Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.57 no.4 Cape Town Dez. 2019
http://dx.doi.org/10.17159/2078-5151/2019/v57n4a2764
TRAUMA
Renal trauma in a Trauma Intensive Care Unit population
V PillayI; M PillayII; TC HardcastleIII
IDepartment of General Surgery, University of KwaZulu-Natal, South Africa
IIDepartment of Virology, Inkosi Albert Luthuli Central Hospital, South Africa
IIIDepartment of Surgery, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: For the majority of renal injuries, non-operative management is the standard of care with nephrectomy reserved for those with severe trauma. This study in a dedicated Trauma Intensive Care Unit (TICU) population aimed to assess the outcomes of renal injuries and identify factors that predict the need for nephrectomy
METHODS: Patients, older than 18 years, admitted to TICU from January 2007 to December 2014 who sustained renal injuries had data extracted from the prospectively collected Class Approved Trauma Registry (BCA207-09). Patients who underwent surgical intervention for the renal injury or received non-operative management were compared. The key variables analysed were: patient demographics, mechanism of injury, grade of renal injury, presenting haemoglobin, initial systolic blood pressure, Injury Severity Score and Renal Injury AAST Grade on CT scan in patients who did not necessarily require immediate surgery, or at surgery in those patients who needed emergency laparotomy
RESULTS: There were 74 confirmed renal injuries. There were 42 low grade injuries (grade I-III) and 32 high grade injuries (5 grade IV and 27 grade V). Twenty-six (35%) had a nephrectomy: 24 with grade V injuries and 2 with grade IV injuries required nephrectomy. Six patients in the high injury grade arm had non-operative management. A low haemoglobin, low systolic blood pressure, higher injury severity score, and a high-grade renal injury, as well as increasing age were positive predictors for nephrectomy in trauma patients with renal injury
CONCLUSION: Non-operative management is a viable option with favourable survival rates in lower grade injury; however, complications should be anticipated and managed accordingly. High grade injuries predict the need for surgery
Keywords: intensive care, trauma, renal injury, nephrectomy, non-operative management
Introduction
The management of blunt and penetrating renal injuries has evolved from mandatory surgical exploration to non-operative care over the last few decades. This paradigm shift stems from improved trauma care, better imaging and angioembolisation, particularly in isolated kidney injuries. In unstable polytrauma patients with renal injuries, nephrectomies are performed as time consuming renal salvage procedures are contraindicated in the damage-control setting. Conservative management of renal injuries is not entirely innocuous, and complications that include urinoma, perinephric abscess formation, delayed bleeding and renovascular hypertension need to be actively sought and managed for successful outcomes.1 In critically ill trauma patients unnecessary nephrectomy when successful non-operative management is possible equates to an iatrogenic injury, whilst delaying a warranted nephrectomy may lead to profound morbidity or mortality. Critical analysis of patient factors can help identify the kidney at risk for nephrectomy or the renal injury which may be successfully managed non-operatively. The aim of this study was to assess the outcome of nephrectomies or non-operative management of renal injuries in the polytrauma population in a dedicated trauma intensive care unit. The secondary aim is to determine predictive factors for nephrectomy in both the total and the severe injury groups.
Methods
This study was a retrospective chart review of prospectively captured patients in the Trauma Registry of the Inkosi Albert Luthuli Central Hospital Trauma Service (IALCH). All patients admitted to Trauma Intensive Care Unit (TICU) from January 2007 to December 2014 who sustained renal injuries were audited from the prospectively collected Class Approved Trauma Registry (BCA207-09).
All adults older than 18 years of age were included in this study. Patients were either those who underwent surgical intervention for renal injury, or those who received non-operative management. Patients who had index laparotomies performed at TICU were referred either directly from the scene of the injury, or from institutions where surgical services were not available, e.g. district hospitals. This study also includes patients who had surgery at regional hospitals and required ICU care in the postoperative setting. Data accrued included: patient demographics, mechanism of injury, grade of renal injury, presenting haemoglobin, initial systolic blood pressure, Injury Severity Score (ISS).
All patients who had primary surgery at IALCH had initial haemoglobin and systolic blood pressure readings recorded. Not all patients referred post-surgery to TICU had initial haemoglobin and systolic blood pressures documented on the accompanying referral letters. Renal-specific complications in patients with non-operative management were also noted. Renal injuries were graded according to the AAST grading of renal injuries, either on CT scan in patients who did not require immediate surgery, or as assessed at emergency laparotomy.2 ISS was calculated by abstraction from the patient record using the standardised formula.
Emergency surgery was performed in the face of haemodynamic instability or peritonitis. Non-operative management entailed strict bed rest, intravenous fluids, serial abdominal examinations, serial haemoglobin assessment, urinary catheterisation with intake and output monitoring, along with analgesia. Repeat CT scans were not routinely performed.
Those with high-grade renal injuries were categorised into 2 groups: those who had nephrectomy for their injuries, versus those who had successful conservative management. The two groups were compared for patient characteristics, injury type, trauma and severity as indicated by the ISS. Chi-square p-values were determined using Stata (Statacorp, USA).
Results
From 2007 to 2014 there were 73 patients with 74 confirmed renal injuries. Table 1 details the severity of renal injury related to the mechanism of injury. One patient had bilateral kidney injuries: grade I and grade IV. There were 42 low grade injuries comprising: 17 grade I injuries, 11 grade II injuries and 14 grade III injuries. High grade injuries totalled 32, with 5 grade IV injuries and 27 grade V injuries.
Blunt trauma accounted for 47 renal injuries and penetrating trauma accounted for 27 renal injuries. None of the 41 patients with grades I; II or III injuries (low grade injuries) underwent nephrectomy. Twenty-six of the 32 patients with high-grade injuries (81.3%): (2 grade IV and 24 grade V) had nephrectomies performed, while 6/32 (18.8%) high grade injury patients (3 grade V and 3 grade IV patients) had successful non-operative management.
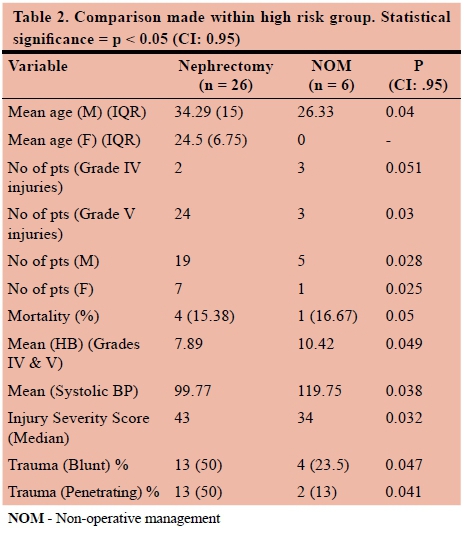
Table 2 compares the high-risk groups. The high-risk groups comprised 24 male and 8 female patients. The mean age for male patients was a decade older than the females. Twenty males and 7 females sustained grade V injuries. Four males and 1 female sustained grade IV injuries. Nineteen males (18 grade V and 1 grade IV) and 7 females (6 grade V and 1 grade IV) underwent nephrectomy. Five males (2 grade V and 3 grade IV) and 1 female patient (grade V) were treated conservatively.
Nine out of 32 patients in the high-grade injury arm had CT scans performed. Six patients had grade V injuries of which: 4 patients had nephrectomies performed; three patients had grade IV injuries, all of which were treated conservatively. No patient had renorrhaphy attempted.
In patients who underwent conservative management, one developed a renal artery pseudo-aneurysm with persistent macroscopic hematuria and was subsequently successfully embolised electively, with complete resolution of the hematuria. One patient developed renal failure requiring ongoing renal replacement therapy, another patient with a renal vein thrombosis was successfully managed expectantly. One patient developed hypertension and another had persistent microscopic hematuria. Only one patient died. This patient had multi-organ failure and was treated conservatively in view of the poor prognosis.
Subgroup analysis
A significant difference was observed in the mean age between males and females requiring a nephrectomy. The mean age of males requiring a nephrectomy (34.29) was found to be significantly higher when compared to those who did not undergo a nephrectomy (26.33, p < 0.05). Twenty-four of the 26 patients who underwent a nephrectomy presented with grade V injuries during examination. Grade V injuries strongly increased the likelihood of a patient requiring a nephrectomy (p-0.03). Of those patients with grade IV injuries (n = 5), only 2 underwent a nephrectomy (p-0.051) therefore, no significant association between grade IV injuries (n = 5) and nephrectomy is observed.
Patients who underwent a nephrectomy did not show any significant difference in mortality when compared to those who did not require a nephrectomy. Furthermore, patients with a lower mean HB of 7.89+/-2.54 [SD = 5.35-10.43] were more likely to require a nephrectomy than patients with a mean HB of 10.42 +/-3.08 [SD = 7.34-13.5] (p < 0.05). In addition to the above, patients with a much higher ISS were more likely to undergo a nephrectomy (p-0.032). Four out of 6 patients who underwent successful non-operative management had blunt abdominal trauma, while only 2 patients with penetrating trauma were able to complete successful conservative management for their high grade injuries.
Discussion
The kidney is implicated in approximately 1-5% of all trauma cases.3 More than half of all genitourinary trauma cases involve the kidney. Conservative management is often unsuccessful in treating persistent bleeding and high-risk vascular injuries secondary to penetrating renal trauma.4
The overall nephrectomy rate in Europe is 13%;3 while Metro and McAninch5 describe a nephrectomy rate of 11% from a study based in the USA, after reviewing 3 150 renal injuries over 25 years. Locally, Moolman et al.6 recorded a nephrectomy rate of 24%. Our study demonstrated an overall nephrectomy rate of 35%. Upon further scrutiny we found that 89% of grade V and 40% of grade IV injuries required nephrectomies. All patients who had an exploratory laparotomy had a nephrectomy. Since the nephrectomy group is confined to high grade injuries, a nephrectomy rate of 35% is not surprising in this group. It may well be low for the grade of injury being treated.
Only 28% of all patients in the high-grade injury arm had CT scans performed. The paucity of imaging stems from patients requiring emergent laparotomy on presentation based on either hemodynamic instability or evidence of peritonism. Unequivocal indications for emergency laparotomy outweigh imaging and this is a case in point in this study. None of the patients in this study had isolated renal injuries, hence the indication for laparotomy was not solely based on renal injury, but rather other solid or hollow visceral compromise.
Often nephrectomies are performed purely because patients are too unstable to tolerate renorrhaphy. This phenomenon was noted in our study. These sentiments are also echoed by Myers and McAninch7 who found that up to 22% of cases potentially salvageable kidneys underwent nephrectomy as a life-saving technique in the face of patient instability and the need for damage control surgery. The 3 patients noted to have grade IV injuries on CT scan were all successfully treated non-operatively, while 2 out of 6 patients with grade V injuries did not undergo nephrectomy. In our study more than 50% of patients with grade IV injuries stable enough to undergo CT imaging underwent successful conservative management.
Pioneering work by Angorn et al. defined the segmental arterial blood supply of the kidney and confirmed selective angioembolisation (SAE).8 SAE is a reasonable alternative to laparotomy provided there is no other indication for immediate open surgery. Angioembolisation has been documented to reduce the failure of conservative management for renal injuries and improve patient outcomes.9 This is particularly evident in specialised centres with expertise and experience with angioembolisation where it is hailed as a viable option to achieve haemorrhage control.10 Emergency SAE is not available in our setting and, considering the injury severity and polytrauma nature of our patients on admission, it is doubtful whether this modality would have had an appreciable effect on our nephrectomy rate. We postulate that SAE is best utilised in patients with preferably isolated renal injuries, or patients not requiring abbreviated/emergency laparotomy for concomitant injuries. A 2016 study by Lachon and colleagues11 advocated the use of angioembolisation in hemodynamically stable and unstable patients. Their study documented salvage rates of 88% for grade IV and up to 50% of grade V injuries.
Polytrauma patients invariably have a higher ISS. In this study the patients who had nephrectomy had higher ISS when compared to those patients who had non-operative management. A Chinese study also noted that a higher ISS was a positive predictor for nephrectomy.12 Although the incidence of blunt and penetrating trauma cases is the same in our study, it is noted that patients with blunt trauma are more amenable to non-operative management when compared to their counterparts who sustained penetrating trauma.
No patient in the low-grade injury arm underwent nephrectomy, however 26 patients in the high-grade arm had nephrectomy performed. Wright, Nathens, et al.13 rate the grade of the renal injury as the greatest predictor for nephrectomy. This sentiment holds true in the current study. An overwhelming 24 out of 27 patients with grade V injuries underwent nephrectomy. Whilst only 2 out of 6 patients with grade IV injuries underwent nephrectomy.
Interrogation of the haemoglobin levels between the operative and non-operative arms in our study revealed a statistically and clinically significant difference between the 2 groups. Higher haemoglobin levels favoured non-operative management. Those patients who underwent nephrectomy had on average 2.53 g/dl lower haemoglobin levels compared to their counterparts, that equates to approximately 2 units of blood. Prasad and Devraj, in a report from India, noted that the need for higher red blood cell concentrate transfusion pointed to a positive prediction for nephrectomy.14
The nephrectomy limb had significantly lower systolic blood pressures compared to the non-operative arm. An Australian study by Mcguire and colleagues15 cites hypotension and increasing age as predictors for nephrectomy. In our study, male patients undergoing nephrectomy were on average 8 years older than their counterparts in the conservatively treated arm. We found that younger patients fared much better, and older patients were noted to have a greater propensity for nephrectomy. It was also noted that 7/26 patients (26.92%) who had nephrectomies were female. This is comparable to the male to female ratio of 3:1 for kidney injuries as reported by the European Association of Urology.
Conservative management, although desirable, can lend itself to complications. Patients in the non-operative arm of our study were found to have sequelae from conservative management.
Pseudo-aneurysms are seen in 6% of patients treated conservatively.1 The treatment of choice is selective angioembolisation and the one patient in this study with a renal artery pseudo-aneurysm fared well post-intervention with resolution of the hematuria.
One out of 6 patients demised in the conservatively treated arm. This patient had extensive injuries and did not die purely because of any nephrectomy being performed, but rather because the injuries sustained were not compatible with life and nephrectomy would have been an exercise in futility. Delayed rebleeding, a noted complication that one can encounter in patients managed conservatively, was not evident in this study. Other complications, including urinoma formation and hypertension, did not occur in this cohort.
Five out of 6 patients (83.33%) with high grade injury treated with non-operative management survived, while in the nephrectomy arm 84.62% of patients survived. In the appropriately selected patient conservative management is equal and comparable to operative intervention. Despite the aggressiveness of surgical intervention being performed in our study, we note no survival disadvantage in patients undergoing nephrectomy.
Limitations
This study was a retrospective chart review of a prospective registry, based at a single centre, specifically dealing with severe trauma leading to an inherently biased sample. A few patients referred to this institution from the base hospitals had referral details that precluded complete data acquisition. Finally, no long-term follow-up was available for any of the patients discharged back to the referring base hospitals.
Conclusion
This study has highlighted that a low haemoglobin, low systolic blood pressure, higher ISS, and a high-grade renal injury, along with an increasing age range, were all positive predictors for nephrectomy in polytrauma patients with any renal injury. These findings concur with international and local evidence. We found that in the polytrauma population in our setting a decision to perform an exploratory laparotomy invariably equated to a nephrectomy being performed. Although renal conservation is highly revered and should be attempted if possible, we found no mortality difference between the nephrectomy and conservatively managed arms of our study.
Non-operative management is a viable option with favourable survival rates in the appropriately selected patient, including some in the high-grade sub-group. The ideal patient for non-operative management of a renal injury is a younger patient, haemodynamically stable, with a higher haemoglobin level and a lower injury severity score not requiring other open surgical intervention.
Conflict of interest
None
Funding
None
Orcid
Τ Hardcastle © http://orcid.org/0000-0002-3967-0234
REFERENCES
1. Broghammer JA, Fisher MB, Santucci RA. Conservative management of renal trauma: a review. Urology. 2007;70:623-9. [ Links ]
2. Moore EE, Shackford SR, Pachter HL, et al. Organ injury scaling: spleen, liver and kidney. J Trauma. 1989 Dec;29(12):1664-6. [ Links ]
3. Summerton DJ, Djakovic N, Kitrey ND, et al. Guidelines on urological trauma; European Association of Urology; 2014. [ Links ]
4. Heyns CF. Renal trauma: indications for imaging and surgical exploration. BJU International. 2004;93:1165-70. [ Links ]
5. Metro MJ, McAninch JW. Surgical exploration of the injured kidney: current indications and techniques; Official Journal of the Brazilian Society of Urology. 2003;29(2):98-105. [ Links ]
6. Moolman C, Navsaria PH, Lazarus J, et al. Nonoperative Management of Penetrating Kidney Injuries: A Prospective Audit. Urology. 2012 Jul;188:169-73. [ Links ]
7. Myers JB, McAninch WA. Nephrectomy for trauma: when is it necessary? Urology. 2009 Apr;181(4):supp. [ Links ]
8. Angorn IB. Segmental dearterialization in penetrating renal trauma. Br J Surg. 1977;64(1):59-65. [ Links ]
9. Muir MT, Inaba K, Ong A, et al. The need for early angiography in patients with penetrating renal injuries. Eur J Trauma Emerg Surg. 2012;38:275-28. [ Links ]
10. Bittenbender EN, Reed AB. Advances in renal intervention for trauma. Sem Vasc Surg. 2013;26:165-9. [ Links ]
11. Lachon C, Fiard G, Arnoux V. High grade blunt renal trauma: predictors of surgery and long-term outcomes of conservative management. A prospective single centre study. Urology. 2015 Jan;195;106-11. [ Links ]
12. Chia-Shen Y, Chun-Jen Chen I , Chien-Ying W, et al. Predictive indications of operation and mortality following renal trauma. J Chin Med Assoc. 2012;75:21e24. [ Links ]
13. Wright JL, Nathens AB, Rivara FP. Renal and Extrarenal Predictors of Nephrectomy from the National Trauma Data Bank; Urology. 2006 Mar;175:970-5. [ Links ]
14. Prasad NH, Devraj R, Ram Chandriah G, et al. Predictors of nephrectomy in high grade blunt renal trauma patients treated primarily with conservative intent. Indian J Urol. 2014 Apr-Jun;30(2):158-60. [ Links ]
15. McGuire J, Bultitude MF, Davis P, et al. Predictors of outcome for blunt high grade renal injury treated with conservative intent. Urology; 2011 Jan;185:187-91 [ Links ]
 Correspondence:
Correspondence:
Vasanthan Pillay
pillayvas@yahoo.com














