Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.58 no.3 Cape Town sep. 2020
LETTER TO THE EDITOR
A step in the right direction for end-stage kidney disease in South Africa
T du Toit
Transplant Unit, Division of General Surgery, Department of Surgery, Faculty ofHealth Sciences, Groote Schuur Hospital and University of Cape Town, South Africa
The Vascular Society of Southern Africa (VASSA) should be commended on the publication of clinical practice guidelines to assist healthcare professionals caring for patients with chronic kidney disease and their dialysis access. The guidelines provide an important and sound framework to facilitate clinical decision-making and should be welcomed.
Chronic kidney disease (CKD) in South Africa (SA) is on the increase and has become one of the leading causes of mortality, accounting for an estimated 1 000 deaths per million population (pmp) annually.1 An exponential rise in CKD in sub-Saharan Africa is projected over the next decade due to the escalating dual burden of communicable diseases, such as infectious glomerulonephritis and HIV, and non-communicable diseases associated with an aging population, lifestyle changes, obesity and rapid urbanisation.2
For the majority of patients who have progressed to end-stage kidney disease (ESKD), kidney transplantation will improve survival, decrease cost and improve quality of life compared to dialysis.3 However, with a low annual kidney transplant rate of 4.6 pmp, predominantly limited by a low annual deceased donor rate of 1.7 pmp, most patients with ESKD in SA depend heavily on the safe and effective administration of dialysis to achieve long-term survival.4 Within this context, the implementation of clinical practice guidelines, quality assessment, research and education in the field of dialysis access might be considered even more crucial and relevant in SA than in countries with better access to transplantation.
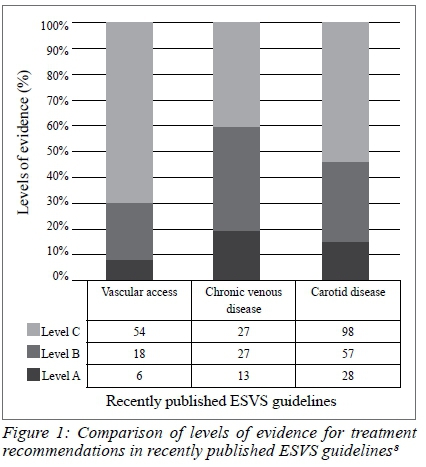
The projected number of patients receiving dialysis worldwide is set to double from 2.61 million in 2010, to 5.44 million in 2030.5 In contrast, downward trends in abdominal aortic aneurysm disease and peripheral bypass surgery have been observed in certain regions.6,7 However, on review of recently published guidelines by the European Society for Vascular Surgery (ESVS), 70% of vascular access recommendations were based on expert opinion (Level C evidence), as opposed to 40% of chronic venous disease, 47% of carotid disease and 51% of peripheral arterial disease recommendations (Figure 1).8 Similarly, 58% of the recommendations included in the VASSA guidelines are based on Level C evidence. The field of dialysis access deserves robust scientific evidence to direct future best practice guidelines.
Multiple international societies have published guidelines on the management of dialysis access. The most recent of these, and arguably the most comprehensive, is an update on the 2006 National Kidney Foundation - Kidney Disease Outcomes Quality Initiative (NKF-KDOQI) guidelines published earlier this year.9 Although the majority of these recommendations can be applied to the South African setting, it is essential to identify and engage the specific challenges unique to SA.
Although vascular surgeons are undoubtedly best equipped to manage vascular access, there is only approximately one vascular surgeon pmp in SA. Vascular services are unevenly distributed and often concentrated in larger, metropolitan areas. In order to reach 278 dialysis units and 8 881 patients across SA and to keep up with future demand, a thoughtful strategy that includes general surgeons needs to be outlined and implemented. Training of general surgery registrars in vascular access needs to be prioritised. Dialysis access procedures should provide crucial training opportunities when appropriately selected and properly supervised, without detriment to the patient.10
The marked disparity in healthcare resources between the public and private sector has been previously described and is particularly acute in relation to accessing dialysis services. In 2017, the treatment rate of ESKD patients in the public sector was 66 pmp, compared to 855 pmp in the private sector.4 Between 1994 and 2017, the number of private dialysis units dramatically increased from 5 to 249 while the number of public sector units remained essentially unchanged (26 to 29).4 Best practice in the management of dialysis access should not differ between sectors. Due to rising healthcare costs, both public and private sector practitioners have a responsibility to offer the most cost-effective treatment. The concept of value, defined as improved outcome at an equal or lower cost, has not received the focus it deserves and studies with value-based endpoints should be prioritised.
Peritoneal dialysis (PD) offers a survival benefit during the first 1.5-2 years, with higher patient satisfaction and lower cost compared to haemodialysis.11 Notably, the proportion of dialysis patients receiving PD in the private sector (5.7%) is far below that of the public sector (38.8%).4 Further studies are needed to clarify the reasons for this phenomenon.
The recently updated NKF-KDOQI guidelines have emphasised the importance of establishing an ESKD Life-Plan, contingency plan and succession plan for each patient receiving or nearing dialysis.9 In other words, we should not only focus on which access option should be performed first, but always consider which option could be next. The placement of covered stents to manage outflow vein stenosis or occlusion (cephalic arch, graft-vein interface, central veins) should be performed with caution as to ensure the preservation of future access options in keeping with the patient's Life-Plan.
Undoubtedly, clinical practice guidelines can improve the quality of dialysis, decrease associated morbidity and mortality and improve the quality of life of ESKD patients. However, one should not underestimate the challenge that the implementation of guidelines across healthcare sectors, hospital groups and medical and surgical specialities might pose. Those involved in managing dialysis access should use these guidelines as a framework for best practice, while remaining aware of the paucity of high quality evidence and the need to work together in a coordinated fashion to address the evidence gaps.
REFERENCES
1. Mayosi BM, Lawn JE, Van Niekerk A, et al. Health in South Africa: Changes and challenges since 2009. Lancet. 2012;380(9858):2029-43. https://doi.org/10.1016/S0140-6736(12)61814-5. [ Links ]
2. Stanifer JW, Jing B, Tolan S, et al. The epidemiology of chronic kidney disease in sub-Saharan Africa: a systematic review and meta-analysis [published correction appears in Lancet Glob Health. 2014 May;2(5):266]. Lancet Glob Health. 2014;2(3):e174-e181. https://doi.org/10.1016/S2214-109X(14)70002-6. [ Links ]
3. Purnell TS, Auguste P, Crews DC, et al. Comparison of life participation activities among adults treated by hemodialysis, peritoneal dialysis, and kidney transplantation: a systematic review. Am J Kidney Dis. 2013;62(5):953-73. https://doi.org/10.1053/j.ajkd.2013.03.022. [ Links ]
4. Davids MR, Jardine T, Marais N, et al. South African Renal Registry Annual Report 2017. Afr J Nephrol. 2019;22(1):60-71. https://doi.org/10.21804/22-1-3810. [ Links ]
5. Liyanage T, Ninomiya T, Jha V, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385(9981):1975-82. https://doi.org/10.1016/S0140-6736(14)61601-9. [ Links ]
6. Persson SE, Boman K, Wanhainen A, et al. Decreasing prevalence of abdominal aortic aneurysm and changes in cardiovascular risk factors. J Vasc Surg. 2017;65(3):651-8. https://doi.org/10.1016/j.jvs.2016.08.091. [ Links ]
7. Goodney PP, Beck AW, Nagle J, et al. National trends in lower extremity bypass surgery, endovascular interventions, and major amputations. J Vasc Surg. 2009;50(1):54-60. https://doi.org/10.1016/j.jvs.2009.01.035. [ Links ]
8. Argyriou C, Georgiadis GS, Lazarides MK. Vascular access guidelines: do we need better evidence? Eur J Vasc Endovasc Surg. 2018;56(4):608. https://doi.org/10.1016/j.ejvs.2018.05.031. [ Links ]
9. Lok CE, Huber TS, Lee T, et al; KDOQI Vascular Access Guideline Work Group. KDOQI clinical practice guideline for vascular access: 2019 update. Am J Kidney Dis. 2020;75(4) (suppl 2):S1-S164. [ Links ]
10. Gundevia Z, Whalley H, Ferring M, et al. Effect of operating surgeon on outcome of arteriovenous fistula formation. Eur J Vasc Endovasc Surg. 2008;35(5):614-8. https://doi.org/10.1016/j.ejvs.2007.11.018. [ Links ]
11. Sinnakirouchenan R, Holley JL. Peritoneal dialysis versus hemodialysis: risks, benefits, and access issues. Adv Chronic Kidney Dis. 2011;18(6):428-32. https://doi.org/10.1053/j.ackd.2011.09.001. [ Links ]
 Correspondence:
Correspondence:
Email: tinus.dutoit@uct.ac.za














