Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.58 n.4 Cape Town Dec. 2020
http://dx.doi.org/10.17159/2078-5151/2020/v58n4a3276
ORIGINAL ARTICLE
Do upper GI bleed guidelines reach patient care: effect of a quality improvement initiative
S RayamajhiI, II, III; I AborkisIII; C KloppersI, II, III; R SpenceIII; SR ThomsonIII, IV
IAcute Care Surgery, Groote Schuur Hospital, South Africa
IIDepartment of Surgery, Groote Schuur Hospital, South Africa
IIIFaculty of Health Sciences, University of Cape Town, South Africa
IVMedical Gastro-enterology, Groote Schuur Hospital, South Africa
ABSTRACT
BACKGROUND: Adherence is variable in clinical practice to consensus guidelines on the management of upper gastrointestinal bleeding. We aimed to assess the effect of a quality improvement program (QIP) on guideline adherence.
METHODS: A QIP was undertaken over a two-month period. Data were collected retrospectively, for the one-year pre QIP and prospectively for one-year post QIP. The QIP goals were adherence to criteria for the timing of oesophago-gastroduodenoscopy (OGD), achievement of dual endotherapy and blood transfusion triggers.
RESULTS: Fifty-one patients were pre QIP and 58 post QIP. The two groups' baseline data were comparable. Over 80% had their OGD within 24 hours (pre QIP 82.3%, post QIP 81.0%). The overall and high-risk groups (variceal and MBS > 10) had an insignificantly longer time to OGD (mean 19.2 and 17.8 hours respectively) in the post QIP cohort (mean 14.2 and 15.2 hours).The practice of dual endotherapy improved post QIP (p = 0.02) for non-variceal bleeding. The Hb g/dL (mean + SD) in stable patients who were transfused was significantly different pre QIP (6.3 + 2) and post QIP (5.7 + 1.69) (p = 0.04). Twelve patients (23.5%) were transfused for Hb above 7 g/dl pre QiP and six (10.3%) post QIP (p = 0.047). Thirty-day mortality rate was 9.8% (pre QIP) and 10.3% (post QIP). Univariate analysis showed that Grade III shock was the only significant factor in determining 30-day mortality.
CONCLUSION: This QIP had no effect on time to OGD adherence which compares favorably to similar audits. Adherence to transfusion triggers and the ability to deliver dual endotherapy routinely were positive QIP outcomes.
Keywords: upper GI bleed, guideline compliance, guideline recommendation adherence
Introduction
Upper gastrointestinal (UGIT) bleeding is a common reason for hospital admission with significant morbidity and mortality. The reported incidence varies from 48-172 per 100 000 in high-income countries.1-4 In the last two decades the mortality rate has decreased and currently ranges between 2-14%.2-8 A recent publication from South Africa by Levin in 2012 reported a mortality rate of 12.8% and surgery rate of 7.9% for non-variceal haemorrhage in 227 patients over six years.9
Clinical management has evolved with adjunct therapies and technical refinements in endotherapy and has resulted in a variety of consensus guidelines designed to improve the management and outcomes of these patients. International evidence-based guidelines contain recommendations in six categories. These are: adequate resuscitation, prognostic stratification, transfusion triggers, PPI acid suppression, early OGD and dual endotherapy.5610 Hypotension in UGIT bleed study of 1 882 patients was associated with a tenfold increased risk of death, based on a blood pressure cut off of below and above a systolic blood pressure of 90 mmHg.1 Hence this is an appropriate target blood pressure for resuscitation. In those patients with UGIT bleeding who are haemodynamically stable at presentation without ischaemic heart disease, recent evidence from a randomised control trial of patients reported better mortality outcomes with a restrictive blood transfusion strategy. They recommended Hb trigger for transfusion is < 7 g/dl and target is 9 g/dl in this category of patients.10-12
Proton pump inhibitor (PPI) therapy by lowering the pH significantly allows clot formation and prevents clot lysis. This pathophysiological benefit translates into a clinical benefit and has led to the recommendation that an intravenous bolus of PPI followed by a continuous infusion should be given to those with high risk ulcers undergoing endotherapy or in those risk stratified as high risk. The evidence for the latter is less convincing than for the former.13
In suspected variceal haemorrhage three randomised control trials support the routine use of vasoactive drugs (terlipressin, somatostatin, and vapreotide) given before endoscopy as it makes endoscopy visualisation easier and improves control of bleeding by endotherapy.14-16
The guideline recommendation for the optimal timing for oesophagogastroduodenoscopy (OGD) is dependent on the patient's clinical status and risk profile. The United Kingdom guidance is that endoscopy should be performed within 24 hours of initial assessment for stable patients. For patients with suspected variceal haemorrhage or high risk assessments on the modified Blatchford score (MBS) or pre-endoscopy Rockall score, endoscopy should be performed within 12 hours.10,17,18
Dual endotherapy is also recommended as a standard of care because a large meta-analysis in 2004 showed that adding a second modality to injection tamponade decreased re-bleeding and mortality by half.19
Despite the evidence outlined above, various analyses of compliance to these guidelines suggest that they are not rigorously implemented.17,18 Against this background we aimed to examine our compliance with regards to our guidelines adapted from international best practice in the management of patients with UGIT bleeding, before and after the implementation of a quality improvement programme (QIP).
Materials and methods
The primary aim of this study was to evaluate the compliance with time to endoscopy, transfusion triggers and dual endotherapy as defined in our guidelines, pre and post QIP. Secondary aims were to assess if implementation of QIP affected re-bleeding, surgery and mortality rates.
A QIP was undertaken over a two-month period with retrospective data collection for the pre QIP group and prospective data for the post QIP group, over one year immediately pre and post implementation. The QIP consisted of dissemination of a unit protocol via email, lectures and placement of protocol posters at strategic points. The target intervention groups were general surgery and medical gastroenterology registrars, fellows and consultants who are involved in all phases of the care of UGIT bleed patients. The QIP was re-enforced at daily intake rounds by the consultants, and new registrars were educated as they joined the unit. The investigators also ensured adequate equipment availability for dual endotherapy (injection with saline and adrenaline combined with either vessel clipping or bipolar heater probe application to the bleeding site). A customised Redcap database was developed to collect data.
The QIP focused on aspects of UGIT bleed care we perceived as being poorly adhered to at our institution. We compared adherence to the recommendations between the two cohorts for: time to OGD (within 24 hours from admission for all, and < 12 hours for suspected variceal haemorrhage and those with a MBS >10), the use of dual modality endotherapy for high risk bleeding ulcers as defined by the Forrest criteria, and blood transfusion based on a haemoglobin trigger of < 7 g/dL in haemodynamically stable patients with no ischaemic heart disease.
All patients over 12 years old admitted to acute care surgery with signs and symptoms of UGIT bleeding were eligible for study. Patients who died prior to OGD (unconfirmed bleed) or had no blood or cause for UGIT bleeding at OGD were excluded. This tertiary hospital admits UGIT bleeding from its own catchment area and the three referral secondary level hospitals that have variable ability to provide a 24-hour OGD service. The hospital provides a 24-hour OGD service in a dedicated endoscopy unit during working hours (08:00-16:00 weekdays) with after-hours OGD being performed in the operating theatre. Patients who presented with Grade III shock (SBP < 100, HR > 120) were deemed unstable. Patients with admission haemoglobin of above 10 g/ dL, stable haemodynamics and OGD findings of low Forrest grade lesions who had no comorbidities were managed by the emergency unit and not admitted to the surgery unit. For the retrospective cohort we collected data and risk scores from patient notes and laboratory results, and management of the patient was at the admitting teams' clinical discretion. The protocol for the QIP group entailed adequate resuscitation first and if there were signs of ongoing bleeding (persistent hypotension or tachycardia, obvious exsanguination), an urgent OGD was performed. The validated MBS was used to stratify the patients into high risk and low risk groups. The MBS is a pre-OGD tool that utilises admission clinical and laboratory findings (systolic blood pressure, heart rate, Hb and urea) for stratification. Patients with a MBS score of 10 or more are prioritised to early OGD (< 12 hours) and those less than 10 to OGD within 24 hours.1,17 Suspected variceal bleed patients were stratified as at high risk of re-bleeding and deemed to require early (< 12 hours) OGD.
At OGD the QIP recommendation for ulcers with high risk stigmata of bleeding (Forrest Ia, Ib, Ila and lib) was to utilise dual modality endotherapy for haemostasis. The admitting team were also advised to use a restrictive blood transfusion strategy for haemodynamically stable patients with no ischaemic heart disease. These recommendations were reinforced on daily rounds by the consultant body who were also the study investigators. Failure to use dual modality endotherapy adequately was also seen as an opportunity to investigate mitigating factors, to address them and to teach with the aim of reemphasising recommendations.
Post OGD Rockall score parameters were recorded to identify patients at risk of re-bleeding and death. The Child-Pugh score was used to assess severity of liver decompensation in variceal bleeding. Local practice is to give a single dose of an intravenous PPI to high risk patients at admission and to continue as indicated by OGD findings. Those with suspected variceal haemorrhage received an octreotide infusion on admission prior to OGD. Repeat OGD was only done on demand where there was clinical concern of ongoing bleeding. Adequate resuscitation and adjunct PPI and octreotide use had been addressed previously as part of a clinical audit of best practice, and steps to emphasise these goals had already been carried out prior to this formal QIP study and compliance with these parameters was not assessed in this study.
Statistical analysis
Categorical data are presented using frequency tables with percentages. Chi-square tests were conducted where appropriate to test for association between categorical variables. Continuous data are summarised in terms of means and standard deviations, and t-tests for comparison of group means are used to test for significance.
Ethical permission to conduct the study was granted by the university (HREC 244/2017) and the institution. No consent was taken for the retrospective cohort. The QIP group's data was collected with verbal consent. All data was captured and stored in a password protected database and computer. The data was collated anonymously, so patients could not be identified from the final dataset used for analysis.
Results
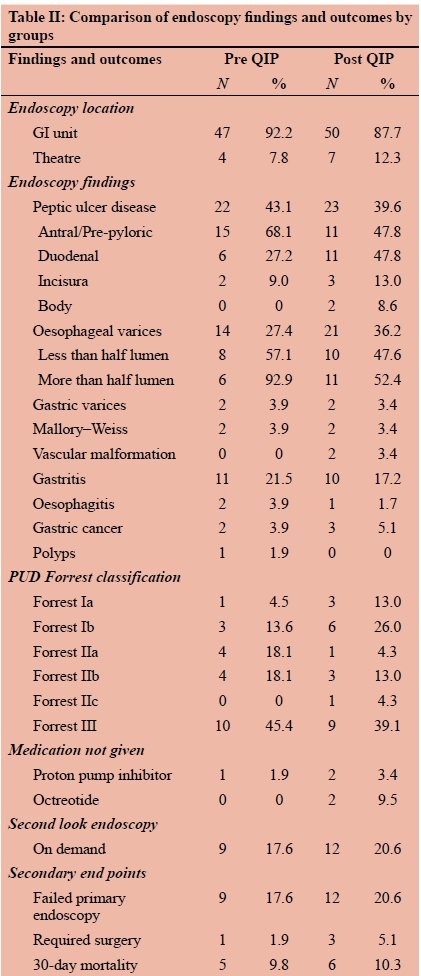
This study included 109 patients, 51 in the pre QIP and 58 in the post QIP groups. Table I details the demographic and comparative variables. These groups' baseline data were not statistically different except for the higher use of prophylactic aspirin in the pre QIP. The OGD findings are detailed in Table II.
The first end point assessed for adherence was 'Time to OGD'. Over 80% in both groups had their OGD within 24 hours (pre QIP 82.3%, post QIP 81.0%, p = 0.07). The overall and high-risk groups (variceal and MBS > 10) had slightly longer time to scope in the post QIP group but this was not significant (Table III). Combining all the patients in the pre and post QIP groups with a high MBS (> 10) showed an eight hours shorter time to OGD than the low scoring (MBS < 10) patients (p = 0.02).
The second end point assessed for adherence was use of dual endotherapy for bleeding ulcers. In the pre QIP group there were 12 patients with high risk stigmata of a bleeding ulcer (Forrest Ia to IIb), of these five (41.6%) had dual therapy compared to 10 bleeding ulcers out of 14 (71%) in post QIP group (p = 0.23). We also compared the use of dual endotherapy for all non-variceal etiology in the presence of blood on OGD. The practice of dual endotherapy improved post implementation (p = 0.023) of QIP (Table III).
Surgery for endotherapy failure was not required in the pre QIP group and required in three patients in the post QIP group. Surgery involved gastrotomy with over-sewing of bleeding vessel and no resections were required. One patient in the pre QIP group underwent a negative laparoscopy for suspected perforation. Repeat OGD was done for concern of re-bleeding in nine (17.6%) patients in the pre QIP group and in 12 (20.6%) patients in the post QIP group.
There were 14 (27.4%) and 21 (36.2) patients with oesophageal variceal bleed in pre QIP and post QIP groups respectively. All oesophageal varices were managed with endoscopic banding whilst gastric varices were treated with sclerotherapy (histo-acryl glue injection) (Table II).
The third end point assessed for adherence was a restrictive blood transfusion strategy in haemodynamically stable patients based on a Hb trigger of 7 g/dL and target of 9 g/dL, without ischaemic heart disease. Blood transfusions were performed in 72.5% pre QIP group and 65.5% post QIP (Table I). The reason for transfusion was for resuscitation in 17.6% of the pre QIP group and in 13.8% of the post QIP group. The rest were transfused because of a low haemoglobin or symptomatic anaemia. The mean Hb in stable patients who were transfused was statistically different between pre QIP group 6.3 g/dL (SD ± 2) and post QIP 5.7 g/dL (SD ± 1.69) (p = 0.04). The number of transfusions for Hb above 7 g/ dL was 12 (23.5%) in the pre QIP group compared to six (10.3%) in the post QIP group (p = 0.047).
There was one major morbidity in the pre QIP group. A patient had a negative laparoscopy for a suspected perforation post OGD after dual endoscopic therapy of a high-risk antral ulcer.
The mortality rate during the index admission was 5.9% in the pre QIP group and 1.7% in the post QIP group. Only one death was directly related to bleeding and this was in the post QIP group. Thirty-day mortality rate was 9.8% in the pre QIP group and 10.3% in the post QIP group, which was statistically insignificant.
Univariate analysis of 30-day mortality risk for both pre and post QIP groups was performed for these variables: age, Hb, Grade III shock, urea, MBS, time to OGD, presence of blood at OGD and OGD findings. Only the presence of Grade III shock reached significance as 30-day mortality risk (p = 0.009).
Discussion
Guidelines for the management of UGIT bleed are constantly being refined by expert panels as evidence from RCT and cohort studies have accrued to provide robust evidence.
The guideline recommendation for the optimal timing for OGD is dependent on patient's clinical status and risk profile. A meta-analysis and other studies comparing very early (< 12 hours) to late early (> 12 hours) endoscopy found no significant reduction in re-bleeding, surgery or mortality.20,23 Moreover, it was found that urgent OGD (0-8 hours) versus early OGD (6 or 8-24 hours), did not show differences in clinical outcome.22,24,25 Registry audits show variable adherence to the OGD timing guideline. In the United Kingdom there was a 47.5-66% compliance to endoscopy within 24 hours in baseline audits.1718 The Canadian RUGBE study showed that 76% had their OGD within 24 hours.2 Our finding that OGD was performed within 24 hours in more than 80% of our cohorts was encouraging. This was despite more than half of our patients being admitted after hours (pre QIP 70.5%, post QIP 58.6%). This study also demonstrated that, overall, patients with higher MBS had shorter time to endoscopy on average by eight hours. This implies that even before the QIP implementation patients were being risk stratified and triaged appropriately.
The recommendation for the routine use of dual endotherapy is based on a large meta-analysis that showed adding a second modality to injection tamponade decreased re-bleeding from 18.4-10.6% and mortality from 5.1-2.6%.19 Despite this evidence, a French audit in 2006 showed that 70.9% had injection therapy alone for high risk bleeding ulcers and mirrored our own institution's practice of a 100% monotherapy use for high risk ulcers reported by Levin et al. between 2004 and 2009.9-26 The improved compliance to dual endotherapy from 25% pre to 50% post intervention was indirectly contributed to by the QIP raising awareness of the need to ensure the availability of accessories for dual therapy out of hours .
A restrictive blood transfusion strategy is applied to blood transfusion not only for UGIT bleed but for several indications across disciplines. A reduction in mortality based on a Hb trigger for transfusion of < 7 g/dl was reported in a 2013 RCT.12 In this study the sub groups with the greatest benefit were Child-Pugh A and B patients with variceal bleeding. In addition, their liberal strategy group had higher re-bleeding and adverse events. This QIP significantly reduced inappropriate over transfusions in our study from 23% in the pre QIP group to 10% in the post QIP group.
The QIP was not designed to detect differences in re-bleeding, surgery or mortality rates. because of their relative infrequent occurrence. The mortality rate in this study of 9.8% and 10.3% is in keeping with reports in the international literature.2,3, 27 Levin's study done at the same institution over six years looked at high risk bleeding ulcers only and had a mortality of 12.8%.9 In the current study the mortality rate was 3.7% for the sub-group of patients with high risk ulcers (Forrest Ia, Ib, Ila and lib), but the total number of patients was significantly less than in Levin's cohort.
In terms of risk stratification, the mean Rockall score was 3.45 and 3.54 in pre QIP and post QIP groups respectively, both being medium risk. In Rockall's study the overall mortality rate was 5.3% for medium risk patients. The 30-day mortality rate of 9.8% and 10.3% in this study is higher than found for the same risk group in Rockall's study.3 The higher mortality of the "medium risk' patients in our study is concerning. What we lack is adequate monitoring facilities for these patients. High care facilities for the medium to high risk patients can help detect clinical deterioration early and mitigate the higher mortality rate that occurs from decompensation in patients with comorbid disease.
Presentation with shock was the only significant risk factor associated with mortality in this study. The initial hypotension and transient tissue hypoxia prior to resuscitation has far reaching complications unfolding a cascade of organ function decompensation. Only one bleeding related death occurred, the rest of the deaths were due to decompensation of medical comorbidity. This emphasises the need to adequately and appropriately resuscitate the patient as initial hypotension is more likely to cause death than ongoing bleeding. The focus of the clinician must shift from immediate OGD to a good resuscitation effort initially and then re-evaluation of urgency in obtaining an OGD.
The QIP has improved compliance to two of the three end points. The NICE QIP audit in 2012/2013 highlighted the need for educating clinicians on a regular and repeated basis to ensure guideline adherence.17 It is not merely sufficient to have many complex guidelines if this does not reach day to day practice. Quality audits and improvements based assessment of the key parameters together with continuous education of clinicians can result in better patient care. Unit protocols with standardised admission forms pertinent to risk stratification and therapy checklists can aid clinicians in better management of UGIT bleeding, especially when junior staff rotate frequently. This QIP has also galvanised the lead clinicians (first and third authors) into continuous oversight of the GI bleeding service through ensuring that junior staff are educated, that recommendations are followed, and that equipment is always available.
Conclusion
This upper GI bleeding QIP initiative has improved adherence to defined guideline criteria for two key performance indicators, transfusion triggers and the ability to deliver dual endotherapy. Our guideline adherence compares favourably to other international QIP reports including the time frames of performance of OGD, a parameter not improved by this QIP. There is an obvious need to continue to monitor adherence to all the recommendations particularly when there are evidence-based changes to guidelines.
Acknowledgements
Dr Juan Klopper for his help with restructuring the study protocol which enabled a smoother journey for ethics approval.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
The study protocol was approved by the Univerity of Cape Town Human Research Ethics Committee (244/2017).
ORCID
S Rayamajhi https://orcid.org/0000-0002-0930-9990
I Aborkis https://orcid.org/0000-0003-3689-8441
C Kloppers https://orcid.org/0000-0003-2438-6879
R Spence https://orcid.org/0000-0001-8470-6980
SR Thomson https://orcid.org/0000-0002-9485-997X
REFERENCES
1. Blatchford O, Davidson LA, Murray WR, Blatchford M, Pell J. Acute upper gastrointestinal haemorrhage in west of Scotland: case ascertainment study. BMJ. 1997 Aug;315(7107):510-5. [ Links ]
2. Barkun A, Sabbah S, Enns R, et al. The Canadian Registry on Nonvariceal Upper Gastrointestinal Bleeding and Endoscopy (RUGBE): endoscopic hemostasis and proton pump inhibition are associated with improved outcomes in a real-life setting. Am J Gastroenterol. 2004 Jul;99(7):1238-46. [ Links ]
3. Rockall TA, Logan RF, Devlin HB, Northfield TC. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. Steering Committee and members of the National Audit of Acute Upper Gastrointestinal Haemorrhage. BMJ. 1995 Jul;311(6999):222. [ Links ]
4. Leerdam ME, Vreeburg EM, Rauws EA, et al. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol. 2003;98(7):1494-99. [ Links ]
5. Barkun A, Bardou M, Marshall JK. Consensus recommendations for managing patients with nonvariceal upper gastrointestinal bleeding (Clinical Guidelines). Ann Intern Med. 2003 Nov;139(10):843-57. [ Links ]
6. Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010 Jan;152(2):101-13. [ Links ]
7. Dworzynski K, Pollit V, Kelsey A, Higgins B, Palmer K. Management of acute upper gastrointestinal bleeding: summary of NICE guidance. BMJ. 2012 Jun;344(7861):45-7. [ Links ]
8. Parvez MN, Goenka M, Tiwari I, Goenka U. Spectrum of upper gastrointestinal bleed: an experience from Eastern India. J Dig Endosc. 2016;7(2):55-61. [ Links ]
9. Levin DA, Watermeyer GA, Deetlefs E, Metz DC, Thomson SR. The efficacy of endoscopic therapy in bleeding peptic ulcer patients. South African Med J. 2012 May;102(5):290-3. [ Links ]
10. Stanley AJ, Laine L. Management of acute upper gastrointestinal bleeding. BMJ. 2019;364. https://doi.org/10.1136/bmj.l536. [ Links ]
11. Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012;107(3):345. https://doi.org/10.1038/ajg.2011.480. [ Links ]
12. Stokes A, Thompson C, Clegg A, Snook J. The influence of a simple blood transfusion policy on overtransfusion in acute upper gastrointestinal haemorrhage. Clin Med. 2015 Aug;15(4):325-9. [ Links ]
13. Laine L, Mcquaid KR. Endoscopic therapy for bleeding ulcers: an evidence-based approach based on meta-analyses of randomised controlled trials. Clin Gastroenterol Hepatol. 2009;7(1):33-47. https://doi.org/10.1016/j.cgh.2008.08.016. [ Links ]
14. Levacher S, Blaise M, Pourriat JL, et al. Early administration of terlipressin plus glyceryl trinitrate to control active upper gastrointestinal bleeding in cirrhotic patients. Lancet. 1995;346(8979):865-8. https://doi.org/10.1016/S0140-6736(95)92708-5. [ Links ]
15. Avgerinos A, Nevens F, Raptis S, Fevery J. Early administration of somatostatin and efficacy of sclerotherapy in acute oesophageal variceal bleeds: the European Acute Bleeding Oesophageal Variceal Episodes (ABOVE) randomised trial. Lancet. 1997;350(9090):1495-99. https://doi.org/10.1016/S0140-6736(97)05099-X. [ Links ]
16. Calès P, Masliah C, Bernard B, et. al. French Club for the Study of Portal Hypertension. Early administration of vapreotide for variceal bleeding in patients with cirrhosis. N Engl J Med. 2001 Jan;344(1):23-28. [ Links ]
17. Wu AX, Cheung M, Forshall E, Tritto G. Audit of management of acute upper gastrointestinal bleeding in a district general hospital trust against National Institute of Health and Care Excellence (NICE) guidelines. Future Hosp J. 2015 Jun;2(2):9. [ Links ]
18. Shih P, Liu S, Li S, et al. Weekend effect in upper gastrointestinal bleeding: a systematic review and meta-analysis. Peer J. 2018 Jan;6:e4248. [ Links ]
19. Calvet X, Vergara M, Brullet E, Gisbert JP, Campo R. Addition of a second endoscopic treatment following epinephrine injection improves outcome in high-risk bleeding ulcers. Gastroenterology. 2004;126(2):441-50. https://doi.org/10.1053/j.gastro.2003.11.006 [ Links ]
20. Lin H, Wang K, Perng C, et al. Early or delayed endoscopy for patients with peptic ulcer bleeding: A prospective randomised study. J Clin Gastroenterol. 1996 Jun;22(4):267-71. [ Links ]
21. Lee JG, Turnipseed S, Romano PS, et al. Endoscopy-based triage significantly reduces hospitalisation rates and costs of treating upper GI bleeding: A randomised controlled trial. Gastrointest Endosc. 1999;50(6):755-61. [ Links ]
22. Tai CM, Huang SP, Wang HP, et al. High-risk ED patients with nonvariceal upper gastrointestinal hemorrhage undergoing emergency or urgent endoscopy: a retrospective analysis. Am J Emerg Med. 2007;25(3):273-8. [ Links ]
23. Bjorkman DJ, Zaman A, Fennerty MB, et al. Urgent vs. elective endoscopy for acute non-variceal upper-GI bleeding: An effectiveness study. Gastrointest Endosc. 2004;60(1):1-8. [ Links ]
24. Targownik LE, Murthy S, Keyvani L, Leeson S. The role of rapid endoscopy for high-risk patients with acute nonvariceal upper gastrointestinal bleeding. Can J Gastroenterol. 2007;21(7):425-9. [ Links ]
25. Schacher GM, Lesbros-Pantoflickova DA, Ortner MB, et al. Is early endoscopy in the emergency room beneficial in patients with bleeding peptic ulcer? A "fortuitously controlled" study. Endoscopy. 2005;37(4):32428. https://doi.org/10.1055/s-2004-826237 [ Links ]
26. Zeitoun JD, Rosa-Hézode I, Chryssostalis A, et al. Epidemiology and adherence to guidelines on the management of bleeding peptic ulcer: a prospective multicenter observational study in 1140 patients. Clin Res Hepatol Gastroenterol. 2012;36(3):227-34. [ Links ]
27. Marmo R, Koch M, Cipolletta L, Bet al. Predicting mortality in patients with in-hospital nonvariceal upper GI bleeding: a prospective, multicenter database study. Gastrointest Endosc. 2014 May;79(5):741-9. https://doi.org/10.1016/j.gie.2013.10.009. [ Links ]
 Correspondence:
Correspondence:
email: shreya.rayamajhi@uct.ac.za














