Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.58 n.4 Cape Town Dec. 2020
http://dx.doi.org/10.17159/2078-5151/2020/v58n4a3153
TRAUMA
A comparison of blunt and penetrating pancreatic trauma
JJP BuitendagI; VY KongII, III; GL LaingII; JL BruceII; V ManchevII; DL ClarkeII, III
IDepartment of Surgery, Tygerberg Hospital, Stellenbosch University, South Africa
IIDepartment of Surgery, Pietermaritzburg Hospital Complex, University of KwaZulu-Natal, South Africa
IIIDepartment of Surgery, University of the Witwatersrand, South Africa
ABSTRACT
BACKGROUND: This project reviews our experience with managing pancreatic trauma from 2012 to 2018.
METHODS: All patients over the age of 15 years with a pancreatic injury during the period December 2012-December 2018 were retrieved from the Hybrid Electronic Medical Registry at Grey's Hospital and reviewed.
RESULTS: During the study period 161 patients sustained a pancreatic injury. The mechanism of trauma was penetrating in 86 patients (53%) and blunt in 75 (47%). The blunt mechanisms included MVA in 27, PVA in 15, falls in four and assaults in the remaining 29. There were 52 stab wounds and 34 gunshot wounds of the pancreas. A total of 26 patients (16%) were shocked on presentation with a systolic blood pressure of 90 mm Hg or less. The median injury severity score was 16. There were 90 patients with American Association for the Surgery of Trauma (AAST) grade I injury to the pancreas, 36 AAST grade II, 27 AAST grade III, 7 AAST grade IV and a single AAST grade V Fifty-four patients (34%) were initially treated non-operatively of which three eventually required surgery. Of the patients who required surgery, 26 (16%) underwent a distal pancreatectomy. The remainder simply underwent pancreatic drainage. The overall mortality rate was 13% (21/161). The operative mortality was 11% (18/161). Thirteen patients (8%) with penetrating injuries and eight patients (5%) with blunt injuries died. Of the 21 patients who died, 14 had multiple injuries. Five patients died due to overwhelming sepsis. One patient died due to hypovolemic shock and another due to a traumatic brain injury.
CONCLUSION: Our centre not infrequently deals with pancreatic trauma secondary to both blunt and penetrating trauma. We follow the general principles outlined in the literature. Despite this, pancreatic trauma is still associated with significant morbidity and mortality
Keywords: trauma, blunt, penetrating, pancreas
Introduction
Pancreatic trauma is relatively rare but is associated with significant morbidity and mortality.1-10 The management of pancreatic trauma is complex. The management principles and strategies have evolved over the last half century in tandem with the improved understanding of how the physiological impact of trauma on the patient influences the operative approach, as well as with advances in imaging, endoscopic techniques, postoperative care and nutritional support.11-15 Randomised controlled trials are not feasible for this condition and most evidence is derived from large case series and clinical audits. In this regard, SouthAfrica has made significant contributions to the literature on the topic, and ongoing clinical audits will be necessary to keep evaluating these evolving management strategies.1-3 The trend in all the major series over the last fifty years has been away from complex operative strategies towards a more conservative approach.1-10 The Pietermaritzburg Metropolitan Trauma Service (PMTS) maintains a prospectively entered electronic surgical registry, which has allowed us to accumulate large patient cohorts over a prolonged period. This study audits a six-year experience with pancreatic trauma and attempts to analyse our management strategies and outcomes and to contextualise them within our own environment and the broader national and international setting.
Methods
Patients over the age of 15 years who presented with a pancreatic injury between December 2012 and December 2018 were retrieved from the Hybrid Electronic Medical Registry (HEMR). Their demographics, physiology on presentation and clinical management and outcome were documented. All injuries were graded using the American Association for the Surgery of Trauma (AAST) pancreas module for the grading of injuries, the injury severity score (ISS), and the abbreviated injury score (AIS)-abdomen and AIS-chest. Complications were classified as pancreas related or non-pancreas related and graded according to the Clavien-Dindo system.16 External fistulae and intra-abdominal collections were considered to be pancreas related complications.
Statistical methods
Statistical analyses were performed using STATA 15.0©. Continuous variables were compared using unpaired t-test, and categorical variables were compared using chi-squared analysis. Further stepwise and multiple logistic regression analyses was performed. Comparison of presenting physiological parameters between penetrating and blunt pancreatic injuries were performed using unpaired t-test. Chi-squared test was used to compare the proportions of visceral injuries between the two groups and to assess other categorical variables between groups, including injury mechanism and mortality.
Results
Over the six-year period, 161 patients sustained a pancreatic injury. There were 141 (88%) males and the mean age was 31 years. There was a total of 86 (53%) penetrating and 75 (47%) blunt injuries (Table I). There were 90 patients with AAST grade I injuries, 36 with grade II, 27 with grade III, seven with grade IV and a single AAST grade V injury. In 51 patients who were managed non-operatively, the injury was graded exclusively by CT scan; in 18 patients who had a CT prior to surgery, both CT and surgery were used to grade the injury; and in 92 patients who underwent surgery without prior imaging, the grading was exclusively surgical. CT and operative grading were largely concordant with the AAST score being the same in the 16 patients who underwent imaging prior to operation.

The median ISS was 16. Associated injuries are summarised in Table II. There were 121 other intra-abdominal injuries. The stomach was the most frequently damaged other organ (n = 91), followed by the spleen (40), the liver and the small bowel (29). Figure 1 shows the proportions of associated intra-abdominal injuries according to mechanism. The majority of associated hollow viscus injuries occurred with penetrating trauma and the majority of solid organ injuries with blunt trauma.
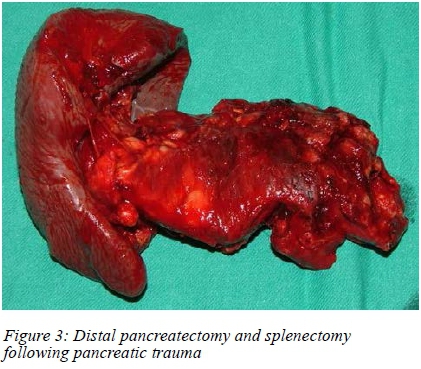
A total of 54 (34%) patients were initially treated non-operatively. Three failed non-operative management (NOM) and required surgery of which two patients demised. The two patients who demised sustained blunt trauma and both were delayed referrals. The injuries which precipitated the need for surgery were not pancreatic related. Of the 110 patients who ultimately required surgery, 25 (16%) underwent a left pancreatic resection (1) a pancreaticoduodenectomy and the remainder (84) underwent pancreatic drainage.
Morbidity compared to AAST grade of pancreatic injury
A total of 92 morbidities were documented of which 39 were pancreatic related.
• The 90 patients with AAST grade I injury to the pancreas developed 51 complications. These included acute kidney injury (AKI) (n = 13), intra-abdominal collections (n = 13), hospital acquired pneumonia (n = 10), wound sepsis (1), cardiac event (1) and neurological events (1).
• The 36 patients with AAST grade II injuries, developed 20 complications which included intra-abdominal collections (9), AKI (4), hospital acquired pneumonia (4), acute cardiac events (4), wound complications (1) and neurological events (1).
• The 27 patients who sustained AAST III injuries, developed 16 complications. These included intra-abdominal collections (7), AKI (2), hospital acquired pneumonia (2), and wound related complications (4).
• The seven patients with AAST IV injuries developed four complications during admission. These included intra-abdominal collections (2) and major wound related complications (2).
• The single patient who sustained an AAST V injury developed an anastomotic leak. According to the Clavien-Dindo classification of morbidity,16 30 patients had grade 1 complications, 31 patients grade 2, two patients grade 3a, eight patients grade 4, five patients grade 4a, three patients grade 4b and 21 patients grade 5.
The median hospital stay for penetrating injuries was nine days with a range of 51 days. For blunt injuries it was five days with a range of 47 days. A total of 27 patients in the penetrating group and 18 patients in the blunt group were admitted to ICU. The median ICU stay for penetrating injuries was four days with a range of 19 days and for blunt injuries six days with a range of 26 days.
The overall mortality rate was 13% (21/161). The operative mortality was 18/110 (16%). Thirteen patients (8%) with penetrating injuries died and eight patients (5%) with blunt injuries died. In the group who required pancreatic resection the mortality rate was 30% (8/26), of which six had penetrating and two blunt trauma. In the drainage group mortality was 12% (10/84). In the initial NOM group the mortality rate was 2/54 (0.4%), Both deaths sustained blunt trauma and experienced a delay in referral. Of the 21 patients who demised, 14 had multiple injuries. Five patients passed away due to overwhelming sepsis. A single patient passed away due to hypovolemic shock and another due to a traumatic brain injury.
Discussion
The pancreas is a retroperitoneal structure and is relatively protected. Thus, either considerable blunt force or penetrating trauma is required to injure it.15 Isolated pancreatic trauma is relatively rare as shown by the high median ISS score and a significant number of associated intra-abdominal and extra-abdominal injuries in patients in this series. Penetrating and blunt pancreatic trauma have different patterns of injury and hence different management strategies.15-18
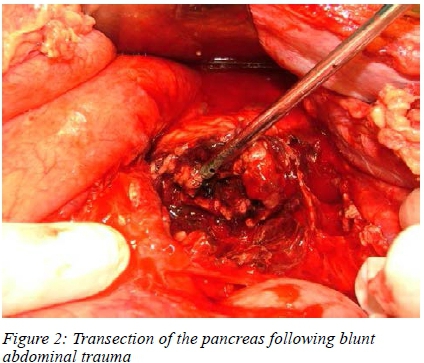
Blunt pancreatic trauma is often associated with delay in recognition. Increased use of imaging may help reduce the delay in diagnosis associated with blunt pancreatic trauma. CT scan has a sensitivity of 80% for identifying a pancreatic injury.2,10,14 There is good correlation between CT and operative grading of pancreatic injury following blunt trauma. Abdominal CT remains the investigation of choice for the diagnosis and grading of blunt pancreatic injury. Minor grades of pancreatic injury may be treated non-operatively. This may require endoscopic intervention in select cases.13,14 High grade injuries with ductal disruption require definitive management. If such an injury is demonstrated at operation, distal pancreatectomy is usually indicated. In select cases a pancreaticogastrostomy may allow for preservation of the distal pancreas.2,4-6,10,14
Penetrating trauma to the pancreas is more frequently associated with hollow visceral injury, and most of these patients require urgent operative management.19-21 These patients are managed according to the grade of injury and physiological concerns dictate the approach.13,19-23 Major resections must be eschewed in the acute setting in lieu of controlling bleeding and soiling and establishing external drainage. Abbreviated laparotomy is usually indicated, and once the patient's physiology has been restored, definitive management is performed at a second operation. At repeat operation the pancreatic injury is managed on its merits. Major resection is only indicated for high grade injuries and this must only be done once the patient's physiology has been restored. This should usually be undertaken in conjunction with experienced hepato-biliary surgeons.23 For low grade injuries a conservative approach involving external drainage is usually adopted. Pancreatic trauma is associated with significant morbidity. Up to one third of all morbidities are directly related to the pancreatic injury. Pancreatic related morbidity includes intra-abdominal collections, pancreatic fistulae and wound sepsis. The remainder of the morbidities are secondary to concomitant injuries.8,10,16,21 The mortality rate remains significant and is related to the need for operation and the complexity of the operative procedure. Patients requiring a resection had a much higher mortality rate (30%) compared to a rate of 12% in the drainage group and of 2% in the non-operative group. The majority of these patients demised secondary to multiple concurrent injuries and not due to the pancreatic injury or the related complications. Only one patient demised secondary to sepsis related complications. In the non-operative group, the mortality was mostly secondary to extra-abdominal injuries. In general, death is usually secondary to massive bleeding, ongoing sepsis or to the overall magnitude of the trauma.
Conclusion
Our centre not infrequently deals with pancreatic trauma secondary to both blunt and penetrating trauma. We follow the general principles outlined in the literature. Despite this, pancreatic trauma is still associated with significant morbidity and mortality.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Ethics approval for the maintenance of this registry was provided by the Biomedical Research Ethics Committee (BREC) (reference: BE 207/09 and BCA 221/13).
ORCID
JJP Buitendag https://orcid.org/0000-0001-7169-129X
GL Laing https://orcid.org/0000-0001-8075-0386
JL Bruce https://orcid.org/0000-0001-8666-4104
V Manchev https://orcid.org/0000-0001-9152-0092
DL Clarke https://orcid.org/0000-0002-6954-153X
REFERENCES
1. Krige JE, Kotze UK, Setshedi M, et al. Surgical management and outcomes of combined pancreaticoduodenal injuries: analysis of 75 consecutive cases. J Am Coll Surg. 2016;222(5):737-49. https://doi.org/10.1016/jjamcollsurg.2016.02.005. [ Links ]
2. Boffard KD, Brooks AJ. Pancreatic trauma - injuries to the pancreas and pancreatic duct. Eur J Surg. 2000;166:4-12. [ Links ]
3. Farrell RJ, Krige JE, Bornman PC, Knottenbelt JD, Terblanche J. Operative strategies in pancreatic trauma. Br J Surg. 1996;83(7):934-7. [ Links ]
4. Krige JE, Thomson SR. Operative strategies in pancreatic trauma - keep it safe and simple. S Afr J Surg. 2011;49(3):106-9. [ Links ]
5. Yilmaz TH, Hauer TJ, Smith MD, et al. Operative techniques in pancreatic trauma - a heuristic approach. Injury. 2013;44(1):153-5. https://doi.org/10.1016/jinjuiy.2012.09.020. Epub 2012 Oct 24. [ Links ]
6. Degiannis E, Glapa M, Loukogeorgakis SP, Smith MD. Management of pancreatic trauma. Injury. 2008;39(1):21-9. [ Links ]
7. Krige JE, Kotze UK, Setshedi M, et al. Prognostic factors, morbidity and mortality in pancreatic trauma: a critical appraisal of432 consecutive patients treated at a level 1 trauma centre. Injury. 2015;46(5):830-6. https://doi.org/10.1016/j.in.iur\.2015.01.032. [ Links ]
8. Krige JE, Kotze UK, Nicol AJ, Navsaria PH. Isolated pancreatic injuries: an analysis of 49 consecutive patients treated at a level 1 trauma centre. J Visc Surg. 2015;152(6):349-55. https://doi.org/10.1016/jjviscsurg.2015.09.010. Epub 2015 Oct 23. [ Links ]
9. Krige JE, Kotze UK, Nicol AJ, Navsaria PH. Morbidity and mortality after distal pancreatectomy for trauma: a critical appraisal of 107 consecutive patients undergoing resection at a level 1 trauma centre. Injury. 2014;45(9):1401-8. https://doi.org/10.1016/j.injury.2014.04.024. Epub 2014 Apr 16. [ Links ]
10. Krige J, Kotze U, Nicol A, Navsaria P. Isolated injury to the pancreas: the importance of the baseline computed tomography scan. J Visc Surg. 2016;153(3):239. https://doi.org/10.1016/j.jviscsurg.2016.03.001. [ Links ]
11. Krige JE, Spence RT, Navsaria PH, Nicol AJ. Development and validation of a pancreatic injury mortality score (PIMS) based on 473 consecutive patients treated at a level 1 trauma center. Pancreatology. 2017;17(4):592-598. https://doi.org/10.1016/j.pan.2017.04.009. [ Links ]
12. Krige JEJ, Kotze UK, Setshedi M, Nicol AJ, Navsaria PH. Management of pancreatic injuries during damage control surgery: an observational outcomes analysis of 79 patients treated at an academic level 1 trauma centre. Eur J Trauma Emerg Surg. 2017;43(3):411-20. https://doi.org/10.1007/s00068-016-0657-6. [ Links ]
13. Krige JEJ, Kotze UK, Navsaria PH, Nicol AJ. Endoscopic and operative treatment of delayed complications after pancreatic trauma: an analysis of 27 civilians treated in an academic level 1 trauma centre. Pancreatology. 2015;15(5):563-9. https://doi.org/10.1016/j.pan.2015.06.008. [ Links ]
14. Buccimazza I, Thomson SR, Anderson F, et al. Isolated main pancreatic duct injuries spectrum and management. Am J Surg 2006;191:448-52. [ Links ]
15. Krige JE, Kotze UK, Sayed R, et al. An analysis of predictors of morbidity after stab wounds of the pancreas in 78 consecutive injuries. Ann R Coll Surg Engl. 2014;96(6):427-33. https://doi.org/10.1308/003588414X13946184901849. [ Links ]
16. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205-13. https://doi.org/10.1097/01.sla.0000133083.54934.ae [ Links ]
17. Degiannis E, Levy RD, Potokar T, et al. Distal pancreatectomy for gunshot injuries of the distal pancreas. Br J Surg. 1995;82:1240-2. [ Links ]
18. Chinnery GE, Krige JE, Kotze UK, et al. Surgical management and outcome of civilian gunshot injuries to the pancreas. Br J Surg. 2012;99(Suppl 1):140-8. https://doi.org/10.1002/bjs.7761. [ Links ]
19. Krige JE, Navsaria PH, Nicol AJ. Damage control laparotomy and delayed pancreatoduodenectomy for complex combined pancreatoduodenal and venous injuries. Eur J Trauma Emerg Surg. 2016;42(2):225-30. https://doi.org/10.1007/s00068-015-0525-9. [ Links ]
20. Krige JE, Beningfield SJ, Nicol AJ, Navsaria P. The management of complex pancreatic injuries. S Afr J Surg. 2005;43(3):92-102. [ Links ]
21. Krige J, Nicol A, Navsaria P. Managing grade 5 pancreatic injuries - think smart, act smart, and call in the pancreatic cavalry early. J Trauma Acute Care Surg. 2017;82(6):1187-8. https://doi.org/10.1097/TA.0000000000001459. [ Links ]
22. Krige JE, Jonas E, Thomson SR, et al. Resection of complex pancreatic injuries: benchmarking postoperative complications using the Accordion classification. World J Gastrointest Surg. 2017;9(3):82-91. https://doi.org/10.4240/wjgs.v9.i3.82. [ Links ]
23. Krige J, Nicol A, Navsaria P. Treating complex pancreatic injuries. Trauma and pancreatic surgeons working together is the modern management paradigm. J Visc Surg. 2017;154(2):143. https://doi.org/10.1016/jjviscsurg.2017.02.002. [ Links ]
 Correspondence:
Correspondence:
email: damianclar@gmail.com














