Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.58 no.4 Cape Town dic. 2020
http://dx.doi.org/10.17159/2078-5151/2020/v58n4a3159
TRAUMA
Can computed tomographic angiography accurately exclude digestive tract injury after penetrating cervical trauma?
JPB MaritzI; A BagadiaII; JA LubbeI
IDivision of Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Hospital, South Africa
IIDivision of Radiology, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Hospital, South Africa
ABSTRACT
BACKGROUND: Multislice computed tomographic angiography (MCTA) has become the method of choice to screen for arterial injury in penetrating cervical trauma (PCT). There is, however, limited knowledge on its accuracy in terms of digestive tract injury (DTI). Currently, our unit liberally employs both computed tomographic angiography (CTA) and contrast swallow for platysma breaching penetrating neck injuries. This study aimed to determine the accuracy of specific computed tomography findings in the diagnosis of DTI after PCT.
METHODS: This was a retrospective review of all consecutive patients with PCT who had undergone MCTA that presented at a single, tertiary, high-volume trauma centre from January 2013 until December 2015. Blinded radiological review of 140 MCTA investigations (33 in the injury group and 107 in the control group) was performed in order to calculate the diagnostic accuracy of trajectory, air, and conventional MCTA signs in the diagnosis of DTI after PCT.
RESULTS: Over the study period, 906 patients presenting with PCT had undergone MCTA and a total of 33 patients (3.6%) had confirmed DTI on aggregate gold standard of diagnosis. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of MCTA for detecting DTI was 100%, 65.4%, 47.1%, and 100%, respectively. No injuries were missed on MCTA.
CONCLUSION: Our findings suggest that DTI can be safely excluded by means of careful assessment of specific signs on CTA in patients presenting after PCT, obviating the need for further investigation.
Keywords: computed tomography, CTA, digestive tract injury, oesophagus, pharynx, penetrating trauma
Introduction
Oesophageal perforation is relatively uncommon after penetrating cervical trauma (PCT), can prove fatal if missed, and remains notoriously difficult to diagnose. Due to a widespread increase in endoscopic intervention, iatrogenic perforation has been shown to be the most common cause of digestive tract injury (DTI) in most series. That said, in areas of the world where trauma is prevalent, PCT dominates as etiological factor.1 Although both mechanisms of injury are commonly characterised by a break in the oesophageal wall, the primary difference between these mechanisms is the presence of a tract in cases of external penetration. Due to this concomitant disruption of tissues surrounding the oesophagus, the extent of which is often unpredictable, the diagnosis and clinical course might differ for DTI after PCT.
Since the advent of non-operative treatment strategies after PCT (i.e. by selective non-operative management or minimally invasive endovascular or endoscopic means), there has been an increased urgency to not only detect but also to define the extent of injuries via imaging, often prolonging time to definitive diagnosis.2 The evolution of multislice computed tomographic angiography (MCTA) has held great promise and has become the method of choice to screen for arterial injury according to zone,3-5 with some authors advocating its use even in stable patients with hard signs of underlying vascular injury.6 In contrast, there is limited knowledge on the accuracy of MCTA in terms of the digestive tract, with available studies including limited numbers of patients. A report published in 2001 that analysed 23 MCTA examinations7 suggested that determination of trajectory can safely eliminate the need for further investigations. The aforementioned report indicated that 11 of 23 patients who sustained PCT could be discharged within 24 hours of admission. Although a gradual incorporation of MCTA into the diagnostic algorithm over the following years led to a decrease in negative explorations, it was not accompanied by a concomitant decrease in adjunctive studies conducted to safely exclude DTI.89
Currently, our unit liberally employs both MCTA and contrast swallow for platysma breaching penetrating neck injuries. The aim of this study was to determine the diagnostic accuracy of tract- and air-specific computed tomography findings after PCT.
Methods
Study population
We retrospectively reviewed all records of consecutive patients with PCT who had undergone MCTA, who presented at a single, tertiary, high-volume trauma centre from January 2013 until December 2015. Inclusion criteria comprised the following: 1) platysma breaching penetrating injury to Zones I-III of the neck, and 2) acquisition of MCTA, followed by an aggregate gold standard of diagnosis for DTI (including either surgical exploration, contrast swallow, endoscopic examination, or clinical follow-up).
Both mechanism of injury and external wound location were determined for each case, and location of injury in the digestive tract was noted. Recorded symptoms and signs were documented. Zones of the neck were defined according to generally accepted consensus definitions10 and Standard of Reporting of Diagnostic Accuracy Studies (STARD) guidelines were followed.11
Institutional protocol and MCTA procedures
All patients with platysma penetrating injuries presenting to hospitals serviced by our trauma centre are referred for assessment at tertiary level. Hemodynamically unstable patients who do not respond to fluid resuscitation, or actively bleeding patients who do not respond to balloon tamponade, are immediately taken to theatre. All remaining patients undergo both MCTA investigation and contrast swallow/pull back. Endoscopy is performed in unconscious or intubated patients where contrast swallow/pull back is less accurate, and in cases with a high clinical suspicion of DTI. If there is an indication for surgical repair of arterial, airway or lymphatic injury, or when the penetrating weapon is still in situ, the digestive tract is explored at the time of surgery. MCTA is performed on a 40-slice scanner (Siemens; Healthcare, Berlin, Germany). Eighty millilitres of iohexol iodinated IV contrast material (Omnipaque 300, GE Healthcare, Cork, Ireland) is injected at a rate of 4 ml/second, followed by a 50 ml saline flush using a Mallinckrodt power injector (Mallinckrodt Pharmaceuticals, Staines-upon-Thames, Surrey, England). Images are acquired in transverse sections of 0.6 mm thickness, from the base of the skull to the top of the aortic arch, and the slice thickness of the multiplanar reconstructed images is adjusted according to the reporting radiologist's preference. Images are reported on by the on-call radiologist (with a wide range of experience) and are available to the trauma team (both medical officers and trauma surgeon) on the picture archiving and communication (PACS) system.
Diagnostic accuracy
A cohort of patients without DTI who had undergone MCTA (i.e. control group) were selected by means of simple random sampling (using a computer-generated table). The MCTA investigations of the control group, together with the MCTA investigations of all patients with DTI (i.e. injury group), were anonymised, randomised, reports were removed, and the image files were securely stored in a separate folder. A senior radiologist with more than 10 years of experience in evaluating trauma imaging, and blinded to the presence of DTI, reported on all the MCTA investigations using a predefined tick sheet. The presence of a platysma penetrating cervical injury was known by the radiologist, but no further clinical information was made available. In addition, the external wound was not marked.
We investigated the diagnostic accuracy of MCTA by assessing the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of MCTA for trajectory- and air-associated signs of DTI, as well as conventional signs of DTI.
MCTA signs of DTI
Trajectory-associated signs that were evaluated included: 1) tract into/through the aerodigestive system, 2) tract violating the deep neck spaces (Figure 1), and 3) transcervical tract. Air-associated signs included: 1) air in the deep neck spaces (Figure 1), 2) air in the superficial soft tissue, 3) mediastinal air, and 4) pneumothorax. Conventional signs included: 1) fluid in the deep neck spaces (Figure 2), 2) wall defect, 3) irregular or thickened wall, and 4) active mucosal bleeding. Deep neck spaces were defined as deep to the middle layer of the fascia colli or deep cervical fascia. A decision was made as to whether the MCTA was diagnostic of a DTI or excluded a DTI. The report included options to indicate when a tract could not be reliably determined or when artifact precluded
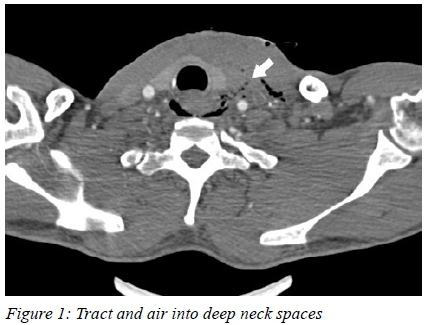
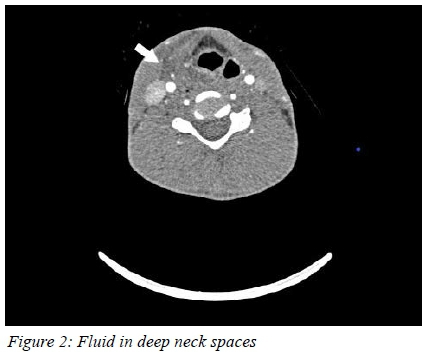
evaluation of the investigation.
Statistical analysis
Descriptive statistics were calculated for demographic variables. Counts and associated percentages were used to describe clinical characteristics of the sample. A priori sample size calculation was performed, specifying sensitivity of 90% with a 95% confidence interval of 5%, resulting in a required sample size of 140 MCTA investigations to be included. Standard formulas were used to calculate sensitivity, specificity, PPV and NPV. All data were analysed using STATA 14.
Results
Over a period of three years (January 2013 to December 2015), 906 stable patients presenting with PCT underwent MCTA at our institution. Contrast swallow was performed in all 906 patients. Thirty-three patients (3.6%) with confirmed DTI, diagnosed by aggregate gold standard (i.e. exploration, contrast swallow, endoscopy or clinical follow-up), were identified. The cases with confirmed DTI had a mean age of 29 years (SD = 9.9) and were predominantly male (90%).
Table I depicts the baseline clinical characteristics of the injury (case) and control groups. Of the 33 cases with DTI, the majority of injuries (25/33, 76%) were secondary to stab wounds, while gunshot wounds (GSW) were present in 24% (8/33) of cases. External penetration in Zone II was evident in 58% of cases (19/33), with the remainder equally distributed between Zones I (6/33) and III (6/33). Two patients had wounds in more than one zone of the neck. The left side of the neck was involved in 21 cases (64%). Twenty-four patients (73%) had a pharyngeal injury and nine patients (27%) had a cervical oesophageal injury.
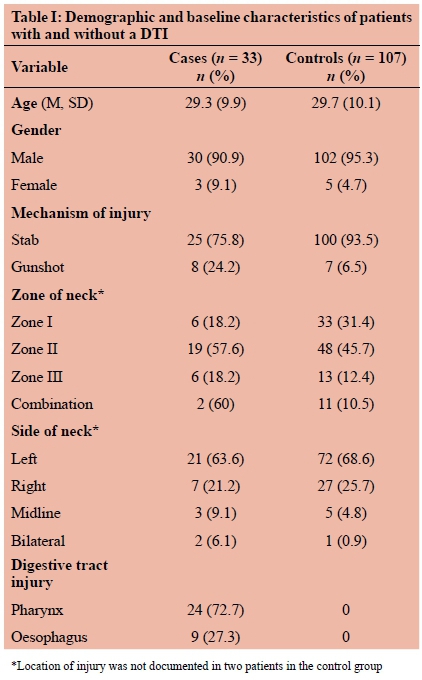
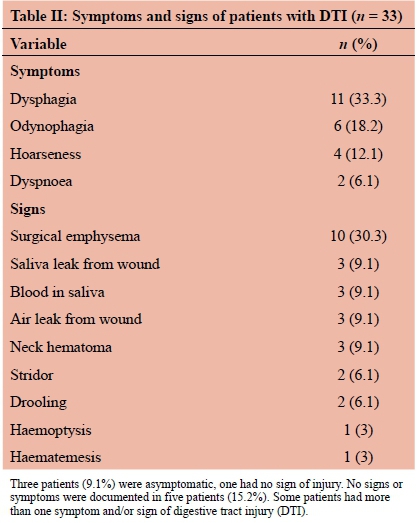
Table II depicts the presenting symptoms and signs present in the 33 patients with DTI. Three patients (9%) were asymptomatic, one of whom also had no signs of injury. In 15% (5/33) of the cases, only wound location was documented, with no mention of accompanying symptoms or signs.
After retrospective blinded review of 140 MCTA investigations, 33 with injuries (i.e. injury group) and 107 without injuries (i.e. control group), a 'tract' could be reliably determined in all and artifact did not preclude evaluation of any of the investigations. Overall sensitivity and specificity of MCTA for detecting DTI was 100% (95% CI: 89.4-100) and 65.4% (95% CI: 55.6-74.4), respectively. The PPV and NPV of MCTA for detecting DTI was 47.1% (95% CI: 35.1-59.4) and 100% (95% CI: 94.4-100), respectively, with a positive likelihood ratio of 2.89 (95% CI 2.2-3.8) being determined.
Sensitivity, specificity, PPV and NPV for the individual signs of DTI on MCTA are represented in Table III. Active mucosal bleed could not be identified by the radiologist in any of the MCTAs and was therefore not included in the evaluation for diagnostic accuracy.
Discussion
Our results suggest sufficient accuracy of MCTA in cases where injury tract and the deep neck spaces are scrutinised, excluding the need for further investigations for DTI after PCT. In the current study, overall sensitivity and NPV of MCTA for detecting DTI was 100%.
The incidence of DTI after PCT has been found to range from 0.02% to 9%,12,13 with an incidence of 3.6% being determined in this study. Worldwide, injuries to the pharynx and cervical oesophagus are more common than injuries to the relatively protected intra-thoracic and short intra-abdominal segments.14 It has also been noted that mortality increases as the injury is found more distally in the digestive tract.13,15 Overall mortality rates range from 2%14 to 44%,16 and associated injuries, mostly arterial, usually account for early deaths, while delayed sepsis due to missed DTI can lead to considerable morbidity in up to 53% of patients.17 In line with previous studies,1217 our series of confirmed DTI revealed mostly young male patients with stab injury to Zone II of the left neck.
Diagnosis of DTI after PCT based on symptoms, signs, and plain radiography remains controversial. Prospective studies that have investigated the presence of symptoms suggestive of DTI have reported conflicting results1820 and were largely based on small numbers of varying patient populations. In our series, 9% of patients were asymptomatic. It must be noted, however, that data on accompanying symptoms and signs were not available for 15% of cases. After iatrogenic and spontaneous oesophageal perforation, up to 12% of plain films can be normal,21 whereas the number after PCT is still unknown.
Previous studies that have reported on the sensitivity and specificity of MCTA for detecting injuries after PCT have determined figures ranging from 50% to 100% and 50% to 98%, respectively.2224 Awais et al. investigated the accuracy of CT chest to detect oesophageal perforation and reported a sensitivity, specificity, PPV and NPV of 100%, 54%, 23% and 100%, respectively. The authors concluded that additional imaging modalities can be omitted if there is no evidence of pneumomediastinum, mediastinal fluid collections or oesophageal wall defects.25 In our series, sensitivity and specificity of MCTA was found to be 100% and 65.4%, respectively. The three most sensitive signs on MCTA, except for 'air in the superficial soft tissue' which all patients had, were 'tract into/through the digestive tract' (94%), 'tract violates the deep neck spaces' (91%), and 'air in the deep neck spaces' (97%). Associated NPVs for the aforementioned signs were 97.5%, 96.2%, and 98.3%, respectively.
CT oesophagography has been proven to be reliable in diagnosing penetrating upper digestive tract injuries. Conradie and Gebremariam established CT oesophagogra-phy as having a sensitivity and NPV of 95% and 98.6%, respectively. Para-oesophageal/hypopharyngeal air and endoluminal contrast extravasation were found to be the most sensitive findings. The sensitivity and NPV were increased to 100% each when CT oesophagography was combined with CTA.26 CT oesophagography is a dynamic study and requires the active participation of the patient and specific operator training which might pose difficulties for some patients and health facilities.27
Two recent studies scrutinised the performance of specific MCTA signs of DTI after PCT, with the results suggesting that treatment algorithms be based on findings. Bodanapally et al. investigated trajectory-related signs and suggested that no further investigation would be necessary in wounds with a trajectory not breaching the deep neck spaces.28 This targeted selective management approach was based on a specificity of 97% for a tract extending into the aerodiges-tive system, and a sensitivity of 97% for a tract violating the deep neck spaces.28 In the current study, the associated specificity and sensitivity of these signs were 72.9% and 90.9%, respectively. In our series, one injury would have been missed if only trajectory-related signs had been taken into account. This one injury was, however, a pharyngeal injury diagnosed on MCTA, resulting from the presence of fluid in the deep neck spaces. Madsen et al. analysed the value of deep surgical emphysema found on MCTA after PCT as an indicator of aerodigestive tract injury.29 They found MCTA to demonstrate sensitivity, specificity, PPV, and NPV of 94.1%, 71.9%, 30%, and 98.9%, respectively. The authors concluded that the absence of surgical emphysema in the deep cervical fascial planes excluded clinically significant aerodigestive tract injury, with no further imaging being necessary. Our findings are consistent with the aforementioned figures, with sensitivity, specificity, PPV, and NPV for the presence of air in the deep neck spaces being 97%, 55%, 40%, and 98%, respectively. In our series, there was a single patient with a pharyngeal injury who had the presence of fluid but no air in the deep neck spaces. Our findings suggest that when either 'tract into/ through the digestive tract' or 'tract violates the deep neck spaces' and 'air in the deep neck spaces' are all present in the same patient, all DTIs are accurately diagnosed, excluding the one pharyngeal injury in which none of these signs were present. In this patient, DTI was diagnosed on MCTA by the presence of significant fluid in the deep neck spaces, ensuring no injuries were missed by MCTA.
Instances where the 'tract' might be difficult to determine might occur after stab wounds where minimal soft tissue disruption occurs. Likewise, in gunshot injuries with accompanying pneumothorax and surgical emphysema, 'tract' might be impossible to follow. The relatively larger size and lower intraluminal pressures encountered in the pharynx make the likelihood of intraluminal air escape into surrounding soft tissues less likely, thus posing a challenge when looking for MCTA signs suggestive of full thickness injury. Taking into account that the amount of time that elapses between injury and imaging might influence expected MCTA signs, our suggested approach to exclusion of a DTI after penetrating cervical trauma is illustrated in Figure 3.
Study limitations
The strength of our study is that all patients with platysma breaching injury at our institution, unless unstable, undergo both MCTA and contrast swallow assessment. As a result, partial verification bias is decreased and a large pool of imaging is generated. There are a number of limitations to the study. These include the retrospective design of the study and the fact that concomitant injuries and time taken to acquire the MCTA could not be taken into account. Images evaluated during the conduct of this study were generated on a 40-slice scanner. Newer generation scanners with higher slice counts offer better spatial resolution with reduced scanning time and they reduce motion artifacts, rendering better quality of images. During blinded radiological review, the presence of a tick sheet and participation in a study may have introduced bias. In addition, senior radiologist assistance to the trauma surgeon may not always be available, especially after-hours. Finally, the simultaneous analysis of a number of variables (i.e. signs) may have introduced bias in terms of determining the individual contribution of these variables.
As a result of this study, radiologists at our centre now report all scans after penetrating cervical trauma according to a tick sheet, thus not only teaching the specific signs of DTI to the junior team (both radiology and trauma), but also decreasing missed injuries and limiting unnecessary further imaging.
Recommendations
Recommendations for future research include larger scale prospective studies that will aid in definitively placing computed tomography in the diagnostic algorithm for DTI after PCT.
Conclusion
The evaluation of the diagnostic accuracy of MCTA to diagnose DTI in our study revealed a sensitivity of 100%, a specificity of 65.4%, a PPV of 47.1% and an NPV of 100%. No injuries were missed on MCTA, ensuring no false negatives. Despite not being a very specific investigation, MCTA proved to be very sensitive and accurate in excluding injury if trajectory was found to not breach the deep neck spaces or digestive tract and no air or fluid was present in the deep neck spaces. If DTI is suspected on MCTA, further confirmatory investigations need to be employed, whereas if injury is excluded, no further investigation is needed.
Findings from our study suggest that in patients presenting after PCT, DTI can be safely excluded by means of careful assessment of specific signs on CTA, obviating the need for further investigation.
Acknowledgements
We thank Dr Lindi Martin for her assistance and valuable contribution. This study was conducted with support from the South African Medical Research Council (SAMRC). We also wish to thank the Stellenbosch University Division of Epidemiology and Biostatistics for their statistical support.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the Health Research Ethics Committee (HREC) of Stellenbosch University (Reference: S16/04/063).
REFERENCES
1. Hasimoto CN, Cataneo C, Eldib R, et al. Efficacy of surgical versus conservative treatment in esophageal perforation: a systematic review of case series studies. Acta Cir Bras. 2013;28(4):266-71. [ Links ]
2. Yeh DD, Hwabejire JO, De Moya M, et al. Preoperative evaluation of penetrating esophageal trauma in the current era: An analysis of the National Trauma Data Bank. J Emerg Trauma Shock. 2015;8(1):30-3. [ Links ]
3. Bodanapally UK, Dreizin D, Sliker CW, Boscak AR, Reddy RP. Vascular injuries to the neck after penetrating trauma: diagnostic performance of 40- and 64-MDCT angiography. Am J Roentgenol. 2015;205(4):866-72. [ Links ]
4. Tisherman SA, Bokhari F, Collier B, et al. Clinical practice guideline: penetrating zone II neck trauma. J Trauma. 2008; 64(5):1392-405. [ Links ]
5. Sperry JL, Moore EE, Coimbra R, et al. Western Trauma Association critical decisions in trauma: penetrating neck trauma. J Trauma Acute Care Surg. 2013;75(6):936-40. [ Links ]
6. Schroll R, Fontenot T, Lipcsey M, et al. Role of computed tomography angiography in the management of Zone II penetrating neck trauma in patients with clinical hard signs. J Trauma Acute Care Surg. 2015;79(6):943-50; discussion 950. [ Links ]
7. Gracias VH, Reilly PM, Philpott J, et al. Computed tomography in the evaluation of penetrating neck trauma: a preliminary study. Arch Surg. 2001;136(11):1231-5. [ Links ]
8. Woo K, Magner DP, Wilson MT, Margulies DR. CT angiography in penetrating neck trauma reduces the need for operative neck exploration. Am Surg. 2005;71(9):754-8. [ Links ]
9. Osborn TM, Bell RB, Qaisi W, Long WB. Computed tomographic angiography as an aid to clinical decision making in the selective management of penetrating injuries to the neck: a reduction in the need for operative exploration. J Trauma. 2008;64(6):1466-71. [ Links ]
10. Roon A, Christensen N. Evaluation and treatment of penetrating cervical injuries. J Trauma. 1997;19(6):391-7. [ Links ]
11. Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ. 2015;351:h5527. [ Links ]
12. Thoma M, Navsaria PH, Edu S, Nicol AJ. Analysis of 203 patients with penetrating neck injuries. World J Surg. 2008;32(12):2716-23. [ Links ]
13. Aiolfi A, Inaba K, Recinos G, et al. Non-iatrogenic esophageal injury: a retrospective analysis from the National Trauma Data Bank. World J Emerg Surg. 2017;12:19. [ Links ]
14. Madsen AS, Laing GL, Bruce JL, Oosthuizen GV, Clarke DL. An audit of penetrating neck injuries in a South African trauma service. Injury. 2016;47(1):64-9. [ Links ]
15. Makhani M, Midani D, Goldberg A, Friedenberg FK. Pathogenesis and outcomes of traumatic injuries of the esophagus. Dis Esophagus. 2014;27(7):630-6. [ Links ]
16. Patel MS, Malinoski DJ, Zhou L, Neal ML, Hoyt DB. Penetrating oesophageal injury: a contemporary analysis of the National Trauma Data Bank. Injury. 2013;44(1):48-55. [ Links ]
17. Asensio JA, Chahwan S, Forno W, et al. Penetrating esophageal injuries: multicenter study of the American Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2001;50(2):289-96. [ Links ]
18. Weigelt JA, Thal ER, Snyder WH, et al. Diagnosis of penetrating cervical esophageal injuries. Am J Surg. 1987;154(6):619-22. [ Links ]
19. Demetriades D, Theodorou D, Cornwell E, et al. Evaluation of penetrating injuries of the neck: prospective study of 223 patients. World J Surg. 1997;21(1):41-8. [ Links ]
20. Vassiliu P, Baker J, Henderson S, Alo K. Aerodigestive injuries of the neck. Am Surg. 2001;67(1):75. [ Links ]
21. Han SY, McElvein RB, Aldrete JS, Tishler JM. Perforation of the esophagus: correlation of site and cause with plain film findings. Am J Roentgenol. 1985;145(3):537-40. [ Links ]
22. Mazolewski PJ, Curry JD, Browder T, Fildes J. Computed tomographic scan can be used for surgical decision making in zone II penetrating neck injuries. J Trauma Acute Care Surg. 2001;51(2):315-9. [ Links ]
23. Inaba K, Munera F, McKenney M, et al. Prospective evaluation of screening multislice helical computed tomographic angio-graphy in the initial evaluation of penetrating neck injuries. J Trauma. 2006;61(1):144-9. [ Links ]
24. Inaba K, Branco BC, Menaker J, et al. Evaluation of multidetector computed tomography for penetrating neck injury: a prospective multicenter study. J Trauma Acute Care Surg. 2012;72(3):574-6. [ Links ]
25. Awais M, Qamar S, Rehman A, Baloch NUA, Shafqat G. Accuracy of CT chest without oral contrast for ruling out esophageal perforation using fluoroscopic esophagography as reference standard: a retrospective study. Eur J Trauma Emerg Surg. 2019;45(3):517-25. [ Links ]
26. Conradie WJ, Gebremariam FA. Can computed tomography esophagography reliably diagnose traumatic penetrating upper digestive tract injuries? Clin Imaging. 2015;39(6):1039-45. [ Links ]
27. Suarez-Poveda T, Morales-Uribe CH, Sanabria A, et al. Diagnostic performance of CT esophagography in patients with suspected esophageal rupture. Emerg Radiol. 2014;21(5):505-10. [ Links ]
28. Bodanapally UK, Shanmuganathan K, Dreizin D, et al. Penetrating aerodigestive injuries in the neck: a proposed CT-aided modified selective management algorithm. Eur Radiol. 2016;26(7):2409-17. [ Links ]
29. Madsen AS, Oosthuizen G, Laing GL, Bruce JL, Clarke DL. The role of computed tomography angiography in the detection of aerodigestive tract injury following penetrating neck injury. J Surg Res. 2016;205(2):490-8. [ Links ]
 Correspondence:
Correspondence:
email: barnardmaritz@gmail.com














