Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.58 no.3 Cape Town sep. 2020
http://dx.doi.org/10.17159/2078-5151/2020/v58n3a3341
TRAUMA SURGERY
Procalcitonin-guided antibiotic therapy for suspected and confirmed sepsis of patients in a surgical trauma ICU: a prospective, two period cross-over, interventional study
RN ChombaI, II; MS MoengIII; W LowmanIV, V
INational Health Laboratory Services, South Africa
IIFaculty of Health Sciences, Helen Joseph Academic Hospital, University of the Witwatersrand, South Africa
IIIDepartment of Surgery, Faculty of Health Sciences, Charlotte Maxeke Johannesburg Academic Hospital, University of the Witwatersrand, South Africa
IVPathcare/Vermaak and Partners Pathologists, South Africa
VFaculty of Health Sciences, Wits Donald Gordon Medical Centre, University of the Witwatersrand, South Africa
ABSTRACT
BACKGROUND: Biomarkers like procalcitonin (PCT) are an important antimicrobial stewardship tool for critically ill patients. There is little evidence regarding the use of PCT-guided antibiotic algorithms in developing countries. Evidence is also lacking for PCT-based antibiotic algorithms in surgical trauma patients admitted to the intensive care unit (ICU).
METHODS: A prospective, two period cross-over study was conducted in a surgical trauma intensive care unit in South Africa. In the first period, 40 patients were recruited into the control group and antibiotics were discontinued as per standard of care. In the second period, 40 patients were recruited into the procalcitonin group and antibiotics were discontinued if the PCT decreased by > 80% from the peak PCT level, or to an absolute value of less than 0.5 μg/L. Antibiotic duration of treatment was the primary outcome. Patients were followed up for 28 days from the first sepsis event.
RESULTS: For the first sepsis event the PCT group had a mean antibiotic duration of 9.3 days while the control group had a mean duration of 10.9 days (p = 0.10). Patients in the intervention group had higher mean (SD) antibiotic free days alive of 7.7 (6.57) days compared to the control group mean (SD) of 3.8 (5.22) days, (p = 0.004). In-hospital mortality rate was lower in the intervention group (15%) compared to the control group (30%) and was statistically significant (p = 0.045).
CONCLUSION: There was no significant difference in duration of antibiotic treatment between the two groups. However, the PCT group had more antibiotic free days alive and lower in-hospital mortality compared to the control group.
Keywords: procalcitonin, trauma, sepsis, intensive care unit
Introduction
The world is facing increasing rates of multidrug resistant bacteria in all hospitals, predominantly in intensive care units (ICUs). Over-use of antibiotics is a major factor driving antibiotic resistance. There is an urgent need to implement antibiotic stewardship in ICUs to reduce antibiotic overuse. The role of biomarkers, especially procalcitonin (PCT), as antibiotic stewardship tools has been investigated in several trials.13 PCT levels are usually low in normal conditions but increase in severe infections and inflammatory conditions. However, the highest levels are found in septic patients. Procalcitonin rises within a few hours of infection with bacteria but reduces with appropriate antibiotic therapy.4 PCT has been used in clinical trials as a tool for monitoring clinical response to antibiotic treatment. Antibiotics are discontinued once the PCT drops to a predetermined level.2,3,5 Antibiotic protocols can prevent antibiotic misuse by guiding safe discontinuation in patients who have had adequate antimicrobial therapy.
Early studies on PCT-guided antibiotic treatment were mostly in primary care patients with pneumonia.5,6 In the ICU setting PCT has been used mainly as part of an algorithm to discontinue antibiotics.127 Studies have proven the efficacy of PCT algorithms in reducing antibiotic duration of treatment and achieving significant cost savings without an increase in adverse outcomes.810
Studies on PCT-guided antibiotic therapy are mainly from Europe. There are few studies from developing countries on the use of PCT-based algorithms for antibiotic stewardship. Most ICU studies contain relatively few numbers of surgical patients with inconclusive evidence in trauma patients but a recent study from South Africa investigated the diagnostic role of PCT in predicting bacteraemia in trauma ICU patients.11 The aim of our study was to determine if a PCT-based clinical algorithm would decrease total antibiotic days compared to standard antibiotic treatment in surgical trauma patients in an ICU setting. It was useful to perform a study to analyse the use of PCT algorithms specifically in surgical trauma patients in South Africa, where antibiotic stewardship programs are not yet well established.
Methods
We conducted a prospective, two-period cross-over case-controlled, interventional study in the trauma ICU at Charlotte Maxeke Hospital, Johannesburg, South Africa. Eighty patients were recruited from April 2014 to July 2015. Adult patients in the trauma ICU with suspected sepsis that were either not on antibiotics or had been on antibiotic therapy for less than 48 hours were approached for consent. Patients were recruited consecutively until the sample size was achieved.
All patients in the PCT group had a serum PCT done at study recruitment and then every 48 hours until antibiotics were discontinued. PCT was not used to guide antibiotic treatment in the control group.
Inclusion criteria
Patients above the age of 18 years admitted to the trauma ICU with suspected or confirmed bacterial sepsis with written consent and who survived more than 48 hours after study inclusion.
Exclusion criteria
Exclusions included patients in whom consent could not be obtained, pregnancy, patients requiring prolonged antibiotic therapy and those who had severe comorbidities, e.g. congestive cardiac failure, cirrhosis, insulin dependent diabetes, renal failure requiring dialysis, and advanced human immunodeficiency virus (HIV) infection with CD4 < 100 cells^L. Patients who had received more than 48 hours of antibiotics before study enrolment and those with poor chance of survival, e.g. injury severity score (ISS) > 45, critical or untreatable injury at screening were also excluded.
Control period
Prior to the study antibiotics were given empirically according to the site-specific ICU algorithm and always covering at least the spectrum of previously prescribed antimicrobials as well as expected organisms. The normal duration of antibiotics was usually 7 days but could be prolonged to 14 days depending on the cultured organism and site of infection. Piperacillin-tazobactam was commonly used as empiric treatment for nosocomial sepsis while amoxicillin-clavulanate was usual for community acquired infections. Antibiotics were changed to cover the spectrum of organisms cultured from the site of sepsis. The control period was between April 2014 and January 2015. Forty patients with suspected or confirmed sepsis were recruited consecutively into the control group. Antibiotics were given as per the ICU protocol above. Decisions regarding discontinuation of antibiotic treatment were left at the attending doctor's discretion.
Intervention period
In the intervention period, forty patients with confirmed or suspected sepsis were recruited consecutively into the intervention group between February 2015 and July 2015. The PCT level was measured at study recruitment and then on alternate days. Antibiotics were given as per the ICU protocol discussed above. If the PCT decreased to an absolute value of less than 0.5 μg/L or by > 80% from the peak PCT concentration, clinicians were encouraged to stop antibiotics. This algorithm was based on pre-existing interventional PCT studies. Antibiotics were not stopped if there were ongoing signs of sepsis (e.g. temperature > 38.3 °C) with an obvious source of sepsis. The PCT complemented but did not replace clinical decision making and clinicians were able to deviate from the PCT algorithm if the need arose. Although clinicians were encouraged to stop antibiotics according to this PCT algorithm the decision to stop was at the discretion of the attending clinician. This was due to patient safety concerns as no clinical study has based antibiotic discontinuation exclusively on a biomarker.
Laboratory methods
The PCT in patient serum was measured on the ADVIA Centaur® BRAHMS PCT assay (Siemens Healthcare Diagnostics Inc., Muenchen, Germany). The assay has a measurement range of 0.02-75 μg/L and analytical sensitivity of 0.02 μg/L.
Microbiological specimens were processed according to standard microbiological procedures. Identification and antimicrobial susceptibility testing (AST) of cultured organisms was performed on the Vitek®2 instrument (bioMérieux Inc., Durham, NC, USA). Alternatively, AST was performed by disc diffusion or E-test® strips (bioMérieux S.A., Marcy l'Étoile, France). All AST results were interpreted according to the Clinical and Laboratory Standards Institute guidelines (CLSI, Wayne, PA, USA) current at the time.
Study outcomes
The primary outcome was to determine if a PCT-based antibiotic algorithm would decrease total antibiotic days compared to standard antibiotic treatment in surgical trauma patients in an ICU setting. Secondary outcomes included antibiotic free days alive at 28 days from study inclusion, in-hospital mortality (death from any cause), ICU length of stay and recurrence or relapse of infection.
Statistical analysis
In calculating the sample size, a difference of 2 days' antibiotic duration between the mean in one group and the mean in the other group (μ1-μ2) of 2 days would be significant. It was determined that 40 patients were needed in each group to detect a significant difference.
Comparisons were made between the two groups using mean (standard deviation) and t-test for continuous variables. The p-value was determined by a chi-square but if the number of items constituting a variable was less than 10 then the p-value was calculated using the Fisher's exact test. Statistical significance was considered for two-sided p < 0.05. Categorical variables were compared using percentages.
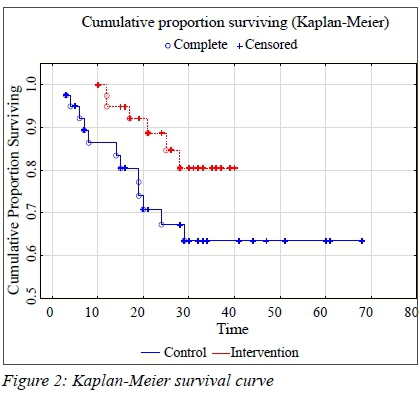
Diversity between study groups was determined using chi-square test and Fisher's exact test as appropriate. Risk ratio for death and infectious complications (relapse) were calculated at the 95% confidence interval. Kaplan-Meier survival curves were evaluated by the log-rank test. A multivariate analysis was not undertaken due to the small number of study subjects. Data was analysed using Statistica™ version 13.2 (TIBCO software Inc., Palo Alto, CA, USA).
Results
General characteristics of the study population
The two groups were well matched in terms of baseline demographics as shown in Table I. There was no significant difference in other markers of sepsis severity, e.g. the sequential organ failure assessment (SOFA) score, baseline temperature and white cell counts. The PCT group, however, had a worse injury severity score (ISS) than the control group. A baseline PCT was considered unnecessary in the control group, hence only 10 patients in the control group had a baseline PCT done (p = 0.04).
There were 8 patients (20%) in the control group who needed inotrope support for the first episode of sepsis compared to 5 patients (12.5%) in the intervention group. The main source of sepsis in both groups was pulmonary (Table I).
Microbiology culture findings
The most commonly isolated organism in both groups of patients was extended spectrum beta lactamase (ESBL) producing Klebsiella pneumoniae (Figure 1). The control group had more patients with negative cultures compared to the PCT group (6 patients vs 2 patients). The PCT group had a slightly higher number of Pseudomonas aeruginosa infections (3 patients vs 8 patients).
The most commonly used empiric antibiotic was piperacillin-tazobactam (PT). There were 16 patients in the control group and 36 patients in the PCT group who received PT as empiric therapy. Carbapenems were more likely to be given empirically in the control group (9 patients) compared to the PCT group (1 patient).
When empiric antibiotics were assessed in terms of appropriateness to the cultured organism, it was found that an equal number of patients in each group (n = 16) received appropriate empiric treatment. There were more patients in the PCT group who received inappropriate empiric antibiotics (22 patients) compared to the control group (17 patients) but the difference was not statistically significant (p = 0.59).
Primary outcome
When duration of therapy for the first sepsis episode was compared between groups, the PCT group had a shorter mean (SD) duration of treatment of 9.3 (5.67) days compared to the control group mean (SD) of 10.9 (2.62) days. This difference, however, did not reach statistical significance (p = 0.10).
There were an almost equal number of patients in both groups who were treated for a second episode of sepsis (14 patients in PCT group vs 15 patients in the control group). The mean (SD) duration of treatment for the second episode of sepsis was shorter in the PCT group 9.6 (2.61) days compared to the control group mean (SD) of 12.0 (4.62) day s but the difference did not reach statistical significance (p = 0.09).
Clinician compliance to the PCT algorithm, i.e. antibiotics stopped within 24 hours of reaching the stopping criteria, was 62.5%. In those who were non-compliant 80% oC patients had their antibiotics stopped within 3 days of reaching the stopping criteria.
Secondary outcomes
Patients in the PCT group had more antibiotic free days alive with mean (SD) of 7.7 (6.57) days compared to the control group mean (SD) of 3.8 (5.22) days (p = 0.004).
Only 2 patients (5%) in the intervention group had a relapse of infection compared to 9 patients (22.5%) in the control group (p = 0.02).
There was no difference in mean (SD) length of ICU stay in the PCT group compared to the control group, 16.1 (8.31) days vs 17.6 (13.84) days (p = 0.5). The PCT group had a slightly longer mean (SD) hospital stay of 25.4 (8.32) days compared to the control group mean of 24.5 (17.03) days. The difference was not statistically significant (p = 0.76).
The PCT group had fewer in-hospital deaths (6 patients, 15%) compared to the control group (12 patients, 30%). Survival between the two groups was compared using Kaplan-Meier analysis as shown in Figure 2. The PCT group had improved survival compared to the control group (Wilcoxon log rank analysis p = 0.045).
Discussion
In this single centre study, a PCT based algorithm failed to demonstrate a reduction in duration of antibiotic treatment in surgical trauma patients. The PCT group had shorter duration of treatment for both the first and second episode of sepsis compared to the control group, but this did not translate into a statistically significant difference. This is in contrast to other studies which found that use of a PCT based antibiotic algorithm reduced duration of antibiotics in critically ill septic patients.2712 This difference is possibly due to poor clinician compliance with a PCT algorithm. Due to safety concerns, experts agree that the decision to stop antibiotics based on a PCT algorithm cannot be enforced and should be supported by clinical judgement.3,13
However, an important finding of this study was a significant increase in antibiotic-free days alive at 28 days in the PCT group compared to controls. Other researchers have reported similar findings. In one such study, 101 patients were randomised to either a PCT group or a control group. The PCT group had more antibiotic-free days alive (13 days) compared to the control group (9.5 days).14 In one systematic review of six ICU studies, there was a 23-37% increase in antibiotic-free days alive in the PCT group compared to the control group.15 Our results show that the PCT group had lower in-hospital mortality compared to controls. Similarly, other authors report reduced mortality in the PCT group compared to the control group.1,316 A recent meta-analysis however, failed to demonstrate reduction in mortality in critically ill septic patients using PCT-guided antibiotic therapy.17 The reduction in mortality and increased antibiotic-free days alive in our study may be due to improved management of septic episodes. Use of a PCT algorithm facilitates decisions around antimicrobial therapy, whereby initiation of antibiotics and evaluation of treatment response is guided not only by clinical judgement but also by an objective laboratory biomarker.
Our study found a small but insignificant reduction in ICU stay in the PCT group. The effects of a PCT-based algorithm on length of ICU stay are not very clear when compared across different studies. One study found a significantly shortened ICU stay in the PCT group compared to the control group.7 Another study however, found that length of ICU stay was one day longer in patients in the PCT arm compared to the standard-of-care arm.18 That particular study differs from other studies because it used an algorithm of PCT-guided antibiotic escalation which prolonged ICU admission without improving survival. A meta-analysis of seven studies comprising 1 075 patients with septic shock or severe sepsis compared PCT-guided antibiotic treatment to standard of care.19 It reported no appreciable difference in ICU length of stay between the PCT and the control groups. The effect of a PCT-based antibiotic algorithm on length of ICU stay is therefore still open to debate.
Our results showed no difference in hospital stay between the PCT and control groups. Other authors have similarly found no difference in duration of hospital stay when comparing PCT-guided strategies to standard of care.1,3, 19, 20
A major concern whilst using a PCT algorithm to discontinue antibiotics is the potential for relapse if infections are inadequately treated. Our study showed a lower relapse rate in the PCT group compared to the control group. Patients in the PCT group may have benefited from a more focused assessment and vigorous source control leading to the lower relapse rate, which again highlights the potential of a PCT algorithm in management of septic patients. A meta-analysis of 14 trials where patients were assigned to receive antibiotics based on a PCT algorithm similarly found decreased risk of treatment failure in patients assigned to the PCT group.21 Some authors report no difference in relapse rates when comparing PCT group to controls.7 One study, however, found that re-institution of antibiotics for relapse was more common in the PCT group than in the control group but the numbers were small in both instances (5% vs 3%).3
To our knowledge, this is the first prospective study evaluating the value of a PCT-based algorithm in reducing antibiotic duration of treatment in surgical trauma ICU patients.
Our study had several limitations; firstly, it was a single centre, non-randomised study. The results of this study may be biased by non-randomisation and may not be extrapolated to patients with a different background. Since this was a single centre study, a crossover design was best suited to the study aims. Secondly, the sample size was calculated to have sufficient power to detect a between-group difference of at least two days in antibiotic duration of treatment. It is likely that a larger sample size would have detected a statistically significant difference between groups with the results that we obtained. The small sample also precluded a multivariate analysis. Thirdly, poor compliance by clinicians to a PCT algorithm may have resulted in a conservative bias and reduced the potential benefits of a PCT-guided algorithm. Fourthly, our definition of relapse was defined using microbiologic criteria. Patients who were discharged home or transferred out may have suffered a late relapse that was underestimated in our study. Finally, our study did not measure the actual reduction in antibiotic costs associated with a PCT algorithm. Other studies have reported a decline in antibiotic costs using PCT algorithms, without any associated adverse outcomes.10,22
Conclusion
Our study showed that PCT has the potential to reduce the duration of antibiotics for surgical trauma patients with suspected and confirmed sepsis. Although not reaching statistical significance, the PCT group had reduced duration of antibiotic treatment for both the first and the second episode of sepsis. We observed a significant increase in antibiotic free days alive, improved hospital survival and a lower infection relapse rate for patients managed according to a PCT algorithm. This reduction in antibiotic usage has the added potential benefit of reducing antibiotic costs. PCT can be measured on alternate days or at longer intervals in resource limited settings to reduce costs while still retaining the observed benefits. The potential of PCT-guided regimens to reduce mortality and increase survival is difficult to quantify in terms of cost benefit and needs to be explored in further studies.
Conflict of interest
The authors declare that they have no competing interests.
Funding source
No funding was required.
Ethical approval
The research protocol was approved by the Human Research Ethics Committee (HREC) of the University of the Witwatersrand. The ethics clearance certificate number is M130860.
ORCID
RN Chomba © https://orcid.org/0000-0003-3147-6688
MS Moeng © https://orcid.org/0000-0001-7459-3388
W Lowman © https://orcid.org/0000-0002-6981-389X
REFERENCES
1. Bouadma L, Luyt C-E, Tubach F, et al. Use of procalcitonin to reduce patients' exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 2010 Feb 6;375(9713):463-74. https://doi.org/10.1016%2FS0140-6736(09)61879-1. [ Links ]
2. Hochreiter M, Köhler T, Schweiger AM, et al. Procalcitonin to guide duration of antibiotic therapy in intensive care patients: a randomised prospective controlled trial. Crit Care. 2009;13(3):R83. https://doi.org/10.1186%2Fcc7903. [ Links ]
3. De Jong E, Van Oers JA, Beishuizen A, et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis. 2016 Jul;16(7):819-27. https://doi.org/10.1016%2FS1473-3099(16)00053-0. [ Links ]
4. Becker KL, Snider R, Nylen ES. Procalcitonin in sepsis and systemic inflammation: a harmful biomarker and a therapeutic target. Br J Pharmacol. 2010 Jan 1;159(2):253-64. https://doi.org/10.1111%2Fj.1476-5381.2009.00433.x. [ Links ]
5. Christ-Crain M, Jaccard-Stolz D, Bingisser R, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet. 2004 Feb 21;363(9409):600-7. https://doi.org/10.1016%2FS0140-6736(04)15591-8. [ Links ]
6. Briel M, Schuetz P, Mueller B, et al. Procalcitonin-guided antibiotic use vs a standard approach for acute respiratory tract infections in primary care. Arch Intern Med. 2008 Oct 13;168(18):2000-7. https://doi.org/10.1001%2Farchinte.168.18.2000. [ Links ]
7. Nobre V, Harbarth S, Graf J-D, Rohner P, Pugin J. Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomised trial. Am J Respir Crit Care Med. 2008 Mar 1;177(5):498-505. https://doi.org/10.1164%2Frccm.200708-1238OC. [ Links ]
8. Broyles MR. Impact of procalcitonin-guided antibiotic management on antibiotic exposure and outcomes: real-world evidence. Open Forum Infect Dis. 2017;4(4):ofx213. https://doi:10.1093/ofid/ofx213. [ Links ]
9. Wirz Y, Meier MA, Bouadma L, et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: a patient-level meta-analysis of randomised trials. Crit Care. 2018 Aug 15;22(1):191. https://doi:10.1186/s13054-018-2125-7. [ Links ]
10. Schuetz P, Balk R, Briel M, et al. Economic evaluation of procalcitonin-guided antibiotic therapy in acute respiratory infections: a US health system perspective. Clin Chem Lab Med. 2015 Mar;53(4):583-92. https://doi.org/10.1515/cclm-2014-1015. [ Links ]
11. Ramasawmy D, Pillay M, Hardcastle TC. Correlation of procalcitonin to positive blood culture results in a sample of South African trauma ICU patients between 2016 and 2017. Eur J Trauma Emerg Surg. 2020 Jan 2. https://doi.org/10.1007/s00068-019-01295-y. [ Links ]
12. Albrich WC, Dusemund F, Bucher B, et al. Effectiveness and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections in "real life": an international, multicenter poststudy survey (ProREAL). Arch Intern Med. 2012 May 14;172(9):715-22. https://doi.org/10.1001%2Farchinternmed.2012.770. [ Links ]
13. Bartoletti M, Antonelli M, Bruno Blasi FA, et al. Procalcitonin-guided antibiotic therapy: an expert consensus. Clin Chem Lab Med. 2018 26;56(8):1223-9. https://doi.org/10.1515/cclm-2018-0259. [ Links ]
14. Stolz D, Smyrnios N, Eggimann P, et al. Procalcitonin for reducedantibioticexposure in ventilator-associatedpneumonia: a randomised study. Eur Respir J. 2009 Dec;34(6):1364-75. https://doi.org/10.1183%2F09031936.00053209. [ Links ]
15. Agarwal R, Schwartz DN. Procalcitonin to guide duration of antimicrobial therapy in intensive care units: a systematic review. Clin Infect Dis. 2011 Aug;53(4):379-87. https://doi.org/10.1093%2Fcid%2Fcir408. [ Links ]
16. Schuetz P, Wirz Y, Sager R, et al. Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: a patient level meta-analysis. Lancet Infect Dis. 2018 Jan;18(1):95-107. https://doi.org/10.1016/S1473-3099(17)30592-3. [ Links ]
17. Peng F, Chang W, Xie J-F, et al. Ineffectiveness of procalcitonin-guided antibiotic therapy in severely critically ill patients: a meta-analysis. Int J Infect Dis. 2019 Aug 1;85:158-66. https://doi.org/10.1016/jijid.2019.05.034. [ Links ]
18. Jensen JU, Hein L, Lundgren B, et al. Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: a randomised trial. Crit Care Med. 2011 Sep;39(9):2048-58. https://doi.org/10.1097%2FCCM.0b013e31821e8791. [ Links ]
19. Prkno A, Wacker C, Brunkhorst FM, Schlattmann P. Procalcitonin-guided therapy in intensive care unit patients with severe sepsis and septic shock-- a systematic review and meta-analysis. Crit Care. 2013 Dec 11;17(6):R291. https://doi.org/10.1186%2Fcc13157. [ Links ]
20. Lam SW, Bauer SR, Fowler R, Duggal A. Systematic review and meta-analysis of procalcitonin-guidance vs. usual care for antimicrobial management in critically ill patients: focus on subgroups based on antibiotic initiation, cessation, or mixed strategies. Crit Care Med. 2018 May;46(5):684-90. https://doi.org/10.1097%2FCCM.0000000000002953. [ Links ]
21. Schuetz P, Briel M, Christ-Crain M, et al. Procalcitonin to guide initiation and duration of antibiotic treatment in acute respiratory infections: an individual patient data meta-analysis. Clin Infect Dis. 2012 Sep;55(5):651-62. https://doi.org/10.1093/cid/cis464. [ Links ]
22. Schroeder S, Hochreiter M, Koehler T, et al. Procalcitonin (PCT)-guided algorithm reduces length of antibiotic treatment in surgical intensive care patients with severe sepsis: results of a prospective randomised study. Langenbecks Arch Surg. 2009 Mar;394(2):221-6. https://doi.org/10.1007%2Fs00423-008-0432-1. [ Links ]
 Correspondence:
Correspondence:
Email: rispah.chomba@wits.ac.za














