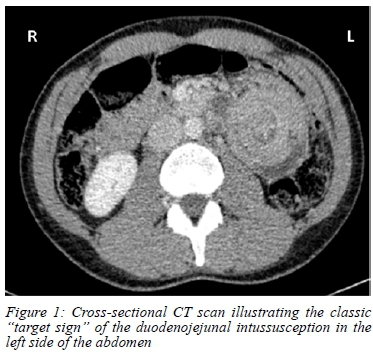
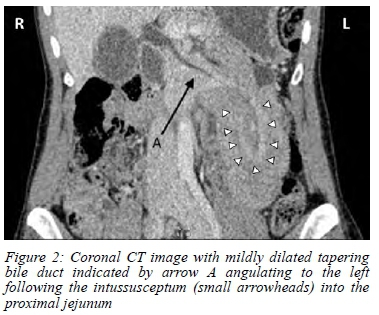
CT abdomen revealed duodenojejunal intussusception with the pancreas forming part of the intussusceptum into the receiving proximal jejunum (Figure 1). This resulted in angulation of the biliary and pancreatic ducts to the patient's left following the direction of the intussusception (Figure 2). Air locules within the duodenum raised concern for pneumatosis intestinalis, later shown to be artefactual by intraoperative findings.
Preoperative endoscopy revealed a stalk originating from the second part of the duodenum, disappearing into the distal duodenum. This area could be passed with the endoscope, revealing a mobile mass in the distal duodenum/upper jejunum. Bile was noted in the duodenum but the relationship of the stalked mass to the Ampulla of Vater could not be determined endoscopically. No mucosal ischaemia was evident.
An upper midline laparotomy was followed by complete Kocherisation of the duodenum. The findings were a palpable mass in the proximal jejunum, distal to the ligament of Treitz and invagination of the second part of the duodenum into itself.
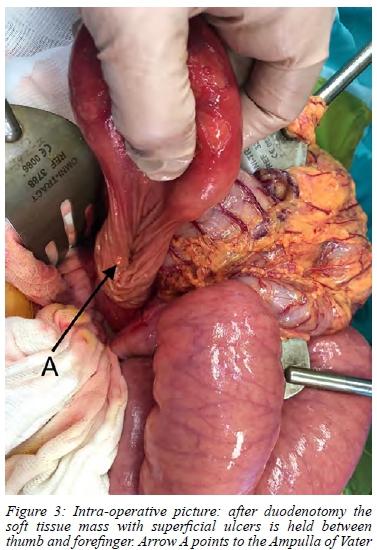
The small bowel mass was manually reduced from distal to proximal with gentle external pressure. With the large mass present in the dilated second part of the duodenum, a longitudinal duodenotomy was performed in the antime-senteric aspect, through which the mass was delivered (Figure 3). The lead point and origin of the mass was in the antimesenteric wall of the second part of the duodenum, just proximal to the level of the ampulla. The mass was situated in a submucosal position and the overlying mucosal surface appeared benign. Three small superficial ulcerations were present. The largest diameter of the mass was approximately 5 cm.
A submucosal excision of the mass was performed, preserving the muscularis propria. The duodenotomy was closed longitudinally without luminal narrowing. She was discharged home on the fifth postoperative day with no immediate postoperative complications. Histopathology reported an inflammatory fibroid polyp of the duodenum with clear resection margins.
Discussion
Intestinal intussusception is uncommon in the adult population. Most cases of intussusception present with intestinal obstruction and up to 30% of cases in adults are associated with malignant pathology.1 Due to the fixation of the pancreas and associated duodenal C-loop to the retroperitoneum, duodenojejunal intussusception is exceptionally rare,2 with less than twenty cases reported in the literature. Causes of duodenal intussusception include duodenal ulcers,3 duplication cysts,4 adenomatous and other polyps,5 as well as adenocarcinomas.1 Gastric outlet obstruction is the most common mode of presentation.1 In this case, the presentation was that of acute pancreatitis, which is almost unprecedented. One similar case has been reported, which describes a 13-year-old male presenting with recurrent episodes of pancreatitis, later shown to be due to a fenestrated duodenal web in the second part of the duodenum acting as the lead point for the intussusception.6 Duodenal intussusception should be considered in the differential diagnosis of gastric outlet obstruction (GOO). GOO due to gastro-jejunal intussusception is more common, with a pathological lead point present in the distal stomach.7 Gastrointestinal stromal tumours (GISTs) have been known to account for gastro-duodenal intussusception due to increased mobility and tumour weight that result in tumour "drooping".8 In our patient the duodenojejunal intussusception was most likely caused by a similar mechanism.
Inflammatory fibroid polyps (IFPs) are benign mesenchy-mal tumours. The cell of origin is unknown and although they share a common PDGFRA gene mutation, IFPs are clearly distinguished from GIST by their morphology, submucosal origin and clinical behaviour. IFPs accounts for 0.1-3% of all gastric polyps. Most are small lesions diagnosed incidentally, while larger polyps tend to display surface ulceration.3
A few cases are documented to have presented with upper gastrointestinal haemorrhage,2 but biliary and/or pancreaticduct (PD) dilatation has not been reported. In this case the presence of biliary and pancreatic duct dilation raised concern for malignancy prior to surgical exploration. The report of pneumatosis intestinalis on CT scan was also worrisome, but preoperative endoscopy was of benefit in assessing the viability of the bowel as well as noting a possible lead point with a benign appearance. Preoperative biopsies would not have been helpful as the mass was mobile, difficult to visualise on endoscopy and in a submucosal location, resulting in biopsies that were unlikely to be representative of the lesion. We considered a GIST to be the most probable preoperative diagnosis.
Endoscopic treatment of duodenal mass lesions includes snare polypectomy,7 but was not possible in this case due to the large size of the lesion, as well as the intussusception that required surgical reduction. In children, fluoroscopic reduction of duodenal intussusception is the treatment of choice, while in adults, resection is advised due to the higher risk of malignant lead points that may require oncological resection. Reduction prior to resection should be avoided if the bowel is compromised due to the high risk of perfo-ration.2
Our surgical approach was simple and consisted of manual reduction of the intussusception, followed by antimesenteric duodenotomy and organ-sparing resection of the mass, since no malignancy or bowel ischaemia was suspected. The duodenum was re-approximated in a longitudinal fashion without causing narrowing due to the dilated condition of the duodenum.
Conclusion
Duodenal intussusception is rare in adults and may mimic acute pancreatitis. The diagnosis is easily made with CT, and upper gastrointestinal endoscopy may aid in identifying a lead point and the exclusion of ischaemia. Surgery consists of reduction of the intussusception with resection of the lead point tailored to its point of origin and the presence of malignancy.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
Ethical approval was received from the Stellenbosch University Human Research Ethics Committee C20/07/023.
ORCID
H Reiner https://orcid.org/0000-0002-9493-5944
I Mia https://orcid.org/0000-0002-2446-960X
WC Coetzee https://orcid.org/0000-0001-6752-1124
A Lambrechts https://orcid.org/0000-0003-0565-3978
S Hofmeyr https://orcid.org/0000-0002-9300-0661
REFERENCES
1. Alexander R, Traverso P, Bolorunduro OB, et al. Profiling adult intussusception patients: comparing colonic versus enteric intussusception. Am J Surg. 2011;202(4):487-91. https://doi.org/10.1016/j.amjsurg.2011.02.006. [ Links ]
2. Marinis A, Yiallourou A, Samanides L, et al. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15(4):407. https://doi.org/10.3748/WJG.15.407. [ Links ]
3. Lingala S, Moore A, Kadire S, et al. Unusual presentation of duodenal ulcer presenting with duodenal intussusception. ACG Case Rep J. 2018;5(1):e25. https://doi.org/10.14309/crj.2018.25. [ Links ]
4. Koike Y. A rare cause of recurrent acute pancreatitis: duodenum intussusception by a fenestrated duodenal web. Gastrointest Endosc. 2017;86(3):567-8. https://doi.org/10.1016/j.gie.2017.03.021. [ Links ]
5. Henry PY, Nair PMC, Anand N, Lal RVF. Solitary Peutz-Jeghers polyp presenting as duodenal intussusception. Indian J Pediatr. 2014;81(10):1122-3. https://doi.org/10.1007/s12098-014-1479-3. [ Links ]
6. Zhao B, Zhou X, Wang W. Duodenal descending part-jejunum intussusception and upper gastrointestinal bleeding caused by duodenal fibrolipoma: a case report. BMC Surg. 2019;19(1):169. https://doi.org/10.1186/s12893-019-0634-1. [ Links ]
7. Yamauchi K, Iwamuro M, Ishii E, et al. Gastroduodenal intussusception with a gastric gastrointestinal stromal tumour treated by endoscopic submucosal dissection. Intern Med. 2017;56(12):1515-9. https://doi.org/10.2169/internalmedicine.56.8160. [ Links ]
8. Schildhaus H-U, Cavlar T, Binot E, et al. Inflammatory fibroid polyps harbour mutations in the platelet-derived growth factor receptor alpha ( PDGFRA) gene. J Pathol. 2008;216(2):176-82. https://doi.org/10.1002/PATH.2393. [ Links ]
 Correspondence:
Correspondence:
A Lambrechts
Email: antonlam@sun.ac.za














