Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.58 n.4 Cape Town Dec. 2020
http://dx.doi.org/10.17159/2078-5151/2020/v58n4a3232
GENERAL SURGERY
Retrospective audit of laparoscopic inguinal hernia repair at a South African tertiary academic hospital
B Moodie; ZM Koto
Department of General Surgery, Sefako Makgatho Health Sciences University, South Africa
ABSTRACT
BACKGROUND: Adoption of laparoscopic inguinal hernia repair (LIHR) in sub-Saharan Africa is poor. The aim of this study was to describe our experience of the feasibility and short-term efficacy of the LIHR service at a South African tertiary academic hospital.
METHODS: A retrospective audit of all the adult, elective, laparoscopic inguinal hernia cases that were done between November 2011 and 31 October 2016. Data were collected regarding the patient demographics, index side of hernia, type of repair, conversion rate, peri- and postoperative complications, postoperative hernia recurrence, persistent groin pain for more than three months and procedure-related mortality.
RESULTS: One hundred and eighty-six patients were evaluated. One hundred and twenty-six (68%) patients were followed up for a mean of 38 months (3.1 years; range 9-67 months). Sixty (32%) patients were lost to follow-up. Early hernia recurrence (onset in < 7 days) occurred in one case after a totally extra-peritoneal (TEP) repair had required conversion to a trans-abdominal pre-peritoneal (TAPP) repair. Late recurrence (onset in > 7 days) occurred in seven TEP repair cases (5.6%). Four recurrences (57%) occurred within the first two years. Recurrences in the next three years showed a 59% reduction giving a recurrence rate of 2.9%. At follow-up, six TEP cases (4.8%) had persistent groin pain persisting for 3-6 months in two cases and for more than one year in four cases. Five cases had seroma, six scrotal haematoma and one port-site sepsis. No death occurred.
CONCLUSION: LIHR could be safely offered in a South African tertiary academic centre with acceptable results that are comparable with the South African private sector setting. LIHR could be implemented in other surgical training centres within a resource-limited environment.
Keywords: inguinal hernia, laparoscopic surgery, laparoscopy training, TAPP repair, TEP repair.
Introduction
Inguinal hernia repair represents one of the most common general surgical procedures, with approximately 20 million performed annually.1 One in four males will develop an inguinal hernia in his lifetime.2 Inguinal hernias account for 75% of all abdominal wall hernias.2 Laparoscopic inguinal hernia repair (LIHR) has been extensively evaluated and been shown to be a safe and effective repair approach.3,4In the hands of well-trained surgeons, the technique produces results equivalent to open repair.3,4 LIHR has been shown to require less postoperative analgaesia, cause less postoperative pain, require less time in hospital and allow return to work earlier.5-9 Despite the advances in laparoscopy, the open mesh-based tension-free inguinal hernia repair (OIHR) remains the criterion standard.3,4
In 2015, the reported utilisation of the LIHR technique was 64% in Germany, 55% in Australia, 45% in Switzerland, 45% in the Netherlands and 28% in Sweden.1 On the African continent, LIHR is still in its infancy with very few reported series in literature. The largest series was reported by McGuire et al., consisting of 507 cases in the South African private sector with results comparable with the best international series.10 Sherpiny from Egypt compared trans-abdominal pre-peritoneal (TAPP) to open repair in their setting and concluded that the TAPP repair approach is safe and now the preferred method of repair.11 Nana et al. from Cameroon and Shakya et al. from Nepal reported their initial experience with LIHR, showing good results.12,13 The authors highlighted the issues of the high cost of equipment and mesh as well as the lack of training as significant obstacles in their setting.12,13
The application of the LIHR approach in the South African tertiary public sector setting (academic training hospitals) has not yet been evaluated. The LIHR approach is taught at all the South African surgical training centres as a 'novel approach' in contrast to it being the primary preferred approach offered. This is due to widespread concerns about cost, the steep learning curve and initial increased operative time required to master the LIHR technique. The South African public health sector must provide an acceptable level of service delivery amidst significant challenges in the form of high patient load, time and staff constraints and budget considerations. In this setting, novel procedures with a steep learning curve often fall by the wayside.
The laparoscopic unit at the Dr George Mukhari Academic Hospital (DGMAH) was established towards the end of 2011 to focus on the development of minimal access surgery. As a result, residents and consultants are trained in a wide variety of routine laparoscopic procedures that has increased the numbers of laparoscopic procedures performed annually, leading to a steady rise in skill and competency of consultants, clinical fellows and surgical residents. Against this background this study aimed to describe our experience regarding the feasibility and efficacy of the LIHR at a tertiary academic hospital (DGMAH).
Methods
We conducted a retrospective audit of adult (> 18 years of age) elective primary LIHRs done since the inception of the dedicated laparoscopic unit at the DGMAH in November 2011 until 31 October 2016. DGMAH is a resource-limited public hospital on the outskirts of the capital city, Pretoria.
In the unit, all patients who present with a primary, elective, reducible inguinal hernia are allocated to the LIHR list. Emergency, irreducible and large inguinoscrotal hernias had open inguinal hernia repair. For training purposes and to keep the surgical backlog to a minimum, some of the potential LIHR cases were also allocated to the OIHR list (Figure 1).
Data were extracted from hospital patient records, theatre procedure records and the general surgery departmental database, and telephonic long-term follow-up interviews were conducted. Data were extracted regarding the patient demographics, index side of hernia, type of repair, peri- and postoperative complications (haemorrhage, haematoma, seroma, surgical site infection) postoperative hernia recurrence, persistent groin pain for more than three months and procedure-related mortality. Follow-up included a one week and one month outpatient visit followed by a long-term telephonic interview. Due to patient financial constraints and the distances that patients needed to travel to the hospital, long-term follow-up was problematic for most patients and could be done only via telephonic interview. Telephonic interviews were performed by the junior author and a senior surgical nurse. During the interview, the patient and operative details were confirmed. Patients were asked a standard set of questions about the duration of postoperative groin pain as well as the presence of persistent groin pain and hernia recurrence on the operated side. All patients with persistent postoperative groin pain and/or possible hernia recurrence (groin swelling/mass) on the operated side were asked to come in for assessment by the junior author at the surgical outpatient clinic.
Procedures
The procedures were performed by general surgery consultants assisted by surgical residents. At times the surgical consultant would allow a senior resident to perform part of the procedure under direct supervision, but the consultant always remained the primary surgeon for the case. The surgical techniques followed were the standard totally extra-peritoneal (TEP) repair and TAPP repair technique with laparoscopy stack, instrument set and minimal use of consumables. The procedures were done under general anaesthesia, with patients in supine position - arms tucked in and pressure points protected. The surgeon stood on the patient's side opposite the hernia with monitors at the feet side of the bed.
TEP repair14
An infra-umbilical incision was made to gain access to the sub-cutaneous tissue followed by exposure of the posterior rectus sheath. The laparoscope was used to develop the pre-peritoneal space and place two additional 5 mm ports under direct vision via a 10-12 mm port. The pre-peritoneal space was insufflated. The hernia was visualised and the inferior epigastric vessels, pubic symphysis, Cooper's ligament and the ilio-pubic tract were exposed by blunt dissection. The hernia was then reduced (direct, femoral, obturator) or dissected from the chord structures (indirect), taking care to avoid injury to the 'triangle of doom' structures (external iliac vessels, gonadal vessels and vas deference). A standard 15 cm x 10 cm mesh was introduced via the infra-umbilical port, positioned anteriorly along the pelvic wall and centred over the hernia defect. Mesh fixation was used where the surgeon preferred it. The pre-peritoneal space was then collapsed, ensuring adequate final mesh position as deflation proceeded and ports removed under direct vision followed by port defect skin closure.
TAPP repair14
An infra-umbilical incision was made to gain access to the rectus sheath and controlled peritoneal access gained under direct vision. A 10-12 mm port was placed and peritoneal cavity insufflated. A 30° scope was inserted, and two additional 5 mm ports were placed under vision in the midline. The hernia was visualised and the overlying peritoneum sharply incised 3-4 cm superiorly from the medial umbilical ligament to the anterior superior iliac spine. The dissection, hernia reduction, mesh placement and closure are identical to the TEP method described above.
Statistical analysis
Statistical analysis was performed with SPSS version 23 software. T-tests and chi-square tests were done to compare groups. A p-value of < 0.05 was considered significant. Categorical data are presented in a table and graphs.
Results
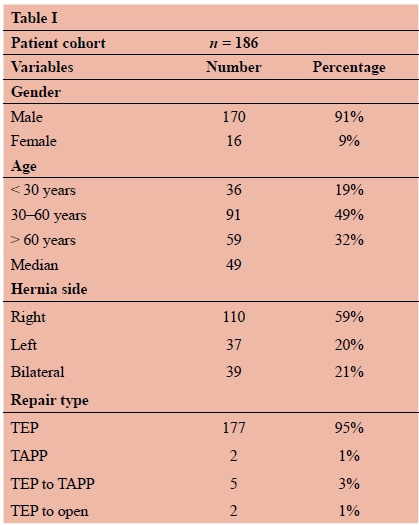
The general procedural information and patient demographics are shown in Table I. One hundred and eighty-six LIHR patients were evaluated and followed up. Sixty (32%) patients never returned for follow-up beyond the first seven days postoperative outpatient visit and could not be reached for a telephonic interview. One hundred and twenty-six (68%) patients were followed up for a mean of 38 months (3.1 years; range 9-67 months). Due to the significant number of patients who were lost to follow-up the outcomes in terms of recurrence rate, chronic postoperative groin pain and other long-term complications were determined only for the patient group with adequate follow-up. Early hernia recurrence (onset in < 7days) occurred in one case (0.8%) after a TEP repair had required conversion to a TAPP repair. Late recurrence (onset in > 7 days) occurred in seven TEP repair cases (5.6%). Four late hernia recurrences occurred within the first two years. Analysis of the subsequent three years showed a 59% reduction in late hernia recurrence, a rate of 2.9% (Figure 2).

Postoperative follow-up identified six TEP cases (4.8%) with persistent groin pain for more than three months postoperatively. Pain persisted for 3-6 months in two cases (1.6%) and in four cases for more than one year (3.2%) shown in Figure 2. Other complications included five cases of seroma (Clavien Dindo Ilia) that required aspiration and compressive dressings, six cases of scrotal haematoma (Clavien Dindo I) that resolved with conservative management, one case of port-site sepsis (Clavien Dindo II) that responded to systemic antibiotics, and no cases of procedure-related mortality.
Discussion
Inguinal hernia repair surgery is the most common procedure in general surgery globally, with 1.5 million repairs performed annually in the western world alone.15 In most countries, however, the Lichtenstein repair technique remains the technique of choice.1 This study intended to assess the feasibility and short term efficacy of the LIHR service at the DGMAH, which is a South African tertiary-level teaching hospital.
Our postoperative hernia recurrence rate of 5.6% is significantly higher than the < 1% rate reported by leading international units (median of 0.6%) as seen from 23 comparisons of TEP repair studies.1 The likely reasons for the higher recurrence rate include the initial procedural learning curve and the relatively low LIHR average annual case load of 37 in our unit. Another factor was that cases were performed by different consultant surgeon/resident combinations.
The incidence of clinically significant postoperative pain in our study group was 4.8%, which is well below the overall incidence of 10-12% reported in literature16-18 with no cases of debilitating pain. The overall complication rate was 9.7% and included cases of seroma, scrotal haematoma and port-site sepsis. Our results, specifically after the initial two years of our review period, were comparable to the largest published series from the South African private sector which showed a recurrence rate of 2.3% and an overall complication rate of 7.9%10 This is significant as there is a remarkable difference between the South African private and public sectors. Our results were also comparable to a smaller series from Egypt comparing LIHR with OIHR that showed a recurrence rate of 3.3% in their LIHR group.11
The LIHR techniques require specialised training and have a significant learning curve.1 A recent survey of 800 North American surgeons and residents revealed that 59% felt that they lacked the requisite training to perform LIHR.19,20 The data are concerning when bearing in mind that 25 years have passed since the introduction of LIHR. The learning curve is reported to be significant enough to prevent some surgeons from offering the repair approach to their patients.20,21 According to the HerniaSurge Group, it requires on average 50-100 TEP repairs by an individual surgeon to achieve outcomes similar to open anterior mesh repair with the first 30-50 being the most critical.1 Although these numbers cannot currently be attained by individual surgeons in our setting, we did observe a significant decrease in complication rates as experience increased. The significance of achieving a certain number has been reported by Voitk et al., who showed that complication rates decreased by 50% after a surgeon had gained the experience of the first 50 cases.19 Consultants and residents in our unit acquire laparoscopic skills and competency required for more advanced laparoscopic interventions in the armamentarium of the modern general surgeon by doing laparoscopic appendectomy, cholecystectomy and trauma laparoscopy.22,23 Our study shows that LIHR can be performed with an acceptable safety profile in our setting but caution should be exercised to reduce the hernia recurrence rate to the level of international standards. This could possibly be achieved as more experience is gained by continued adequate mentoring and supervision as part of a structured LIHR training programme as suggested by the Hernia Interest Group of South Africa and the European Hernia Society.24
In the early years of laparoscopy, Pallas et al. raised concerns about the pursuit of laparoscopic training and skill set acquisition in Africa and asked the question whether it is utopia or realism.25 Pallas et al. were sceptical and cautioned the clinician to bear in mind that techniques are still developing and therefore more costly to the local economy.25 They added that indications for LIHR should be carefully tailored to cope with local conditions and site-specific problems.25 Recently, Nsadi et al. from the DRC concluded that there is no reason to develop LIHR in developing countries due to cost and the challenges in learning and performing the procedure.26 These authors encourage surgeons and teaching institutions to focus their efforts on open repairs with commercial or low-cost mosquito net meshes.26
This study has several limitations that include its retrospective nature, significant loss to follow-up, telephonic interviews for the long-term follow-up and having the initial procedural 'learning curve' part of the review period. Despite these limitations this is the first audit of LIHR in the South African public service setting. It shows that LIHR can be safely offered in a South African tertiary academic centre with results that are comparable to the South African private sector setting. LIHR could be implemented in other surgical training centres within a resource-limited environment. Outcomes could, however, be improved to reach the level of leading international series.
Acknowledgements
The authors would like to thank Sr S Ndlovu, Mr Matlou Mabitsela, Prof. Herman Schoeman and Mrs Lene Kraft for their assistance, guidance and expertise with this research project and manuscript preparation.
Conflict of interest
The authors declare no conflict of interest.
Funding
None.
Ethical approval
Ethical approval was obtained from the Sefako Makgatho Health Sciences University Research Council: SMUREC/ M/315/2016:PG.
ORCID
Β Moodie https://orcid.org/0000-0002-1610-167X
ZM Koto https://orcid.org/0000-0002-9274-2508
REFERENCES
1. HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22:1-165. https://doi.org/10.1007/s10029-017-1668-x. [ Links ]
2. Jenkins JT, O'Dwyer PJ. Inguinal hernias. BMJ. 2008;336(76 38):269-72. https://doi.org/10.1136/bmj.39450.428275.AD. [ Links ]
3. Kuhry E, Van Veen RN, Langeveld HR, et al. Open or endoscopic total extraperitoneal inguinal hernia repair? A systematic review. Surg Endosc. 2007;21(2):161-6. https://doi.org/10.1007/s00464-006-0167-4. [ Links ]
4. Neumayer L, Giobbie-Hurder A, Jonasson O, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med. 2004;350(18):1819-27. https://doi.org/10.1056/NEJMoa040093. [ Links ]
5. Kark AE, Kurzer MN, Belsham PA. Three thousand one hundred seventy-five primary inguinal hernia repairs: advantages of ambulatory open mesh repair using local anesthesia. J Am Coll Surg. 1998;186(4):447-55; discussion 456. https://doi.org/10.1016/s1072-7515(98)00057-x. [ Links ]
6. Novitsky YW, Czerniach DR, Kercher KW, et al. Advantages of laparoscopic transabdominal preperitoneal herniorrhaphy in the evaluation and management of inguinal hernias. Am J Surg. 2007;193(4):466-70. https://doi.org/10.1016/j.amjsurg.2006.10.015. [ Links ]
7. Takata MC, Duh QY. Laparoscopic inguinal hernia repair. Surg Clin North Am. 2008;88(1):157-78. https://doi.org/10.1016/j.suc.2007.10.005. [ Links ]
8. Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR. Meta-analysis of randomised clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg. 2003;90(12):1479-92. https://doi.org/10.1002/bjs.4301. [ Links ]
9. McCormack K, Scott NW, Go PM, Ross S, Grant AM. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003. https://doi.org/10.1002/14651858.CD001785. [ Links ]
10. McGuire C, Baigrie IRJ, Theunissen D, Fernandes NL, Chapman RL. Outcome of laparoscopic inguinal hernia repair in a South African private practice setting. S Afr J Surg. 2012;50(4):115-18. https://doi.org/10.7196/sajs.1170. [ Links ]
11. Sherpiny WYE. Comparative study between laparoscopic trans abdominal preperitoneal and open mesh hernioplasty in repair of non-complicated inguinal hernia. Int Surg J. 2020;7(1):24-30. https://doi.org/10.18203/2349-2902.isj20195944. [ Links ]
12. Nana OB, Bang GA, Guifo ML, et al. Laparoscopic surgery for groin hernia in a third world country: a report of 9 cases of TAPP repair in Yacunde Camaroon. Pan Afr Med J. 2016;23:246. https://doi.org/10.11604/pamj.2016.23.246.8281. [ Links ]
13. Shakya VC, Shrestha ARM, Byanjankar B, Pandit R. Laparoscopic inguinal hernia repair: a prospective evaluation at Eastern Nepal. Pan Afr Med J. 2014;17:241. https://doi.org/10.11604/pamj.2014.17.241.2610. [ Links ]
14. Pallati P. Laparoscopic inguinal hernia repair. Available from: http://www.sages.org. Accessed 8 January 2020. [ Links ]
15. Bittner R, Arregui ME, Bisgaard T, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia repair (International Endohernia Society (IEHS). Surg Endosc. 2011;25:2773-843. https://doi.org/10.1007/s00464-011-1799-6. [ Links ]
16. Aasvang EK, Bay-Nielsen M, Kehlet H. Pain and functional impairment 6 years after inguinal herniorrhaphy. Hernia. 2006;10(4):316-21. https://doi.org/10.1007/s10029-006-0098-y. [ Links ]
17. Alfieri S, Amid PK, Campanelli G, et al. International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 2011;15(3):239-49. https://doi.org/10.1007/s10029-011-0798-9. [ Links ]
18. Nienhuijs SW, Rosman C, Strobbe LJA, Wolff A, Bleichrodt RP. An overview of the features influencing pain after inguinal hernia repair. Int J Surg. 2008;6(4):351-6. https://doi.org/10.1016/j.ijsu.2008.02.005. [ Links ]
19. Voitk AJ. The learning curve in laparoscopic inguinal hernia repair for the community general surgeon. Can J Surg. 1998;42(6):446-50. PMID: 9854534. PMCID: PMC3949801. [ Links ]
20. Zahiri HR, Park AE, Pugh CM, Vassiliou M, Voeller G. " See one, do one, teach one": inadequacies of current methods to train surgeons in hernia repair. Surg Endosc Other Interv Tech. 2015;29(10):2867-72. https://doi.org/10.1007/s00464-015-4411-7. [ Links ]
21. Trevisonno M, Kaneva P, Watanabe Y, et al. A survey of general surgeons regarding laparoscopic inguinal hernia repair: practice patterns, barriers and educational needs. Hernia. 2015;19(5):719-24. https://doi.org/10.1007/s10029-014-1287-8. [ Links ]
22. Pandey S, Slavic S, Cross K, Soulsby R, Pullyblank AM. Laparoscopic appendectomy: a training model for laparoscopic right hemicolectomy? Colorectal Disease. 2007;9:536-9. https://doi.org/10.1111/j.1463-1318.2007.01244.x. [ Links ]
23. Man E, Nemeth T, Geczi T, Simonka Z, Lazar G. Learning curve after rapid introduction of laparoscopic appendectomy: are there any risks in surgical resident participation? World J Emerg Surg. 2016;11:17. https://doi.org/10.1186/s13017-016-0074-5. [ Links ]
24. Simonds MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13:33-403. https://doi.org/10.1007/s10029-009-0529-7. [ Links ]
25. Pallas G, Simon F, Sockeel P, Chapuis O, Jancovici R. Inguinal hernia in Africa and laparoscopy: utopia or realism? Med Trop. 2000 Mar;60(4):389-94. PMID: 11436598. [ Links ]
26. Nsadi B, Detry O, Arung W. Inguinal hernia surgery in developing countries: should laparoscopic repairs be performed? Pan Afr Med J. 2017;27:5. https://doi.org/10.11604/pamj.2017.27.5.12358. [ Links ]
 Correspondence:
Correspondence:
email: drbenmoodie@icloud.com














