Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.58 no.1 Cape Town Mar. 2020
http://dx.doi.org/10.17159/2078-5151/2020/v58n1a3102
TRAUMA
Efficacy and patterns of use of antimicrobial prophylaxis for gunshot wounds in a South African hospital setting: an observational study using propensity score-based analyses
MC VisbeekI, II; JJ TaljaardII; MGJ de BoerI; UJ CronjeIII; E SteynIV
IDepartment of Infectious Diseases, Leiden University Medical Center, The Netherlands
IIDivision of Infectious Diseases, Department of Medicine, Tygerberg Academic Hospital, Stellenbosch University, South Africa
IIIDepartment of General Surgery, Mitchell's Plain District Hospital, South Africa
IVDivision of Surgery, Department of Surgical Sciences, Stellenbosch University and Tygerberg Academic Hospital, South Africa
ABSTRACT
BACKGROUND: Limited evidence supports the efficacy of antimicrobial prophylaxis (AP) in prevention of gunshot wound-related (GSW-related) infection in resource restricted areas. At Tygerberg Hospital, South Africa, it is standard care for GSW patients to receive one dose of broad-spectrum AP. For various reasons, this protocol is not consistently followed. This study aimed to assess the efficacy of AP in the reduction of in-hospital GSW-related infection and to identify opportunities for practice improvement
METHODS: All patients admitted with GSW over a three-month period were eligible for inclusion. Patients who did and did not receive AP were identified retrospectively the morning of admission; thereafter, data was collected prospectively. Data regarding circumstances of the incident, injury characteristics, type of AP and surgery was obtained. The occurrence of in-hospital GSW-related infection was recorded over 30 days or until discharge. Propensity score matching (PSM) and inverse probability weighting (IPW) methods were utilised to assess the effect of AP on the prevention of GSW-related infection
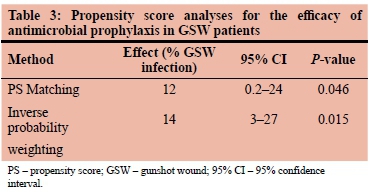
RESULTS: 165 consecutive patients were assessed, of which 103 received AP according to protocol within 12 hours of admission. PSM showed a reduced in-hospital GSW infection risk of 12% (95% CI, 0.2-24%, p = 0.046) with AP. IPW showed that AP reduced the risk for infection by 14% (95% CI, 3-27%, p = 0.015
CONCLUSIONS: Providing AP to GSW patients in a civilian setting appeared to result in a modest but clinically relevant lower risk of in-hospital GSW-related infection. In this study setting, optimisation of AP for all patients with GSWs should significantly lower the burden of wound infection
Keywords: Antimicrobial prophylaxis, gunshot wounds, infection
Introduction
The high rates of interpersonal violence involving firearms is a major problem in certain areas of South Africa.1 Firearm injuries contribute to the total burden of injury, both in terms of costs of care, as well as pressure on the already-limited resources in the public healthcare system. When gang violence leads to surges in admission rates of victims of gunshot wounds (GSWs), optimal care should be offered, as preventable complications may increase hospital stay. Wound infection is one of the many complications of GSWs.2 Contrary to popular belief, bullets are not sterile, despite high temperatures during firing.3 Such wounds often contain particles of clothing, environmental materials or skin contaminants, carried forward by the penetrating bullet, or sucked into the wound tract by the vacuum resulting from temporary cavitation. Traversing missiles fired by higher caliber weapons create a shock wave effect, leading to devitalisation of tissue and, particularly in the case of hollow viscus perforation, life-threatening infection may follow. In addition, for many reasons, delays to definitive treatment often occur in the pre-hospital or in-hospital setting. All these factors contribute to the high infective morbidity and mortality of gunshot injuries.
International guidelines recommend local debridement of the entrance and exit wounds and washout of the wound tract, as well as one dose of broad-spectrum antimicrobial prophylaxis (AP).4,5 At Tygerberg Hospital (TBH), the protocol for management of GSWs is to administer a single prophylactic intravenous dose of cefazolin or an oral dose of amoxicillin-clavulanic acid within 12 hours of admission. In daily clinical practice, the implementation of these wound care protocols is often compromised by late presentation, treatments at other clinics before referral and overcrowding of the treatment facility. Notably, violation of a protocol does not necessarily imply an error, as it may be a well-considered decision. Preliminary observations, however, indicated that in many cases the motivation for protocol violation was not immediately apparent.
This study aimed to audit the use of AP in GSW patients and to assess the efficacy of AP in reduction of in-hospital GSW-related infection, ultimately to identify opportunities for practice improvement. To address these aims, we investigated the following in GSW patients who presented to the TBH trauma unit: the use of AP, the prevalence of protocol violation, reasons for protocol violation and baseline factors associated with the later development of an in-hospital GSW infection. Addressing the aforementioned may contribute to a better understanding of how the incidence of in-hospital GSW infections could be reduced within this setting.
Methods
Design, setting and study population
All consecutive patients who presented with single or multiple GSWs to the trauma emergency room (ER) at TBH, Cape Town, South Africa, from 12 October 2017 to 3 January 2018, were eligible for inclusion. This series reports on civilian gunshot injuries, which are typically due to weapons with low to medium muzzle velocity. Patients who did and did not receive AP were retrospectively identified on the morning after admission; thereafter, data was collected prospectively. Demographic and injury-related data, as well as data associated with treatment and outcomes was collected for this observational study. Patients who died shortly after admission, before receiving treatment, were excluded. TBH serves a large metropolitan area and a rural referral region, consisting of a population of approximately 3 million. TBH is part of the South African public health care system, providing health care to those who are not privately insured. Many of the patients presenting at TBH with GSW injures are inhabitants of the townships surrounding the hospital, where poverty, drug abuse and gang violence is rife.
Standard procedures and definitions
The standard care at TBH for a newly admitted GSW patient consists of a primary survey by the ER-physician on duty to manage any immediate life-threatening conditions. To identify injuries and localise bullets and injury trajectories, a full body X-ray (LODOX) and standard radiological investigations, including CT scans, are performed according to clinical indications. If indicated, surgery is performed as soon as possible. As all GSW patients undergo radiological investigation as part of the standard work-up, the radiological reports of trauma emergency admissions were reviewed daily to ensure that no eligible patients were missed. According to ER protocol, GSW patients should receive a single intravenous dose of AP (either cefazolin or amoxicillin-clavulanic acid) within 12 hours of admission. Further care is provided by the relevant specialist surgical disciplines, who follow standard antibiotic prophylaxis and treatment protocols. AP received prior to admission to TBH was considered as adequate AP. If the attending physician diagnosed an infection, a form was added to the patient's medical chart on which details of the surgical and antimicrobial treatment were recorded.
Patient data
The following data was collected: demographic characteristics, the site and extent of the injury, the type and duration of antibiotic treatment, whether any surgical procedures were performed, and the occurrence of in-hospital infection(s). Patients were followed-up for 30 days or until discharge, to observe whether any GSW-related infection had developed. Surgery performed within 24 hours of admission was distinguished from surgery performed after 24 hours. Locations of the GSWs were categorised as follows: head and neck, thorax/abdomen/pelvis, limbs, and multiple locations (i.e., a combination of GSW locations).
Descriptive statistical analyses
Uni- and multivariate logistic regression analyses were performed to identify factors associated with AP status (i.e., 'yes, received' or 'no, did not receive'). Results of the univariate analyses were presented as risk ratios (RR) with 95% confidence intervals (95% CI). Chi-square tests were used to determine if there were any significant associations between categorical variables. The multivariate model that included the independent estimators of receiving AP was used to calculate the propensity scores (PSs, see below). Separate univariate analyses were performed to determine which clinical characteristics at presentation were associated with the later occurrence of in-hospital GSW-related infection.
Propensity score (PS) analyses
PS methods can be used to analyse observational data with regard to a treatment outcome, by defining which individuals and/or treatment groups have the same probability of receiving the intervention (e.g., AP). This probability is based on measured confounders and other baseline variables. By assessment of the outcome in relation to the intervention (i.e., yes or no) for patients with similar PSs (using randomness within observations), PS methods aim to attain the results reflective of those from a randomised study.6
In this study, the outcome of interest was 'in-hospital GSW infection before discharge or within 30 days of admission'. PSs were used to correct for selection bias, minimising the differences in the baseline characteristics between the patients who received AP correctly (i.e., according to the protocol) and those who did not. A multivariate logistic regression model was constructed to obtain the PS for each individual patient.6 Variables from both the univariate model for the risk of receiving AP and the model for the risk of developing an in-hospital GSW infection were included in the multivariate analysis (if the p-value in the univariate analysis was less than 0.10, and if the relation between the variable and the outcome was plausible). The balance of confounders within the quintiles of the PS was assessed.7 In addition, distribution of PSs in GSW patients who did and did not receive AP were plotted to verify if sufficient overlap was present.
The PSs were used to apply PS Matching (PSM), using the nearest neighbour method, and to derive inverse probability of treatment weights (IPTW), with the inverse of the PS for patients who received AP properly, and the inverse of 1 minus the PS for patients who did not receive AP.6 Both the PSM and the IPTW were used to calculate the Average Treatment Effect (ATE) of AP. Data analyses were performed using STATA software (StataCorp LP, 2015, IC Stata Statistical Software: Release 15, College Station, TX).
Results
Population
One hundred and seventy-two (172) consecutive patients were identified, of which 165 were included in the study (i.e., seven patients were excluded due to incomplete or missing information). As TBH is a tertiary hospital, 116 of the 165 patients (70.3%) were referred to TBH from smaller hospitals or field clinics. The 30-day in-hospital mortality rate for patients with GSWs in TBH over this period was 2.4% (4/165).
Univariate analyses
The mean age of the patients was 28.7 years (standard deviation: 10.2 years; range: 13-69 years), and the majority of patients were male (94.5%).
AP had been administered according to protocol in 103 patients (62.4%). Fifty-one patients (30.9%) developed an in-hospital GSW-related infection. The univariate analysis of baseline characteristics for receiving AP showed that the presence of a fracture, the presence of hollow viscus injury, being admitted on a Wednesday or a Thursday and receiving surgery within 24 hours were associated with a higher likelihood of receiving AP according to protocol (Table 1). The difference in adherence to protocol-based AP administration across days of the week is depicted in Figure 1.
Univariate analysis of baseline characteristics for acquiring an in-hospital GSW infection showed that the presence of a fracture, the presence of hollow viscus injury, receiving surgery within 24 hours, having more than one GSW and a hematocrit lower than 30% were associated with a higher risk of having an in-hospital GSW infection (Table 2).
PS analyses
The variables included in the multivariate model used to calculate the PSs were: receiving surgery within 24 hours of admission; presence of hollow viscus injury; presence of a fracture; the day of the week on which the patient was admitted. The 'multiple GSW' variable, despite being significant in the univariate analysis, was omitted from the PS analysis as it demonstrated no effect in the regression model. In addition, the variable 'hematocrit below 30%' was not included in the analysis as it was not recorded for a large portion of the sample. No major differences in the distribution of the confounders were observed between groups with and without AP, within the PS-based quintiles. The distribution of the PSs overlapped substantially for GSW patients who did and did not receive AP (graph not shown). According to the logit PSM and inverse probability weighting (IPW) analyses, the administration of AP according to protocol to GSW patients decreased the incidence of in-hospital GSW infections by 12% (95% CI 0.2-24) and 14% (95% CI 3-27), respectively (Table 3).
Discussion
This study evaluated the efficacy and the patterns of use of AP in GSW patients, using data collected at TBH between October 2017 and January 2018. Although the protocol used in TBH for early management of GSW patients dictates that every GSW patient should receive one dose of AP after admission, due to random and non-random events, patients did not always receive the prophylaxis. Of the GSW patients, 103 (62.4%) received AP according to protocol. Fifty-one (30.9%) GSW patients developed an in-hospital GSW-related infection. Results of PS and IPW analysis indicated that administration of AP results in an estimated average risk reduction of in-hospital GSW-related infection of 12% and 14%, respectively. Based on these findings, one could conclude that a single dose of AP is a modest but effective tool to reduce the incidence of in-hospital GSW-related infection in resource-limited settings.
A retrospective observational study conducted in Nigeria reported that GSWs in the lower extremities, hollow viscus injury, the presence of a fracture, and a delay > 6 hours between the incident and admission, were associated with the occurrence of GSW-related infection.2 Our findings confirm the observation that presence of hollow viscus injury, or a fracture, are associated with acquiring a GSW-related infection. A study by Nguyen et al., conducted in the United States of America, investigated the infection rates and treatment of GSWs of the extremities.8 This non-randomised clinical study reported that a single dose of AP was associated with a lower rate of infection, compared to no AP, in GSWs with only soft tissue injury. In addition, the study found that administering multiple doses versus a single dose did not result in a further reduction of the rate of GSW infection.
In our study, patients with one or more fractures, with hollow viscus injury, who were admitted on a Wednesday or a Thursday, and who went to theatre within 24 hours, had a higher likelihood of receiving the dose of AP according to protocol. The fact that patients admitted on a Wednesday or a Thursday had a higher likelihood of receiving AP could be explained by the reduced trauma caseload on these mid-week days compared to weekends, when the massive patient load may have contributed to less optimal compliance with standard protocols. Patients with rib fractures usually received chest drains for which AP was routinely administered, and patients with hollow viscus injury received AP at induction of anesthesia for emergency laparotomy. Patients with multiple GSWs and patients with a gunshot-related fracture appeared to have a higher risk of acquiring an in-hospital GSW infection, with a relative risk of 2.08 and 1.81, respectively. Yet, only 63.9% of the multiple GSWs patients and 69.1% of the patients with a gunshot-related fracture received antimicrobial therapy according to the protocol. For this already-overburdened health-care setting, stricter adherence to the protocol may contribute to decreasing the GSW infection rates, especially for these higher risk subgroups.
Strengths and limitations
A limitation of this study is that only GSW-related infection that occurred during admission could be assessed. Patients who left the hospital or were infection free during the maximal follow-up period of 30 days were considered not to have acquired a GSW-related infection. It was not possible to trace all patients after they had left TBH. Hence, only GSW infections occurring during the admission period were evaluated. A second limitation of this study is that, due to limited available data, we did not assess the blood transfusion requirements of patients. It is well known that patients receiving massive transfusion would be more susceptible to infective complications. How this links up with the timing of the initial AP would require further investigation. PS analysis is widely accepted as appropriate for the analysis of observational studies6 and this method assumes that all confounders are known and have been measured. This study was designed with the aim of recognising and recording all potential confounders, however, this cannot be guaranteed. The strength of this study lies in the complete and detailed clinical data, prospectively collected in a large series of civilian low- to medium-energy transfer handgun injuries. A level of randomness in the allocation of AP was demonstrated, which allowed for the application of PS analyses. Given that timely and adequate surgical management plays an important role in the prevention of GSW-related infection, the impact of AP may vary according to circumstances. Paradoxically, the patients who underwent surgery within the first 24 hours had higher infection rates, as this group included those with risk to life or limb. Shock, hypoxia, acidosis, and tissue ischemia are physiological indicators that mandate urgent intervention for emergency surgery.
Relevance
The increasing prevalence of antimicrobial resistance is a global health crisis.9,10 One of the factors associated with the development of antimicrobial resistance is inappropriate prescription and administration of antibiotics. From a global health perspective, antimicrobial therapy could be considered in terms of access versus excess. In low-income countries, the accessibility to appropriate antimicrobials is often the limiting factor in providing the best care for patients with an infection or at high risk of acquiring one. Middle- and high-income countries suffer more often from an excessive use of antimicrobials which predisposes to future antimicrobial resistance.11,12 Achieving a balance between access and excess in AP is essential for the prudent management of infectious diseases and their prophylaxis. The results of this study show that in this particular South African setting, the access to optimal antimicrobial therapy remains challenging, despite TBH being a tertiary referral hospital. Awareness of the strengths and weaknesses of a system, as well as the optimisation of antimicrobial therapy governance, should reduce infections and eventually lower mortality rates and healthcare costs.
Conclusions
Providing AP to GSW patients results in a modest but clinically relevant reduction of the risk of in-hospital GSW-related infection. In resource-limited settings, the provision of appropriate AP for patients with multiple GSWs or GSW-related fractures is feasible, although it can be challenging at times. More research should be conducted to strengthen the evidence of the efficacy of AP for the prevention of GSW-related infection, preferably a randomised clinical trial (RCT). As RCTs are almost impossible to perform in the acutely injured, an observational study with more patients from multiple centers could enhance our knowledge of the efficacy of AP. Future studies should focus on the optimal timing of prophylaxis as well as the duration of prophylactic antibiotic administration, especially for complex injuries involving combinations of bone, soft tissue, and hollow viscera.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of TBH and the Human Research Ethics Committee of the University of Stellenbosch.
Acknowledgement
The authors thank Prof. S le Cessie, Department of Clinical Epidemiology and Biostatistics, Leiden University, for advice on conducting the propensity score analyses.
Conflict of interest
The authors declare that there is no conflict of interest. This manuscript represents original research. It has not been published previously, nor is it under review elsewhere. The information contained within this manuscript has not been published in abstract form or in Congress proceedings. None of the authors has a conflict of interest. All journal requirements for submission, including ethics approval, have been fulfilled.
ORCID
MC Visbeek https://orcid.org/0000-0002-6025-2053
JJ Taljaard https://orcid.org/0000-0002-5210-9054
MGJ de Boer https://orcid.org/0000-0002-5009-6499
UJ Cronje https://orcid.org/0000-0002-9587-4127
E Steyn https://orcid.org/0000-0002-8090-1559
REFERENCES
1. Matzopoulos R, Simonetti J, Prinsloo M, et al. A retrospective time trend study of firearm and non-firearm homicide in Cape Town from 1994 to 2013. S Afr Med J. 2018;108(3):197-204. Available from: http://dx.doi.org/10.7196/SAMJ.2018.v108i3.12756. PMID: 30004363. [ Links ]
2. Omoke NI. Analysis of risk factors for gunshot wound infection in a Nigerian civilian trauma setting. World J Surg. 2016;40(8):1885-91. Available from: http://dx.doi.org/10.1007/s00268-016-3475-4. PMID: 26932876. [ Links ]
3. Wolf AW, Benson DR, Shoji H, Hoeprich P, Gilmore A. Autosterilization in low-velocity bullets. J Trauma. 1978;18(1):63. PMID: 621766. [ Links ]
4. Hospenthal DR, Murray CK, Andersen RC, et al. Guidelines for the prevention of infections associated with combat-related injuries: 2011 update: endorsed by the Infectious Diseases Society of America and the Surgical Infection Society. J Trauma. 2011;71(2 Suppl 2):S210-34. Available from: http://dx.doi.org/10.1097/TA.0b013e318227ac4b. PMID: 21814089. [ Links ]
5. Dellinger EP, Gross PA, Barrett TL, et al. Quality standard for antimicrobial prophylaxis in surgical procedures. Clin Infect Dis. 1994;18(3):422-7. Available from: http://dx.doi.org/10.1093/clinids/18.3.422. PMID: 8011827. [ Links ]
6. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399-424. Available from: http://dx.doi.org/10.1080/00273171.2011.568786. PMID: 21818162. [ Links ]
7. Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014;49(5):1701-20. Available from: http://dx.doi.org/10.1111/1475-6773.12182. PMID: 24779867. [ Links ]
8. Nguyen MP, Savakus JC, O'Donnell JA, et al. Infection rates and treatment of low-velocity extremity gunshot injuries. J Orthop Trauma. 2017;31(6):326-9. Available from: http://dx.doi.org/10.1097/BOT.0000000000000827. PMID: 28240620. [ Links ]
9. Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health. 2015;109(7):309-18. Available from: http://dx.doi.org/10.1179/2047773215Y.0000000030. PMID: 26343252. [ Links ]
10. World Health Organization. Worldwide country situation analysis: response to antimicrobial resistance. Geneva: World Health Organization, 2015. [ Links ]
11. Mendelson M, Rottingen J-A, Gopinathan U, et al. Maximising access to achieve appropriate human antimicrobial use in low-income and middle-income countries. Lancet. 2016;387(10014):188-98. Available from: http://dx.doi.org/10.1016/S0140-6736(15)00547-4. PMID: 26603919. [ Links ]
12. Tacconelli E. Antimicrobial use: risk driver of multidrug resistant microorganisms in healthcare settings. Curr Opin Infect Dis. 2009;22(4):352-8. Available from: http://dx.doi.org/10.1097/QCO.0b013e32832d52e0. PMID: 19461514. [ Links ]
 Correspondence:
Correspondence:
E Steyn
Email: esteyn@sun.ac.za














