Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.59 n.2 Cape Town Jun. 2021
http://dx.doi.org/10.17159/2078-5151/2021/v59n2a3457
BENIGN BREAST DISEASE
Is conservative management of fibroadenomas feasible? 5-year results from the Durban Breast Unit
N BarakzaiI; E MansoorI; I BuccimazzaII, III
IDepartment of General Surgery, Nelson R Mandela School ofMedicine, University of KwaZulu-Natal, South Africa
IIDepartment of Specialised Surgery, Inkosi Albert Luthuli Central Hospital, South Africa
IIIBreast Unit, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: Fibroadenomas (FAs) usually present in young women and, despite being the commonest benign breast masses, are often excised. This study aimed to assess the results of a conservative management protocol in the setting of dedicated breast clinics to reassess the validity of this conservative approach
METHOD: A retrospective chart review of a prospectively maintained database of the index presentation of patients diagnosed with FAs on triple assessment at the breast clinics of Inkosi Albert Luthuli Central Hospital (IALCH) and Addington Hospital (ADH) was undertaken. Women under 35 years with FA less than 5 cm and agreeable to the 5-year conservative management strategy from 2008 to 2015 were included. Variables assessed over the 5-year study period included adherence to clinic visits and any change in size of the lesion(s
RESULTS: Three hundred and six women were studied. The mean age of presentation was 21.5 years (IQR 12-34), and the mean FA size was 2.43 cm (IQR 0.5-4.8). 72.9% were of African ethnicity. 76.5% had a single FA, and in 16.3%, they were bilateral. 50.7% of patients were lost to follow-up, and 9.6% (n = 25) had spontaneous resolution of their FA. Conservative management of FAs was feasible in only 26.1% of patients
CONCLUSION: Conservative management of FAs over 5 years is not practical in our local setting due to the high patient attrition rate. In those who completed the 5-year observation period, only 1 in 10 patients had complete resolution of their FA
Keywords: conservative management, fibroadenomas, FA, benign breast, excision, spontaneous regression
Introduction
Fibroadenomas (FAs) are the commonest benign breast lesions in women1 and constitute approximately 50% of all breast biopsies and about 75% of biopsies in women under the age of 20.2,3 They are believed to be aberrations of normal breast development, especially in the second and third decades of life.4,5 FAs arise from stromal and epithelial connective tissue cells and contain receptors for both oestrogen and progesterone. It is believed that these lesions have a hormonal aetiology related to the increased sensitivity of breast tissue to oestrogen. For this reason, FAs tend to proliferate during pregnancy and shrink during menopause.
Despite the high incidence of FAs, there is controversy regarding whether they should routinely be excised or observed. Growth patterns of FAs are unpredictable, with approximately 50% regressing, 25% remaining static and 25% increasing in size over a five-year period.3 There have been no long-term studies, but it is likely that most FAs regress toward the end of a woman's reproductive years. Until the 1980s, the majority of FAs were excised for reasons that included: cancer phobia, lack of knowledge of their natural history, patient requests and a family history of breast cancer.6-8 In the following two decades, reports showed that cytologically proven FAs may be managed conservatively. The shift to conservatism is largely attributed to the advent of ultrasound that aids in characterising benign lesions and differentiating them from malignancies. This leads to an improved overall diagnostic efficacy of the triple assessment, which provides up to a 95% (+ 2% SD) accurate differentiation between benign and malignant lesions.9
Understanding the natural history of FAs and identifying patients that can be safely observed without the need for routine surgical intervention is desirable in a resource-constrained environment where surgical resources and expertise may be limited. Excision should be reserved for specific indications, and determined by Unit policy, thus reducing healthcare costs and unnecessary breast surgery in young patients. However, a conservative strategy requires adherence to prolonged follow-up, which may be difficult in a poor socio-economic population group and a dysfunctional healthcare system. Hence guidelines for conservative management remain institution based, with a lack of universality.
This study was prompted by the dearth of cogent strategies for managing FAs and variability in follow-up schedules mentioned in the literature.
The primary aim of the study was to assess the results of a conservative approach to the management of FAs in our setting and determine whether the local population group was able to adhere to the 5-year programme, and if not, to identify the ideal follow-up duration that would allow us to derive a cogent conservative management protocol without losing a large number of patients to follow-up. The secondary aim was to develop a pragmatic algorithm based on the results of the current conservative strategy.
Method
A retrospective chart review of a prospectively maintained database of the index presentation of patients diagnosed with FAs on triple assessment at the breast clinics of Inkosi Albert Luthuli Central Hospital (IALCH) and Addington Hospital (ADH) was undertaken. The study group included all women under the age of 35 with FAs less than 5 cm who were agreeable to the 5-year conservative management strategy during the 7-year study period from January 2008 to December 2015. The conservative management policy was instituted in 2008. The duration of observation was based on the natural history of these lesions as proposed in the literature1,4,7,8,10 and the protocol described below.
The conservative management protocol entailed confirmation of FAs by way of triple assessment defined as clinical breast examination using palpation and callipers, ultrasound imaging of the breast by radiologists and biopsy of the lesion via fine needle aspiration cytology, with six monthly palpation-based clinical assessment of the FA size, usually performed by the same physician. Ultrasound imaging of the breast by radiologists was to confirm concordance with clinical findings and detect other occult lesions in both breasts; all detected lesions were measured, however, for the purpose of the study, only measurements by clinical examination were used. Change in size was noted to the nearest millimetre. Ultrasound was only used at the initial consult. Those who did not require upfront excision as per Unit policy (age > 35 years and/or size > 5 cm) were counselled regarding conservative management for a defined period (observation) versus excision. No formal consent form was signed by the patients. Those who declined to be managed conservatively were offered excision and excluded from the study.
Observation was terminated if there was complete resolution of the lesion without the need for surgical excision during the period of conservative management. Complete resolution refers to a clinically impalpable lesion. Provision was made for cross-over to surgical treatment if conservative management was no longer acceptable to the patient. Surgical excision was also performed if the lesion increased in size (any increase by > 10 mm was considered an indication for surgery), failed to resolve or the patient reached the age of 35 years (whichever came first) during the five-year observation period. Feasibility of conservative management was defined as a non-surgical, successful adherence to the 5-year observation programme in lesions that did not resolve during this period. It was still deemed feasible if the FA resolved within the 5-year period.
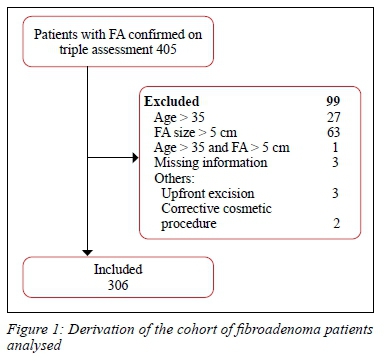
Figure 1 shows the numbers assessed, excluded and analysed.
All pregnant and lactating women were initially managed conservatively, irrespective of lesion size, until delivery or cessation of lactation, after which the strategy was revised: resection for lesions > 5 cm and conservative management for those < 5 cm.
Continuous variables included age, duration of symptoms, size of the lesions, duration of follow-up and size during follow-up (static/increased/decreased/resolved). Categorical variables include ethnicity, pregnancy status, lactation, use of oral contraceptive pills, history of prior FA assessment and/or excision, number of lesions (single vs multiple based on clinical assessment) and laterality (unilateral vs bilateral also based on clinical assessment). Family history of breast cancer was not analysed as a variable as it does not influence FA management decisions in the Unit.
IBM SPSS version 25 was used to analyse the data. A profile of the patients was generated by summarising the data using frequency tables and percentages for categorical variables, and summary statistics including means, standard deviations and ranges for continuous variables. Associations between feasibility and various factors were tested using chi-square tests for categorical factors, t-tests for continuous normally distributed factors, and Mann-Whitney tests for non-normally distributed variables. A p-value < 0.05 was considered as statistically significant.
Results
Three hundred and six women fulfilled the inclusion criteria. Their mean age was 21.5 years (range: IQR 12-34 years). African ethnicity predominated (223/306; 72.9%), followed by Indian ancestry (68/306; 22.2%), mixed ethnicity (11/306; 3.6%) and Caucasian ancestry (4/306; 1.3%).
The duration of symptoms ranged from 1 month to 120 months, with 75% of women presenting with symptoms < 18 months.
At presentation, 2.6% (8/306) of patients were pregnant, 2.6% (8/306) lactating and 12.4% (38/306) on oral contraceptives. Most patients (281/306; 91.8%) had no previous history of a breast lump, 7/306 (2.3%) patients had a previous assessment of a breast mass and 18/306 (5.9%) patients had a previous excision of a breast mass of undetermined histology.
The mean size of the FAs was 2.43 cm (IQR range 0.54.8 cm). The majority of women presented with a single FA (234/306; 76.5%); only 23.5% (72/306) had multiple FAs.
Most FAs were unilateral (256/306; 83.7%). Bilateral FAs occurred in 16.3% (50/306) of patients.
Follow-up
Of the women studied, 85% (260/306) returned for at least one follow-up visit, and 15% (46/306) never returned after the index consultation. Overall, 155/306 (50.7%) patients were lost to follow-up (Table I). Of these patients, 105/306 (34.3%) defaulted review in the first year. 55/306 patients (18%) are currently being followed-up, and 96 (35.68%) were discharged from further follow-up. Discharges comprised of patients whose lumps had resolved (n = 25) or who had an excision for any reason (increase in size or personal preference, n = 71).
Progression
In the assessable cohort of 260 patients, the FAs remained static in 23.1% (60/260), increased in size in 28.1% (73/260), decreased in size in 39.2% (102/260), and in 9.6% (25/260) of patients, there was complete resolution of the FA(s). The average initial size of FAs that underwent complete resolution was 2.1 cm (90.1% of FAs that underwent complete resolution were < 3 cm in size). The majority of patients did not undergo surgical excision: 76.8% (235/306) compared to 23.2% (71/306) who had surgery. Reasons for surgical excision during the observation period included pain (10/71; 14.1%), FAs that increased in size to > 5 cm (7/71; 9.9%), reached age of35 years and over (5/71; 7.0%), declined to continue with conservative management (3/71; 4.22%), and unspecified requests (46/71; 64.8%). All patients who had surgery during the observation period were discharged. The histology report of all these patients confirmed a FA. There were no reports of a phyllodes tumour.
Feasibility of conservative management
Conservative management was deemed to have failed (not feasible) if the patient did not adhere to the 5-year observation programme or had excision of the FA within that period. It was still deemed feasible if the FA resolved within the 5-year period. During the conservative management period, the lesion was excised for the following reasons: on patient request following a variable observation period, if there was an increase in size of the lesion (> 10 mm) or failure to resolve during the 5-year observation period, or the patients reached the age of 35 years.
The feasibility of cases as depicted in Table 1 shows that feasibility rates decline every year during the follow-up period, being 63% (195/306) in the first year and only 26% (80/360) by year 5.
Table II shows no statistically significant associations regarding feasibility of conservative management in the variables tested.
Table III shows that age at presentation and FA size had no effect on feasibility.
Table IV shows the median follow-up for conservative management failures and feasible cases was 16 and 25 months, respectively, though this difference was not statistically significant.
Patients without surgery whose lumps decreased in size
There were 89 cases (29%) who were classified as failures, as they did not complete the full observation period and were lost to follow-up, but the lump decreased in size. These patients had FAs ranging from 0.5-4.8 cm with a mean of 2.75 cm. Their median follow-up time was 18 months, with 75% of patients having a follow-up period of < 26 months. It remains unknown whether this group may have achieved regression of the lesion if a longer follow-up period for conservative management had been undertaken.
Discussion
The conservative management of FAs has been extensively researched. The literature is replete with studies suggesting a role for conservative management in patients with FAs under the age of 35 years and a mass of below 5 cm, following a confident diagnosis of FA using triple assessment, as there is a negligible risk of malignant transformation and a high rate of regression.5,6,11,12
Notwithstanding, there are no cogent universal guidelines for the conservative management of FAs, particularly in respect of duration of observation and the need for excision.
Existing policies are based on individual institutional experiences and provider preferences. This Unit's policy of conservatism (observation in lieu of routine excision) was based on the reported natural history of FAs, i.e., that most lesions (50%) resolve over a period of 5 years and that most would therefore not require excision or further follow-up.
Our study aimed to assess whether conservative management of FAs over a 5-year period is feasible in our local, resource-limited setting, namely whether patients adhere to a prolonged observation period. 50.7% of all patients were lost to follow-up. No specific factors could be attributed to the feasibility or failure of conservative management of FAs. A 1996 British study showed that conservative management of FAs in patients under the age of 40 years was acceptable to the majority of women, with most women being able to adhere to follow-up for at least two years.10 This highlights the disparity of conservative feasibility between first and third world economic realities.
The feasibility of conservative management relies largely on patients adhering to a follow-up programme. In our study, 50.7% of all patients were lost to follow-up, with the largest numbers being lost in the first year. Factors for poor adherence were not documented in this study and may be interesting research for a future study. We surmise that lack of transport, unaffordability of recurrent visits to hospital, inadequate counselling performed by health care workers, language barriers or fear of missing work could have contributed to the high attrition rate of these patients.
This study did not find any statistically significant relationship between FA occurrence and pregnancy, lactation or oral contraceptive pill use, however, the numbers of these sub-groups are too small for conclusive analysis. Various other studies suggest that pregnancy and lactation results in growth of these lesions, whereas hormone therapy and oral contraceptive use does not change the risk of having these lesions.13-15
Furthermore, the age of the patient, size of the lesion, duration of prior symptomatology did not statistically contribute to the feasibility or failure of conservative management. In a study by Takei et al., it was found that in Japanese women, FAs increase in size more frequently in younger than in older women.16
In this study, the behaviour of these lesions showed marked variability, with 23.1% remaining static in size, 28.1% increasing, 39.2% decreasing, and only 9.6% undergoing complete resolution. This low rate of resolution needs to be interpreted with caution due to the large number of patients lost to follow-up. However, a significant percentage (39.2%) of patients demonstrated a reduction in size of the lesion. It is unknown whether long-term adherence to conservative management follow-up would have resulted in the resolution of more lesions. Complete resolution of FAs in this study was a fifth of that reported by Dent and Cant, who found that 50% of FAs resolved by five years.8
Very few patients were able to comply with the 5-year conservative management period. When coupled with the high numbers lost yearly, this may support shorter conservative management periods. The median follow-up duration in all patients was 18 months. Those in whom conservative management was deemed feasible had a median follow-up of 25 months, but in cases where conservative management had failed, the median follow-up was 16 months.
Our audit revealed that the current policy regarding the management of FAs is not feasible due to high attrition rates for reasons as yet unqualified.
The inability to determine the spontaneous regression rate of FAs and the knowledge that five years of observation appears too long in our setting, invalidates the existing policy. This information has helped us to revise the policy for conservative management of FAs based on a shorter follow-up period of two years (Figure 2).
Based on our results, we recommend a shorter conservative management duration of 24 months, after which surgery should be offered to patients if the lesion is still present. Those with recurrent FAs (to prevent extensive scarring and deformity), FAs diagnosed during pregnancy and highly motivated patients whose lesions are decreasing in size but prefer a longer period of observation can be considered for an extended period of conservative management. The variability in counselling by the health care workers emphasising adherence to a treatment plan may contribute to patient follow-up as well.
Many clinicians question the role of excision of FAs, including in those that enlarge.17 However, in our setting, where patients demonstrate poor health-seeking behaviours, disease presents at an advanced stage and breast cancer is increasingly diagnosed at a younger age,18 we believe there is still a role for excising palpable breast lesions, including FAs. It is imperative that by the age the incidence of breast cancer manifests (mid-third decade), there are no palpable breast lesions, so that any new lesion is viewed with suspicion, prompting the patient to seek medical advice.
Study limitations
A large number of patients were lost to follow-up and this negatively impacted the end-points assessed. Lack of adequate documentation, such as histological data on patients with previous breast lesion excisions and/or assessments and reasons for the large number of patients requesting surgery were also limitations of our study. We are not able to account for the high attrition rate; this limits the validity of our revised protocol as the reasons why patients failed to keep follow-up appointments were not factored in the above algorithm.
Conclusion
In our study, 50.7% of patients with FAs diagnosed on triple assessment and managed conservatively over a 5-year period, were lost to follow-up; 45% of these patients defaulted in the first two years from diagnosis. Conservative management of FAs was therefore feasible in only 26.1% of patients over the 5-year observation period. Although we were unable to identify reasons for the high attrition rate, adherence to conservative management of FAs in suitable patients locally appears to be feasible for only a short period of time. Patients should be offered surgery after a 2-year period of observation. An exception can be made for of a select cohort of patients whose surgery should either be deferred due to pregnancy or are motivated to continue observation for up to 5 years.
This change in management paradigm in order to mitigate the high attrition rate from follow-up clinics has to be balanced against performing unnecessary surgery and placing undue burden on surgical services in an economically constrained society.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
The Breast Unit has obtained class approval for all patients entered into the computerised database (BREC no: BCA173/15). The study was approved by the Biomedical and Research Ethics Committee (BREC) and the University of KwaZulu-Natal (BE004/16).
ORCID
N Barakzai https://orcid.org/0000-0002-4819-1489
E Mansoor https://orcid.org/0000-0002-8958-7703
I Buccimazza https://orcid.org/0000-0002-5399-3101
REFERENCES
1. Houssami N, Cheung M, Dixon JM. Fibroadenoma of the breast. Med J Aust. 2001;174(4):185-8. PMID: 11270760. [ Links ]
2. Onuigbo WI. Adolescent breast masses in Nigerian Igbos. Am J Surg. 1979;137(3):367-8. https://doi.org/10.1016/0002-9610(79)90069-2. [ Links ]
3. Greenberg R, Skornick Y, Kaplan O. Management of breast fibroadenomas. J Gen Intern Med. 1998;13(9):640-5. https://doi.org/10.1046/j.1525-1497.1998.cr188.x. [ Links ]
4. Hughes L, Mansel R, Webster DT. Aberrations of normal development and involution (ANDI) - a new perspective on pathogenesis and nomenclature of benign breast disorders. Lancet. 1987;330(8571):1316-9. https://doi.org/10.1016/s0140-6736(87)91204-9 [ Links ]
5. Al Salamah SM. Do all fibroadenomas need surgical excision? JK Pract. 2006;13:75-7. [ Links ]
6. Wilkinson S, Anderson T, Rifkind E, Chetty U, Forrest AJ. Fibroadenoma of the breast - a follow-up of conservative management. Br J Surg. 1989 Apr;76(4):390-1. https://doi.org/10.1002/bjs.1800760424. PMID: 2720350. [ Links ]
7. Dupont WD, Page DL, Parl FF, et al. Long term risk of breast cancer in women with fibroadenoma. N Engl J Med. 1994;331:10-5. https://doi.org/10.1056/NEJM199407073310103. [ Links ]
8. Dent OM, Cant PJ. Fibroadenoma. World J Surg. 1989;13:706-10. [ Links ]
9. Cant PJ, Madden MV, Close PM, Learmonth GM. Case for conservative management of selected fibroadenoma of the breast. Br J Surg. 1987;74:857-9. https://doi.org/10.1002/bjs.1800740936. PMID: 3664257. [ Links ]
10. Dixon JM, Dobie V, Lamb J, Walsh JS, Chetty U. Assessment of the acceptability of conservative management of fibroadenoma of the breast. Br J Surg. 1996;83(2)1365-2168. https://doi.org/10.1046/j.1365-2168.1996.02105.x [ Links ]
11. Deschenes L, Jacob S, Fabia J, Christen A. Beware of breast fibroadenomas in middle-aged women. Can J Surg. 1985;28(4):372-4. PMID: 2990650. [ Links ]
12. Ciatto S, Bonardi R, Zappa M, Giorgi D. Risk of breast cancer subsequent to histological or clinical diagnosis of fibroadenoma-retrospective longitudinal study of 3938 cases. Ann Oncol. 1997;8(3):297-300. https://doi.org/10.1023/A:1008263522021. [ Links ]
13. Ravnihar B, Segel DG, Lindther J. An epidemiologic study of breast cancer and benign breast neoplasm in relation to the oral contraceptive and estrogen use. Eur J Cancer. 1979;15:395-405. https://doi.org/10.1016/0014-2964(79)90074-4. [ Links ]
14. Canny PF, Berkowitz GS, Kelsey JL. Fibroadenoma and the use of exogenous hormones - a case control study. Am J Epidemiol. 1988;127:454-61. https://doi.org/10.1093/oxfordjournals.aje.a114822. [ Links ]
15. Karagulle E, Turk E, Erinanc OH, Moray G. Giant fibroadenoma growing rapidly during pregnancy. Iran Red Crescent Med J. 2014;16(8)e9531. https://doi.org/10.5812/ircmj.9531. [ Links ]
16. Takei H, Lino Y, Horiguchi J, et al. Natural history of fibroadenomas based on the correlation between size and patient age. Jpn J Clin Oncol. 1999;29(1)8-10. https://doi.org/10.1093/jjco/29.1.8. [ Links ]
17. Klinger K, Bhimani C, Shames J, Sevrukov A. Fibroadenoma - from imaging evaluation to treatment. J Am Osteopath Coll Radiol. 2018;8(2):17-30. https://doi.org/10.1016/j.carj.2010.08.004. [ Links ]
18. Cubasch H, Nietz S, Ruff P, et al. South African Breast Cancer and HIV Outcomes Study: methods and baseline assessment. J Glob Oncol. 2017;3:114-24. [ Links ]
 Correspondence:
Correspondence:
N Barakzai
Email: naziabarakzai@yahoo.com














