Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.59 no.1 Cape Town mar. 2021
http://dx.doi.org/10.17159/2078-5151/2021/v59n1a3400
EMERGENCY SURGERY
Skin-only closure as a temporary abdominal closure technique in a rural setting - exploring role and safety profile
H KrugerI; DG CouchI; GV OosthuizenI, II
INgwelezane General Hospital, South Africa
IIDepartment of Surgery, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: Acute laparotomy for trauma or sepsis often prevents definitive closure due to need for relook laparotomy or to prevent abdominal compartment syndrome. Skin-only closure is widely used in our setting. In this study, we review the safety and effectiveness of this technique
METHODS: Patients presenting with intra-abdominal pathology undergoing acute laparotomy and then subsequent skin-only closure using 2-0 prolene were included in the study and followed postoperatively for a three-month period for adverse events stratified by Clavien-Dindo grading, and rate of definitive closure
RESULTS: During the study period, twenty-five patients underwent emergent laparotomy and skin-only closure. The median age of patients undergoing skin-only closure was 27 years (standard deviation 9.1). Six patients presented with major trauma and 19 presented with sepsis. Twenty-one patients underwent subsequent fascial closure. One patient was unable to undergo fascial closure and was managed as a planned ventral hernia. Fourteen patients developed a postoperative complication. There were no deaths and no readmissions to intensive care. Three further patients developed a ventral hernia
CONCLUSION: Skin-only closure, in carefully selected patients, is a feasible alternative to other temporary abdominal closure techniques in a resource-constrained setting
Keywords: damage control, skin-only closure, temporary abdominal closure, hernia
Background
Acute intra-abdominal sepsis or trauma requiring emergent laparotomy results in diffuse tissue oedema, which increases the risk of developing postoperative abdominal compartment syndrome after fascial closure. This, coupled with the frequent need for relaparotomy after damage control, often calls for a temporary abdominal closure method.1
Multiple techniques in temporary abdominal closure have been described, including Opsite sandwich,23 Bogota bag,4 ABTHERA™,5 and skin-only closure, but there is no single definitive method found to be superior in assisting delayed primary closure despite a wealth of published reports.1
Temporary closure, although helpful in preventing abdominal compartment syndrome and allowing rapid access for further laparotomies, is associated with failure of subsequent fascial closure, ward-evisceration, skin necrosis, and the development of entero-cutaneous fistulas.
Several studies have suggested that skin-only closure, using interrupted or continuous suture, or towel clips, is beneficial for achieving subsequent fascial closure, although should be reserved for more haemodynamically stable patients.6,7 This technique, however, has been reported to have an incidence of ward-evisceration of 5%, skin necrosis of 7%, and entero-cutaneous fistula of 21%, with an overall mortality rate of 44%, and may not be possible in the setting of major tissue oedema predisposing to intra-abdominal hypertension.8 This is in comparison to Bogota bag or Opsite sandwich closure with reported fistula rates below 10%, and a negligible risk of compartment syndrome.9
The main drawback of any of these techniques is a subsequent ventral hernia rate approaching 60%.4 While suction-assisted devices such as the ABTHERATM have reported fistula rates below 3.5%2,10 and subsequent fascial closure rates of up to 90%11, they have limited utility in low-resource rural settings due to cost considerations and often due to limited access to wall suction.
Our centre in KwaZulu-Natal is in a low-resource semi-rural setting. We receive a high burden of severe abdominal sepsis and trauma from 18 referral hospitals serving a population of approximately 3 million. We perform in the region of 250 emergency surgical procedures per month, with damage control laparotomy and subsequent relaparotomy being daily occurrences.
Due to the resource-limited nature of our setting, the use of skin-only closure as a bridge to relaparotomy and definitive delayed fascial closure is widely used. Where possible, skin-only closure is done in preference to Opsite sandwich or Bogota bag closure, as this negates the use of wall suction, controls intra-abdominal secretions, does not require frequent dressing changes, and allows early ambulation. In this study, we sought to review the outcomes of patients undergoing skin-only closure in the emergent setting and to illustrate the safety and pitfalls of this technique.
Material and methods
Due to the observation-of-practice nature of the study, individual informed consent was deemed not necessary by the ethics committee prior to the collection of data. This was a prospectively collected case-note study in a single state-funded hospital in KwaZulu-Natal, South Africa. Patients presenting with intra-abdominal pathology undergoing acute laparotomy and then subsequent skin-only closure were included in the study and followed postoperatively for a three-month period. Data were manually entered into a database detailing information from admission to discharge from hospital. Primary outcome measures were skin necrosis, abdominal compartment syndrome requiring return to theatre for decompression, ward-evisceration, surgical site infection (SSI), number of laparotomies to fascial closure, development of entero-cutaneous fistula and ventral hernia. Inclusion criteria were emergent laparotomy for acute intra-abdominal sepsis or trauma requiring damage control where the operating surgeon felt primary fascial closure was not possible due to the risk of intra-abdominal hypertension or compartment syndrome. In order to avoid including patients with a need for further laparotomy alone without significant tissue oedema which may have biased positive outcomes, patients requiring further laparotomy alone in the absence of tissue oedema were excluded. The skin-only closure for all patients was performed by the operating surgeon using a continuous 2-0 prolene suture secured at either end of the wound with reef knots. The wound was then covered with a single layer, porous non-suction wound dressing. Patients were then taken to the intensive care unit and reviewed at least every 4 hours until relaparotomy or fascial closure.
Results
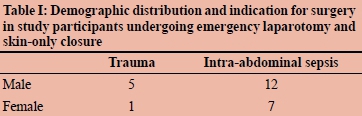
Between 1 April and 1 July 2019, twenty-five patients underwent emergent laparotomy and skin-only closure. The median age of patients undergoing skin-only closure was 27 years (standard deviation 9.1). Table I demonstrates the demographic profile and indications for laparotomy in the study group.
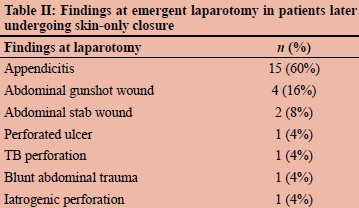
The most common source of intra-abdominal sepsis was ruptured appendicitis (n = 14) followed by perforated peptic ulcer disease, iatrogenic small bowel injury post caesarean section and spontaneous small bowel perforation due to acute tuberculosis (Table II). All patients undergoing laparotomy for intra-abdominal sepsis had 4-quadrant purulent or faecal peritonitis with widespread soiling. Among the trauma laparotomies, four were for trans-axial gunshot wounds, two were for stab wounds with major vascular retroperitoneal injury, and one was for blunt injury with underlying bowel perforation and mesenteric injury. All seven trauma patients had bowel content soiling.
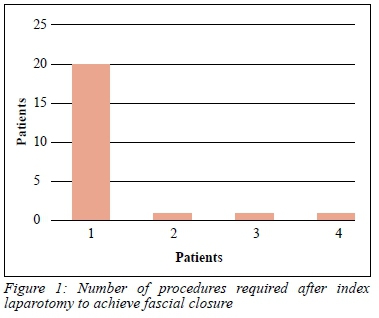
Twenty patients (80%) underwent fascial closure at the first subsequent laparotomy within 48 hours of initial surgery. Four patients underwent more than one re-laparotomy before fascial closure was achieved (Figure 1). In patients without primary closure at the first re-laparotomy, reasons for delayed closure were residual tissue oedema (n = 2) and residual sepsis (n = 1). One patient unfit for further surgery was unable to undergo fascial closure and was managed as a planned ventral hernia, left with definitive skin-only closure.
Complications
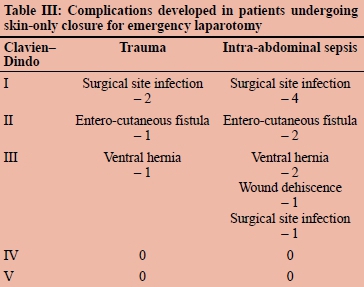
Of the 25 patients undergoing skin-only closure, 14 patients (56%) developed a postoperative complication. There were no deaths and no complications requiring intensive care input. No patients developed skin necrosis or abdominal compartment syndrome. Six patients developed SSI subsequent to fascial closure after four days, which was managed on the ward without significant intervention. One patient developed SSI that required debridement in theatre with subsequent split skin graft. Three patients (12%) developed entero-cutaneous fistulae, all closing without operative intervention but did require total parenteral nutrition during their hospital stay. Three patients developed a ventral hernia within the study period requiring deferred component separation and hernia repair. One patient who was managed as a planned ventral hernia with definitive skin-only closure developed a wound dehiscence (with no evisceration) after 12 weeks, requiring long-term management of an open abdomen without subsequent surgery. Table III tabulates the abovementioned complications, expressed by indication for surgery and Clavien-Dindo classification of complications.
Discussion
Delayed abdominal closure employed to prevent abdominal compartment syndrome and to allow rapid access for planned relaparotomy following a damage control procedure has been reported for many years as an effective bridge to definitive fascial repair where haemodynamic instability, coagulopathy or sepsis prevents immediate closure.12,13
The three most frequently employed techniques include suction-assisted devices such as the hand-made Opsite sandwich or the pre-made ABTHERATM abdominal suction device, Bogota bag-type closure, or skin-only closure. Among the most worrisome complications associated with these techniques are abdominal compartment syndrome requiring decompression, ward-evisceration, skin necrosis, SSI, development of entero-cutaneous fistula, and ventral hernia requiring complex delayed repair.
We employ skin-only closure during our initial laparotomy as temporary closure technique of choice in patients who are deemed to not require large volume fluid resuscitation, therefore being at higher risk of ACS, and in whom the skin can be opposed without undue tension and/or significant elevation of airway pressure whilst completely relaxed under anaesthesia (peak airway pressure below 25 cmH20), and who will require a mandatory relaparotomy. We also employ skin-only closure as a definitive procedure in patients when a planned incisional hernia is necessitated by prolonged inability to close the abdominal fascia. This is outlined in Figure 2.
Abdominal compartment syndrome should be an infrequent occurrence if the chosen temporary closure method has been correctly executed; however, patients should be observed for the development of this condition and returned to theatre for decompression if required. In our series, no patients developed this complication. Similarly, ward-evisceration or skin necrosis may occur with temporary closure methods, for which patients should be promptly returned to theatre for repeat closure. In our study, no patients had ward-evisceration or skin necrosis.
Surgical site infection is a common problem after emergency laparotomy and rates vary between 15% and 25% for intra-abdominal surgery.14 In our group of patients, 28% had SSI, this likely related to the presence of intra-abdominal sepsis at presentation as well as the acute physiological insult from the indication for the laparotomy. Most were managed conservatively, with only one patient needing a repeat procedure related to SSI.
Development of entero-cutaneous fistula in temporary abdominal closure is a common and highly morbid complication resulting in the death of 11% of patients.15 This frequently necessitates the use of total parenteral nutrition, which significantly increases the resources required to achieve discharge from hospital.
The incidence of fistula formation with the use of temporary abdominal closure techniques has been reported as 3.5-20% in suction-assisted devices,5,10,16,17 8-9% in those with Bogota bag closure,18,19 and 14% in skin-only closure.8 In our series, the rate of fistula formation was 12%.
Failure to achieve eventual closure of the rectus sheath requiring subsequent ventral hernia repair, requiring a further inpatient stay and component separation or synthetic mesh, has been reported as 28-29% for vacuum assisted devices,20,21 13-35% for Bogota bag closure18,21 and 48% for skin-only closure.8 Our failure to close rate was 12%.
In our unit we make extensive use of the Opsite sandwich and Bogota bag, with skin-only closure reserved for a select group of patients. As a result of this study, we have refined our indications for the use of skin-only closure, as balanced against the other two methods.
Conclusion
Although our study was small and retrospective in nature, it has shed light on the outcomes of skin-only closure in our unit and has helped us to improve our practice in this regard. Skin-only closure, in carefully selected patients, is a feasible alternative to other temporary abdominal closure techniques, especially in a resource-constrained setting where the likes of ABTHERA™ is not an option and where wall suction is often in short supply. Further work within our research unit is being undertaken to examine outcomes between vacuum-assisted devices, Bogota bag, and skin-only closure.
Ethical approval
Approval for this study was granted by the Biomedical Research Ethics Committee of the University of Kwazulu-Natal (Ref No: BCA027/19).
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
ORCID
H Kruger https://orcid.org/0000-0002-6740-7353
DG Couch https://orcid.org/0000-0002-1535-566X
GV Oosthuizen https://orcïd.org/0000-0001-6898-2969
REFERENCES
1. Boele van Hensbroek P, Wind J, Dijkgraaf MGW, Busch ORC, Goslings JC. Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg. 2009;33(2):199-207. [ Links ]
2. Brock WB, Barker DE, Burns RP. Temporary closure of open abdominal wounds: the vacuum pack. Am Surg. 1995;61(1):30-5. [ Links ]
3. Wilde JM, Loudon MA. Modified Opsite® sandwich for temporary abdominal closure: a non-traumatic experience. Ann R Coll Surg Engl. 2007;89(1):57-61. https://doi.org/10.1308/003588407X155446. [ Links ]
4. Manterola C, Moraga J, Urrutia S. Contained laparostomy with a Bogota bag. Results of case series. Cir Esp. (English Ed.) 2011;89(6):379-85. https://doi.org/10.1016/j.ciresp.2011.01.010. [ Links ]
5. Richter S, Dold S, Doberauer JP, Mai P, Schuld J. Negative pressure wound therapy for the treatment of the open abdomen and incidence of enteral fistulas: a retrospective bicentre analysis. Gastroenterol Res Pract. 2013;2013:730829. https://doi.org/10.1155/2013/730829. [ Links ]
6. Hu P, Uhlich R, Gleason F, Kerby J, Bosarge P. Impact of initial temporary abdominal closure in damage control surgery: a retrospective analysis. World J Emerg Surg. 2018;13:43. https://doi.org/10.1186/s13017-018-0204-3. [ Links ]
7. Huang Q, Li J, Lau W. Techniques for abdominal wall closure after damage control laparotomy: from temporary abdominal closure to early/delayed fascial closure - a review. Gastroenterol Res Pract. 2016;2016:2073260. https://doi.org/10.1155/2016/2073260. [ Links ]
8. Tremblay LN, Feliciano DV, Schmidt J, et al. Skin only or silo closure in the critically ill patient with an open abdomen. Am J Surg. 2001;182(6):670-5. https://doi.org/10.1016/s0002-9610(01)00805-4. [ Links ]
9. Batacchi S, Matano S, Nella A, et al. Vacuum-assisted closure device enhances recovery of critically ill patients following emergency surgical procedures. Crit Care. 2009;13(6):R194. https://doi.org/10.1186/cc8193. [ Links ]
10. Hougaard HT, Ellebaek M, Holst UT, Qvist N. The open abdomen: temporary closure with a modified negative pressure therapy technique. Int Wound J. 2014;11(S1):13-6. https://doi.org/10.1111/iwj.12281. [ Links ]
11. Fitzgerald JEF, Gupta S, Masterson S, Sigurdsson HH. Laparostomy management using the ABThera™ open abdomen negative pressure therapy system in a grade IV open abdomen secondary to acute pancreatitis. Int Wound J. 2013;10(2):138-44. https://doi.org/10.1111/j.1742-481X.2012.00953.x. [ Links ]
12. Lucas CE, Ledgerwood AM. Prospective evaluation of haemostatic techniques for liver injuries. J Trauma. 1976;16(6):442-51. https://doi.org/10.1097/00005373-197606000-00003. [ Links ]
13. Rotondo MF, Schwab CW, McGonigal MD, et al. 'Damage control': an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35(3):375-82. [ Links ]
14. Azoury S, Farrow N, Hu Q, et al. Postoperative abdominal wound infection - epidemiology, risk factors, identification, and management. Chronic Wound Care Management and Research. 2015;2:137-48. https://doi.org/10.2147/CWCMR.S62514. [ Links ]
15. Hollington P, Mawdsley J, Lim W, et al. An 11-year experience of enterocutaneous fistula. Br J Surg. 2004 Dec;91(12):1646-51. https://doi.org/10.1002/bjs.4788. [ Links ]
16. Olona C, Caro A, Duque E, et al. Comparative study of open abdomen treatment: ABThera™ vs. abdominal dressing™. Hernia. 2015;19(2):323-8. https://doi.org/10.1007/s10029-014-1253-5. [ Links ]
17. Atema JJ, Gans SL, Boermeester MA. Systematic review and meta-analysis of the open abdomen and temporary abdominal closure techniques in non-trauma patients. World J Surg. World J Surg. 2015;39(4):912-25. https://doi.org/10.1007/s00268-014-2883-6. [ Links ]
18. Muhammad Y, Gondal KM, Khan UA. Use of the "Bogota bag" for closure of open abdominal wound after exploratory laparotomy-our experience at Mayo Hospital Lahore. J Pak Med Assoc. 2016;66(8):980-3. [ Links ]
19. Kirshtein B, Roy-Shapira A, Lantsberg L, Mizrahi S. Use of the "Bogota bag" for temporary abdominal closure in patients with secondary peritonitis. Am Surg. 2007;73(3):249-52. [ Links ]
20. Stone PA, Hass SM, Flaherty SK, et al. Vacuum-assisted fascial closure for patients with abdominal trauma. J Trauma. 2004;57(5):1082-6. https://doi.org/10.1097/01.ta.0000149248.02598.9e. [ Links ]
21. Kaplan M, Banwell P, Orgill DP, et al. Guidelines for the management of the open abdomen. Wounds-a Compendium of Clinical Research and Practice. 2005 Oct 1:1-24. [ Links ]
 Correspondence:
Correspondence:
DG Couch
Email: couch27@gmail.com














