Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.58 no.4 Cape Town dic. 2020
http://dx.doi.org/10.17159/2078-5151/2020/v58n4a3221
ORIGINAL ARTICLE
Evaluation of views and perceptions of junior doctors on urology training and exposure during internship in South Africa: are we losing future urologists?
S Silolo; Η van Deventer; A van der Merwe
Department of Urology, Faculty of Medicine and Health Sciences, Stellenbosch University, South Africa
ABSTRACT
BACKGROUND: In South Africa, urological and other subspecialty training and exposure vary across each university at undergraduate and internship level. Many students and junior doctors complete their degrees and medical internship with little or no exposure and training to enable them to manage common urological conditions at primary healthcare level with the adequate competency, proficiency and confidence. We aimed to evaluate the exposure and urological training ofjunior doctors during internship and to determine whether it had any impact on their attitudes toward urology as a speciality in which to pursue a career.
METHODS: We used a descriptive cross-sectional survey design. We emailed a questionnaire to 200 community service doctors who completed internship during 2016-2018, working across Western Cape hospitals. The questionnaire aimed to assess their clinical exposure to urology, confidence in basic urological knowledge and clinical skills, and their attitudes toward urology as a postgraduate career choice.
RESULTS: The response rate was 104/200 (52%), 75% (n = 78) of the respondents had completed their internship without rotating through the urology department, 53.8% (n = 56) felt that their knowledge of essential urology topics was 'average' and still required further teaching and guidance, and 43.3% (n = 45) were not confident of performing a circumcision. 11.5% (n = 12) respondents were interested in pursuing a career in urology. The duration of the rotation through urology during internship and pursuing a career in urology were significantly associated (p = 0.005).
CONCLUSION: The study showed that urological exposure and training at internship level is below the standard it needs to be in order to produce proficient and competent doctors able to practise efficiently during community service. The study also highlighted that limited exposure has a negative impact on potential future urologists wanting to pursue a career in the field. Incorporation of necessary urology skills short courses into the internship programme might help mitigate some of these challenges.
Keywords: urology training, urological exposure, urology teaching, medical internship, undergraduate training.
Introduction
In South Africa, urological training and clinical exposure vary across each university at undergraduate and internship level. Because of the shorter duration of clinical rotations in subspecialties, many students and junior doctors complete their degrees and medical internship with limited exposure and training, making them less able to manage common urological conditions at primary healthcare level with adequate proficiency and confidence. This is equally true for most subspeciality departments such as otorhinolaryngology (ENT), ophthalmology, and paediatric surgery. The lack of exposure could affect the future of specialist training of urologists in South Africa as many might see urology as a less attractive career option to pursue.
As from 2005, after concerns were raised about the clinical competencies of intern doctors in specific disciplines, newly qualified junior doctors in South Africa are required to complete a mandatory two years of internship following completion of their undergraduate degree.1 During these two years, they rotate through different clinical departments at four-month rotation intervals, i.e. surgery, obstetrics and gynaecology, internal medicine, paediatrics, and family medicine (including psychiatry) with anaesthetics and orthopaedics split into two-month rotations each.2 Subspecialties such as urology, ENT, plastic surgery and ophthalmology if at all, are incorporated as part of the surgical rotation for a short one- to two-week rotation.
The concern is that many junior doctors complete their internship without the confidence, core skills, and knowledge to be able to manage common basic urological problems.
Previous studies have assessed the South African internship programme and factors influencing the development of practical skills in junior doctors. They concluded that the current programme prepared junior doctors adequately for community service, but it highlighted significant areas of weakness in subspecialties like urology, ENT, and ophthalmology.3,4
In South Africa, research on the training and exposure of junior doctors in urology is lacking. However, minimal exposure to urology in junior doctors and undergraduates is not a problem isolated to South Africa, as evident in a study done in the United Kingdom (UK): 'Perception, career choice and self-efficacy of UK medical students and junior doctors in urology'. Many students reported that the clinical exposure they received was not adequate to be able to increase their confidence in performing basic urological procedures.5
Some studies in the United States highlight that about 15% of junior doctors complete internship without having rotated through urology.6 These statistics are thought to be much higher in South Africa, although currently, no data are available.
The primary aim of this study was to evaluate the views and perceptions of community service doctors on the exposure and urological training during the internship period. Secondary aims were evaluating the attitudes of junior doctors toward pursuing a career in urology.
Methods
We used a descriptive cross-sectional survey design. The target population was the 1 300 post-internship doctors from 2016-2018 employed by the local government to community service medical officer posts in 2019-2020. We aimed to sample the community service doctors placed at various hospitals across the Western Cape. All the community service doctors had done their internships at various hospitals across the country. They were then assigned to community service posts across the country by an online application process.
We used probability sampling through a simple random sampling method where all community service medical officers allocated to posts formed part of the target population. We sampled 200 community service doctors placed across Western Cape hospitals. We predicted a response rate of 65% (allowing for non-responders) would yield a 5% sample error or less with a 95% confidence interval to yield a statistically significant result.
Participants received the questionnaire or a link to the questionnaire via email. The questionnaire was designed to assess their views and perceptions on the urological training and exposure they received during the internship period, and whether it was adequate to prepare them for community service, by gauging their levels of confidence in managing common urological conditions. The questionnaire was designed by the researcher based on general survey design principles,7 internship objectives prescribed in the Health Professions Council of South Africa (HPCSA) internship logbook, and previously administered self-evaluation surveys.
The questionnaire was reviewed and edited by senior urologists with teaching experience. It was then piloted on ten randomly selected medical officers to test its feasibility, and clarity of questions.
The questionnaire aimed to assess the following domains:
• demographics,
• clinical exposure to urology during undergraduate and postgraduate level,
• confidence in basic urology knowledge,
• confidence in core basic urological skills,
• attitudes toward urology as a postgraduate career choice, and
• views and opinions on improvements that can be made to the current model for training interns in urology during the internship period.
Inclusion criteria
• All junior doctors who completed internship from 2016 to 2018.
• All doctors who completed an internship in South Africa.
Exclusion criteria
• Doctors who declined to participate in the study.
• Doctors who completed their undergraduate and internship training outside of South Africa.
• Doctors who were currently in the department of urology as a medical officer or registrar.
• Surveys submitted beyond the deadline for data collection.
The collected data were coded, entered into Excel, cleaned, and exported into IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, N.Y., USA) for analysis. Data were summarised using frequencies and percentages. Association between variables was assessed using the chi-square test. Statistical analysis was done by the support of a Biostatistician from the Division of Epidemiology and Biostatistics.
Results
The response rate was 104/200 (52%) respondents who had trained and completed their internship at various hospitals across South Africa. Of the 104 respondents, 69.2% (n = 72) were female and 30.8% (n = 32) were male. The majority of the respondents (90.4%, n = 94) were between the age of 20-29. The respondents included doctors who had graduated from all nine medical schools in South Africa. Most of the respondents (39.4%, n = 41) felt their overall training in urology was poor or below average, while 29.8% (n = 31) said their overall training was 'average'; only 11.6% (n = 12) felt it was adequate and could practise independently.
Exposure to urology
Of the 104 respondents, more than 64% had completed in-ternship at either a level three tertiary hospital (48.1%, n = 50) or a combined level two and three hospital complex (16.3%, n = 17), while 22.1% (n = 23) and 3.8% (n = 4) completed at a level two (regional) and level one (district) hospital respectively.
Seventy-eight of the respondents (75%) had completed their internship without rotating through the urology department, 13.5% (n = 14) had rotated through urology for four weeks or more during internship, and 8.7% (n = 9) rotated for two weeks (Figure 1).

Of the 104 respondents, 84.6% (n = 88) felt a rotation in urology should be mandatory for all interns during internship.
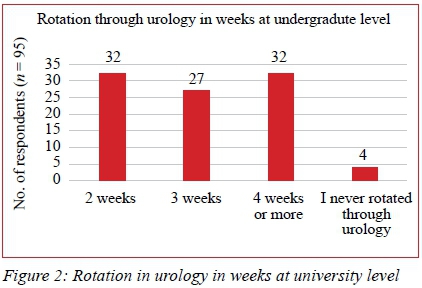
At the undergraduate level (n = 95), 33.7% (n = 32) rotated for more than four weeks, 28.4% (n = 27) rotated for three weeks, and 4.2% (n = 4) had never rotated through urology (Figure 2).
Basic urology knowledge
More than half of the respondents (53.8%, n = 56) felt that their knowledge of essential urology topics was 'average' and still required further guidance from seniors. A total of 20.2% (n = 21) felt that their knowledge was poor or below average and knew very little about urology; 26% (n = 27) felt they had gained adequate knowledge and could practise independently (Figure 3).
Basic urological skills
Most of the participants felt they were not confident enough to perform various basic urological procedures. Of the 104 respondents, 48.1% (n = 50) were not confident in performing suprapubic catheterisations, 25% (n = 26) were confident in performing suprapubic catheterisations alone, while 26.9% (n = 28) felt confident with senior supervision around.
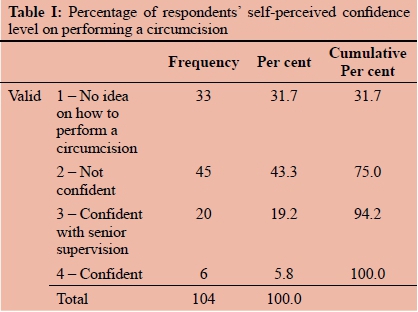
With regards to performing an uncomplicated circumcision, 43.3% (n = 45) were not confident of performing a circumcision, while 31.7% (n = 33) had no idea on how to perform a circumcision, only 5.8% (n = 6) felt confident of performing the procedure alone; 19.2% were confident only if senior supervision is around to assist (Table I).
The only procedure respondents felt comfortable to perform was transurethral catheterisation, with more than 95% (n = 100) confident in performing the procedure.
Of the 104 respondents, 25% (n = 26) felt confident in managing common urological emergencies such as paraphimosis, priapism or renal colic, when 'on-call', 33.7% (n = 35) felt they needed senior supervision, while 41.3% (n = 43) felt that they were 'not confident' in managing some of the emergencies.
Career prospects
Urology was not viewed as an appealing career speciality by 58.7% (n = 61), as they stated they had no interest in pursuing a career in urology. Twelve respondents (11.5%) were interested in specialising in urology, and 29.8% (n = 31) were undecided. Of the respondents not interested in a career path in urology, 12.5% (n = 13) sighted 'lack of exposure' as their reason for not wanting to specialise in urology, and 41.3% (n = 43) were interested in other departments.
Investigating associations
A statistically significant association was found between the hospital level of training during internship and the confidence to perform suprapubic catheterisation (p = 0.005). No other statistically significant associations were found between the perceived quality of urological training during internship (as measured by the hospital level of training during internship) and the confidence levels in basic urological core skills and knowledge, including current knowledge and understanding of basic urology topics, confidence in the ability to perform a transurethral catheterisation, confidence in the ability to perform an uncomplicated circumcision, and confidence in the ability to manage common urological emergencies. The hospital level of training during internship was not significantly associated with pursuing a career in urology.
The association between the duration of the rotation through urology during internship and pursuing a career in urology was statistically significant (p = 0.005).
There were no significant associations between the duration of rotation through urology during internship and the confidence levels in basic urological core skills and knowledge, including current knowledge and understanding of basic urology topics, confidence in the ability to perform a transurethral catheterisation, confidence in the ability to perform suprapubic catheterisation, confidence in the ability to perform an uncomplicated circumcision, and confidence in the ability to manage common urological emergencies.
Discussion
Community service doctors in South Africa are often placed to work in level one and level two hospitals (district and regional hospitals) where they are the proverbial first-hand in the hospital chain system. They often encounter a vast spectrum of medical conditions in an acute setting and are tasked with the acute management of these conditions and referral to the relevant department if necessary.8
Patients with urological pathology are prevalent in district hospitals. These patients often present with a range of symptoms and conditions, some of which have similar clinical presentations, so they need to have basic urology knowledge in order to recognise and manage these patients competently and efficiently in an acute setting and be able to identify cases that warrant urgent referral to a tertiary institution for intervention.
Exposure to urology
This study has highlighted the lack of exposure that junior doctors receive during their training, as 75% (n = 78) stated that they completed internship without having rotated through urology. Of the total participants, 20.2% (n = 21) felt that their basic urology knowledge was below average and knew very little about urology. This is of concern given that most of these doctors will often be placed in rural hospitals with little or no supervision from senior practitioners and will be expected to treat and manage common urological problems with very little knowledge and skill to be able to provide competent primary care.9
In South Africa, there is no uniform syllabus at undergraduate level across all the medical schools; it varies across each institution. This was evident in our study in the disparity in duration of rotations in urology at undergraduate level as seen in Figure 2, where 33.7% of the respondents received two-week rotations while another 33.7% had four-week rotations. Perhaps developing a standardised syllabus and a minimum duration of clinical rotations for all medical schools would help improve urological teaching and exposure at undergraduate level.
Most of the respondents felt that urology should be made a mandatory rotation to all interns during internship. This shows the willingness and desire of junior doctors to be trained in necessary urological skills and topics in order to better prepare them for community service. The challenge is finding suitable and adequate space in an already full two-year rotation. Introducing 'urological basic skills short courses' during surgical rotations might be an alternative solution to this. This study showed that most junior doctors (82.7%) were amenable to this idea, as most of the respondents agreed that urology basic skills short courses should be implemented during their surgical rotations. Many studies have shown that basic skills courses have a positive impact on the knowledge and confidence of junior doctors with regards to practical urology skills.5,10 One study in the UK also demonstrated an increased desire among junior doctors to specialise in urology after having been exposed to and attending urology skills courses.11
Confidence in performing procedures
Encouraging to note was that 96% of the respondents felt confident in being able to perform transurethral catheter-isation, which is a skill taught at undergraduate level (96% of the respondents had been exposed to urology at this level). It is also a skill they are exposed to and use in every department they rotate through during internship.
What was alarming to note in this study was that 43.5% (n = 45) were not confident in performing an uncomplicated circumcision, while a further 31.7% (n = 33) felt they had 'no idea' on how to perform a circumcision. These results are of concern because South Africa has the highest HIV epidemic in the world, and one of the many ways government has identified to try and stem the vast spread of this disease is through the introduction of voluntary male medical circumcision (VMMC) services. These services are offered at primary healthcare level because it has been proven to reduce the risk of HIV transmission.12-14
If community service doctors working at these rural primary healthcare facilities are not competent in performing such procedures early on, this is most likely going to have a negative impact on programmes such as VMMC and the HIV statistics in the country.
This study also noted that 41.3% (n = 43) of respondents were not confident in managing common urological emergencies when on call. Combining little knowledge of essential urology and lack of senior staffing and supervision at rural and district hospitals, community service doctors felt that they were not confident enough to manage these patient s adequately. Inadvertently, this is a catalyst for several potential medico-legal and clinical governance issues, as sometimes urological emergencies can go unrecognised with severe morbidity and mortality, e.g. renal calculi leading to obstruction and eventual end-stage renal failure.
Career prospects
We aimed to investigate the relationship between the exposure to urology and wanting to specialise in urology. According to our results, the duration of the rotation through urology during internship and pursuing a career in urology were significantly associated (p = 0.005). The respondents who rotated longer through urology, and as a result had more exposure, were more likely to choose urology for specialisation. Those who never rotated through urology were less likely to choose a career path in urology. One of the respondents noted that she 'had always been interested in urology but received far too little exposure at both undergraduate and internship level'.
This shows that the interest to specialise in urology is there, and perhaps young doctors are being deprived of an opportunity to gain first-hand experience in the department that interests them,just as they do with the more conventional departments such as paediatrics, general surgery and internal medicine.
According to the Health Professions Council of South Africa (HPCSA) registry statistics, South Africa has 303 urologists registered with the council, servicing a population of 58.78 million.15,16 This equates to a urologist to population ratio of 0.51 per 100 000. This number is very low compared to other countries like the United States of America (USA), with 11 990 urologists (3.72 per 100 000 population),17 and Canada, with 716 urologists (1.9 urologists per 100 000 population).18 Although the decision to pursue a career in any department or subspecialty is multi-factorial, early exposure and training in urology can help junior doctors widen their prospective career choice options and potentially consider pursuing a career in urology - and thus help increase the number of urologists in the country. Table II represents the urologist density per 100 000 population of five countries, including South Africa, the USA, Canada, the UK and Australia.19

Limitations
The study reflected the subjective views of junior doctors and not objective findings and, as such, might have given room for bias. Response bias is a common factor in self-administered surveys, in which some participants might want to represent themselves in a positive light and tend to give responses which they perceive to be socially desirable.20 The response rate of 52% was lower than expected, possibly owing to the impersonal nature of the emailed surveys.
Another possible contributing factor to the low response rate was that we relied on email addresses received from the provincial health department database, as we encountered difficulty in contacting each different hospital to cross reference with the current working email addresses doctors were using at the time of data collection.
Another limitation was the small sample size because of the difficulty we encountered in obtaining authorisation, information, and distribution of the survey in each province. This was diffused by including doctors who did their internship across all hospitals around South Africa and had graduated from all nine medical schools in the country. Although each university was represented, the small sample size meant that there was a disparity in the distribution of representation by undergraduate university in the sample. This made it difficult to observe any significant associations between university of study and outcomes in urological training. A larger sample size can help mitigate this. Given the results seen even in this small target population, it justifies the need for a more extensive study nationally, in order to improve the validity of the results.
Conclusion
This study has highlighted the need for training and exposure of junior doctors in clinical urology. Early implementation of urological outreach programmes at district level hospitals to provide clinical support and training ofjunior doctors will help improve confidence and clinical acumen when managing urological patients. Incorporation of a basic urological skills course into the current internship programme would be one way to increase exposure and training to improve junior doctors' professional development and clinical skills. This will aid them in managing basic urological conditions and thus positively affect their confidence levels in performing specific procedures.21
Acknowledgements
We acknowledge B. Ayele, Biostatistician at the Division of Epidemiology and Biostatistics, Stellenbosch University who assisted with the data analysis and interpretation of this project. We also acknowledge Luzuko Magula, Abongile Jojo and Nasiphi Ndum-Ndum for the help and support throughout this project.
Conflict of interest
There is no conflict of interest to declare by all authors.
Funding source
No external funding was received for this project
Ethical approval
Ethics approval was received from the Health Research Ethics Committee under the Ref: S18/08/158. Permission to commence the study was also obtained from the Western Cape Department of Health.
ORCID
S Silolo https://orcid.org/0000-0002-7051-3800
Η van Deventer https://orcid/org/0000-0001-7472-1773
A van der Merwe https://orcid/org/0000-0002-2006-8331
REFERENCES
1. Meintjes Y. The 2-year internship training. S Afr Med J. 2003;93(5):336-7. [ Links ]
2. HPCSA. Medical and Dental Professions Board, Health Professions Council of South Africa, Handbook on internship training guidelines for interns, accredited facilities and health authorities. 2017 ed. 2017. p. 3-42. [ Links ]
3. Nkabinde TC, Ross A, Reid S, Nkwanyana NM. Internship training adequately prepares South African medical graduates for community service - with exceptions. S Afr Med J. 2013;103(12):930-4. [ Links ]
4. Jaschinski J, De Villiers M. Factors influencing the development of practical skills of interns working in regional hospitals of the Western Cape province of South Africa. SA Fam Pr. 2008;50(1):70-70d. [ Links ]
5. Jones P, Rai BP, Qazi HAR, Somani BK, Nabi G. Perception, career choice and self-efficacy of UK medical students and junior doctors in urology. Can Urol Assoc J. 2015;9(9-10):E573-8. [ Links ]
6. Benson GS. The decline of urological education in United States medical schools. J Urol. 1994 Jul;152(1):169-70. [ Links ]
7. Krosnick JA. Survey research. Annu Rev Psychol. 1999;50:537-67. [ Links ]
8. Reid SJ, Chabikuli N, Jaques PH, Fehrsen GS. The procedural skills of rural hospital doctors. S Afr Med J. 1999;89:769-74. [ Links ]
9. Bola S, Trollip E, Parkinson F. The state of South African internships: a national survey against HPCSA guidelines. S Afr Med J. 2015;105(7):535-9. [ Links ]
10. Auvert B, Taljaard D, Lagarde E, et al. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. Plos Med. 2005;2(11):1112-22. [ Links ]
11. Epidemic transition metrics. 2010;2010. [ Links ]
12. Luk ACO, Mcconnell T. Urology teaching and exposure in foundation training and medical school: is it enough? Eur Urol Suppl. 2019;16(3):e1254-5. [ Links ]
13. Browne C, Norton S, Nolan JM, et al. The impact of a structured clinical training course on interns' self-reported confidence with core clinical urology skills. Ir J Med Sci. 2018;187:255-60. [ Links ]
14. WHO/UNAIDS. New data on male circumcision and HIV prevention: policy and programme implications. [ Links ]
15. HPCSA. HPCSA iRegister [Internet]. 2020. Available from: http://isystems.hpcsa.co.za/iregister/. [ Links ]
16. Stats SA. Mid-year population estimates. 2019. [ Links ]
17. American Urological Association. The state of the urology workforce and practice in the United States. 2019. [ Links ]
18. Canadian Medical Association. Urology Profile. 2018. [ Links ]
19. Naik R, Mandal I, Hampson A, Casey R, Vasdev N. A comparison of urology training across five major English-speaking countries. Curr Urol. 2020;14(1):14-21. [ Links ]
20. Mazor KM, Clauser BE, Field T, Yood RA, Gurwitz JH. A demonstration of the impact of response bias on the results of patient satisfaction surveys. Health Serv Res. 2002;37(5):1403-17. [ Links ]
21. Biyani CS, Hanchanale V, Rajpal S, et al. First urology simulation boot camp in the United Kingdom. African J Urol. 2017;23(3):258-67. [ Links ]
 Correspondence:
Correspondence:
email: sisekosilolo@gmail.com














