Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.59 n.2 Cape Town Jun. 2021
http://dx.doi.org/10.17159/2078-5151/2021/v59n2a3468
CASE REPORT
Laparoscopic repair of a delayed traumatic bladder injury
S MakhadiI; MS MoengII, III; TR GovenderII; ZS LungaII
IDr George Mukhari Academic Hospital, Sefako Makgatho Health Sciences University, South Africa
IICharlotte Maxeke Johannesburg Academic Hospital, University of the Witwatersrand, South Africa
IIIMilpark Hospital, South Africa
SUMMARY
Isolated bladder injuries from falls are not common; we report a laparoscopic bladder repair in a patient with delayed presentation. There are about 20 case reports of laparoscopic repair of traumatic bladder reported in the literature, but none with such a delayed presentation.1 We describe the technique of laparoscopic bladder repair. The delay in the presentation might have facilitated laparoscopic repair as it might have excluded bowel injuries.
Case report
We present a 50-year-old man who fell from the stairs and sustained blunt abdominal trauma. He presented to our emergency department four days after the event. He gave a history of drinking alcohol before the fall. His main complaint was progressive abdominal distention and abdominal discomfort. On examination of his abdomen, he was noted to be distended but non-peritonitic. A transurethral catheter was inserted, and there was no gross haematuria noted. eFAST showed a large amount of free fluid in the abdomen. A CT cystogram showed an intraperitoneal bladder injury. No other injuries were reported on the CT scan. He underwent a laparoscopic bladder repair.
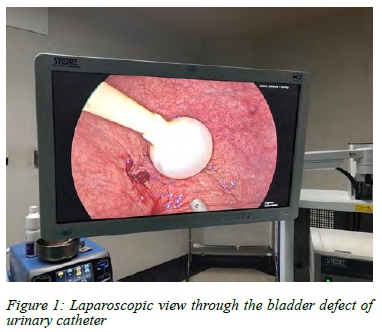
In theatre, the patient was supine and under general anaesthetic. A 12 mm infra-umbilical port was inserted, and the peritoneum was insufflated to 15 mmHg. Two 5 mm ports were inserted in the left and right lower quadrants of the abdomen. There was a defect noted at the dome of the bladder measuring 4 cm (AAST grade 4 bladder injury), and 8 litres of uroperitoneum was suctioned. The was no septic contamination or altered blood present in the peritoneum. The bladder trigone was normal. The catheter was visualised in the bladder (Figure 1), and there was no extraperitoneal extension of the injury. The bladder injury was then repaired using interrupted vicryl 2.0 sutures in two layers, pre-cut to 20 cm (Figure 2). 200 ml of saline was instilled into the bladder via the transurethral catheter to check for a leak.

Postoperatively the patient was given analgesia, and his urine output was monitored as per the standard of care. The postoperative period was uncomplicated, with no evidence of haematuria by day three post-operation. The pain was well controlled, and he was mobilising very well. He was discharged with his transurethral catheter and was asked to come back on day 7 postoperatively for catheter removal. At his outpatient follow-up, he was well with no abdominal pain or distention, and his transurethral catheter was removed. No cystogram was deemed necessary as this was a simple intraperitoneal bladder injury repair. He passed urine well, and no complications were reported.
Discussion
Bladder injuries occur in 1.6-10% of blunt abdominal trauma and are associated with significant morbidity.1-4 Traumatic bladder injuries may result from blunt or penetrating injuries. Bladder injuries can be intraperitoneal or extraperitoneal. In a study done in South Africa, Pietermaritzburg, the majority of bladder injuries were from penetrating injuries (65%) and blunt injuries (22%).5 Intraperitoneal bladder injuries were more common, representing 60% versus 22% extraperitoneal injuries.5 Intraperitoneal bladder injuries are treated with the surgical repair; this is often done via laparotomy to exclude other injuries. Great strides have recently been made in the use of laparoscopy in trauma.
Bladder injuries present with gross haematuria, seen in 67-95% of cases.4 Microscopic haematuria may be seen in 5% of cases.4 Other signs such as low urine output, elevated creatinine levels, oedema of the perineum/thigh, inability to urinate and suprapubic tenderness should raise an index of suspicion for bladder injury.5-8 However, our patient did not present with gross haematuria despite the apparent abdominal distention. A high index of suspicion should be maintained in patients with free fluid on eFAST, especially without peritoneal signs even when delayed. The diagnostic study of choice to evaluate a bladder is a CT cystogram or retrograde cystogram.1-4,6-8 The two modalities have similar sensitivity and specificity.1,2
We prefer to repair bladder injuries as soon as they are diagnosed. The repair is usually done via laparotomy due to the fear of missing injuries and limited laparoscopic skills in most centres. This shortfall is not as major a concern as before due to the advances in imaging and laparoscopy skills. Currently, evidence suggests that it is possible to repair traumatic bladder injuries laparoscopically1-4,6-7.
The first laparoscopic traumatic bladder repair was reported in 1996 by Iselin et al.6 Since then, multiple case reports of laparoscopic bladder repairs have been published.7 Benefits of laparoscopy include decreased hospital stay, less postoperative pain, more rapid return to work, decreased intra-abdominal adhesions and reduced risk of hernias.1,2 Case series demonstrate the safety and advantages of traumatic bladder repair.1,2,6 The primary concern has always been missing other injuries. Koto et al. showed the safety and reliability of laparoscopy in trauma.8
The procedure involves suctioning the urine, and the bladder injury is usually located at the dome and obvious. In the open technique, the bladder is inspected inside for occult injuries at the bladder neck, urethral orifices, and trigone. During laparoscopic repair, these areas are magnified and easily identifiable. The repair is performed with an absorbable suture to avoid a nidus for urinary stones. This can be done in a single or double layer in a continuous or interrupted manner.1-4 The repair needs to be watertight when performed. The testing of the repair using saline water or methylene blue via a urinary catheter is not always necessary.
After the repair, patients are treated for 7-10 days with a urinary catheter. It is possible to discharge stable patients home with a urinary catheter. A follow-up cystogram to prove healing is unnecessary for simple bladder repair but should be considered in complex bladder repair.
Laparoscopic bladder repair is an acceptable procedure and is safe in skilled hands. There is room for improvement of laparoscopic skills in trauma care. The physiology on presentation and associated injuries may limit the application of this technique. Laparoscopic technology has had significant advancements since the 1990s with many improvements in image quality and instrumentation.1-4 Patients with isolated traumatic bladder injuries may benefit from laparoscopic repair and potentially improve their outcomes.
Conclusion
Repair of traumatic bladder rupture can be done laparoscopically in a selected number of patients, even if their presentation to the emergency department is delayed. Post bladder repair, patients can be discharged home with urinary catheters for 7-10 days.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
Ethical approval was obtained from the University of the Witwatersrand Human Research Ethics Committee M190589.
ORCID
S Makhadi https://orcid.org/0000-0003-3381-5866
MS Moeng https://orcid.org/0000-0001-7459-3388
TR Govender https://orcid.org/0000-0001-7937-749X
ZS Lunga https://orcid.org/0000-0002-8369-9608
REFERENCES
1. Kim B, Roberts M. Laparoscopic repair of traumatic intraperitoneal bladder rupture: case report and review of the literature. Can Urol Assoc J. 2012;6(6):E270-E273. [ Links ]
2. Arnold MR, lu CD, Thomas BW, et al. Advancing the use of laparoscopy in trauma: repair of intraperitoneal bladder injuries. Am Surg. 2019;85(12):1402-4. [ Links ]
3. Marchand TD, Cuadra RH, Ricchiuti DJ. Laparoscopic repair of a traumatic bladder rupture. J Soc Laparoendosc Surg. 2012;16:155-8. [ Links ]
4. Mahat Y, Leong JY, Chung PH. A contemporary review of adult bladder trauma. J Inj Violence Res. 2019;11(2):101-6. [ Links ]
5. Urry RJ, Clarke DL, Bruce JL, Laing GL. The incidence, spectrum, and outcomes of traumatic bladder injuries within the Pietermaritzburg Metropolitan Trauma Service. Injury. 2016;47(5):1057-63. [ Links ]
6. Iselin CE, Rohner S, Tuchschmid Y, Schmidlin F, Graber P. Laparoscopic repair of traumatic intraperitoneal bladder rupture. Urol Int. 1996;57:119-21. [ Links ]
7. Al-Aghbari S, Al-Harthy A, Ahmed M. Laparoscopic repair of traumatic intraperitoneal bladder rupture. Sultan Qaboos Univ Med J. 2011;11(4):515-8. [ Links ]
8. Koto MZ, Matsevych OY, Aldous C. Diagnostic laparoscopy for trauma: how not to miss injuries. J Laparoendosc Adv Surg Tech A. 2018;28(5):506-13. [ Links ]
 Correspondence:
Correspondence:
S Makhadi
Email: Sm61459@gmail.com














