Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.57 no.4 Cape Town Dez. 2019
http://dx.doi.org/10.17159/2078-5151/2019/v57n4a2856
GENERAL SURGERY
Compliance with the Surviving Sepsis Campaign guidelines for early resuscitation does not translate into improved outcomes in patients with surgical sepsis in South Africa
S GreenI; MTD SmithII; VY KongII, IV; DL SkinnerI; JL BruceII; GL LaingII; P BrysiewiczIII; DL ClarkeII, IV
IDepartment of Anaesthesia, Critical Care and Pain Management, University of KwaZulu-Natal, Durban, South Africa
IIDepartment of Surgery, University of KwaZulu-Natal, Durban, South Africa
IIISchool of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa
IVDepartment of Surgery, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
INTRODUCTION: This project set out to audit our compliance with the 3-hour bundles of care for surgical sepsis and to interrogate how compliance or non-compliance impacts on the outcome of surgical sepsis in our institution.
METHODS: All emergency surgical patients over the age of fifteen years were reviewed. All patients who fulfilled the ACCP/ SCCM criteria for sepsis or septic shock, with a documented surgical source of infection, were identified for review.
RESULTS: A total of 677 septic patients with a documented surgical source of sepsis were included. Of the 677 patients, 53% (360/677) had intra-abdominal sepsis, 17% (116/677) had diabetic-related limb sepsis and the remaining 30% (201) had soft tissue infections. A total of 585 operative procedures were performed. Compliance with all components of the 3-hour bundle metrics was achieved in 379/677 patients (56%), and not achieved in 298/677 patients (44%). The only significant difference between the compliant and the non-compliant groups was respiratory rate greater than 22 breaths/minute (131 vs 71, p = 0.002) in the compliant cohort. Amongst the compliant cohort 77/379 patients (20%) required admission to ICU, whilst 41/298 patients (14%) in the non-compliant cohort required admission to ICU. This difference was statistically different (p = 0.026). There was no difference in the median length of hospital stay (6 days) between the two groups. Fifty-five patients in the compliant cohort died (15%), whilst 31 (10%) of the patients in the non-compliant cohort died. This difference was not statistically different (p = 0.111).
CONCLUSION: Compliance with the SCC 3-hour bundle did not seem to improve mortality outcomes in our setting. This observation cannot be adequately explained with our current data and further work looking at management of surgical sepsis in our setting is required. Time to surgical source control is probably the single most important determinant of outcome in patients with surgical sepsis and other aspects of the care bundle are of secondary importance.
Keywords: surgical sepsis, compliance, surviving sepsis, source control.
Introduction
Sepsis is a heterogeneous syndrome which develops as a result of an unregulated immune response secondary to infection, and which can lead to organ dysfunction and death.1 The worldwide incidence of sepsis appears to be increasing and it has been estimated that the annual global incidence is 31.5 million cases of which 19.4 million are severe.2 This translates into approximately 5.3 million sepsis related deaths each year.2-3 There is, however, very little information on the epidemiology and outcome of sepsis in low and middle income countries.2-8 This is a major deficit, as it is estimated that 90% of the worldwide deaths due to pneumonia, meningitis or other infectious causes occur in these countries.3 Over the last decade guidelines for the management of sepsis and septic shock have been regularly released and updated as the Surviving Sepsis Campaign (SSC) guidelines. These guidelines propose "bundles of care".9 Although data exists to suggest that implementing these "bundles of care" results in improved mortality rates,10-13 the uptake of these bundles in low- and middle-income countries (LMICs) has been heterogeneous.5-8 This project was undertaken in a busy public hospital in South Africa, which is a MIC. It set out to audit our compliance with the 3-hour bundles of care for surgical sepsis and to interrogate how compliance or non-compliance impacted on the outcome of sepsis in our institution, with regards to mortality, ICU admission and length of hospital stay.
Materials and methods
Clinical setting
This was a retrospective review of a prospectively entered database undertaken at the Pietermaritzburg Metropolitan Trauma Service (PMTS) in Pietermaritzburg, KwaZulu-Natal Province (KZN), South Africa. KZN is located on the east coast of South Africa and has a population of over 11 million people. Fifty per cent of the population resides in rural areas. Grey's Hospital provides tertiary care to the city of Pietermaritzburg and also serves as the referral center for nineteen other rural hospitals within the western third of the province. This is a total catchment population of over three million people. Our prospectively entered electronic registry was reviewed for the five-year period from January 2010 to December 2014. Ethics approval for the maintenance of this registry was provided by the Biomedical Research Ethics Committee (BREC) of the University of KwaZulu-Natal (reference: BCA 221/13).
Patient enrolment criteria and definitions
All emergency surgical patients over the age of fifteen years who were admitted to Grey's Hospital were reviewed. Patients with a documented surgical source of infection and with at least two of the following 2012 ACCP/SCCM criteria for sepsis or septic shock,9 were identified: fever (> 38.3oC) or hypothermia (core temperature < 36oC), heart rate > 90 bpm or more than two standard deviations (SD) above the normal value for age, tachypnoea, altered mental status.
Patients without a confirmed surgical source of sepsis were excluded. Data reviewed from the registry included basic demographic information, admission physiological parameters, biochemistry and haematology results, diagnosis, fluids administered, antibiotics received, surgery performed, requirement for intensive care (ICU) admission, length of hospital stay and mortality. Morbidities were classified by organ systems (e.g. hospital acquired pneumonia was classified as "respiratory system").
The surgical pathologies were classified into the following categories: intra-abdominal sepsis, diabetic related limb sepsis, soft tissue sepsis.
We reviewed compliance with the SSC bundles within the first three hours of presentation.
The 3-hour bundle includes the following interventions: Measurement of a serum lactate level, obtaining blood cultures before the administration of antibiotics, the administration of broad-spectrum intravenous antibiotics, the administration of 30 ml/kg of intravenous crystalloid if hypotension is present. Hypotension is defined as a systolic BP (SBP) less than 90 mmHg.
For the purposes of this study, compliance was defined as completing the following components within three hours: measurement of serum lactate, administration of broad spectrum antibiotics within three hours and administration of 30 ml/kg of intravenous colloid if patients had hypotension (SBP < 90 mmHg). Not all surgical patients get blood cultures done in the emergency department, so this component of the 3-hour bundle could not be measured. Non-compliance was defined as failure to complete any or all of these components within three hours. Time of presentation/time zero was defined as the time of arrival in the emergency department.
Statistical methods
Data were processed and analysed using Stata 13.0 (StataCorp, 2013). Continuous variables were summarised using mean and standard deviation [SD]. If there was evidence of skewing/asymmetrical outliers, the median and interquartile range [IQR] were presented instead.
Results
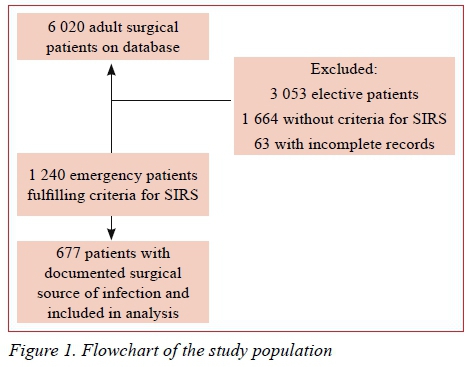
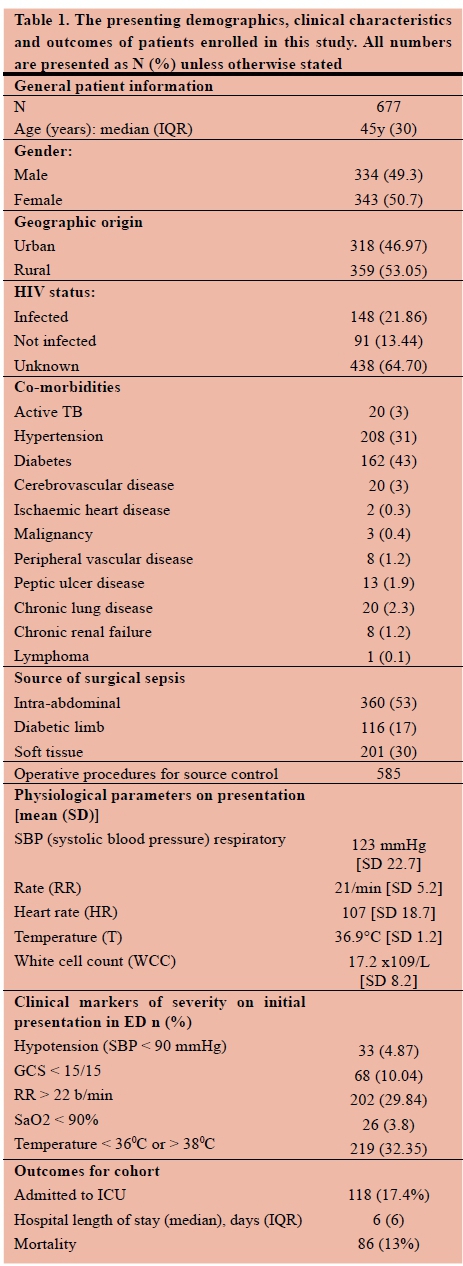
Figure 1 shows the patient selection. Out of a total of 6 020 adult surgical patients on the registry, 3 053 were elective patients, 1 664 patients did not fulfil the ACCP/SCCM criteria for sepsis or septic shock and 63 had incomplete records. The remaining 1 240 emergency surgical patients fulfilled the criteria for ACCP/SCCM criteria for sepsis or septic shock. Of these, 677 had a documented surgical source of sepsis and were included. Table 1 summarises the study population. Of the 677 patients, 49% (334/677) were male and the median age was 45 years [IQR 30y].
Clinical presentation
Physiological parameters (mean value) on presentation were as follows: systolic blood pressure (SBP): 123 mmHg [SD 23], respiratory rate (RR): 21/min [SD 5.2], heart rate (HR): 107 [SD 19], temperature (T): 37°C [SD 2], white cell count (WCC): 20 x109/L [SD 8]. Twenty-two percent (148/677) of all patients were known to be HIV positive, 13% (91/677) were negative and the remaining 65% (438) were of unknown HIV-infection status. The markers of disease severity on initial presentation to ED that were used included: hypotension (SBP < 90 mmHg), Glasgow Coma Score (GCS) < 15, a RR > 22 breaths/minute, SpO2 < 90%, and T either < 36oC or > 38oC. A total of 33 patients (4,9%) were hypotensive (SBP < 90mmHg), 68 patients (10,0%) had a GCS < 15, 202 (29.8%) patients had a RR > 22 breaths/minute, 33 patients (4.9%) presented with SpO2 < 90% in room air, and 219 (32.4%) patients had a temperature < 36oC or > 38oC. These data are tabulated in Table 1.
Spectrum of surgical disease
Of the 677 patients, 53% (360/677) had intra-abdominal sepsis, 17% (116/677) had diabetic-related limb sepsis and the remaining 30% (201) had soft tissue infections. A total of 585 operative procedures were performed. These data are included in Table 1.
Outcome
A total of 118 patients (17%) required admission to ICU. The median hospital stay was 6 days (IQR 6), and 86 patients died, giving an overall mortality rate of 13%.
A total of 207 patients (31%) developed complications. The mortality for intra-abdominal sepsis was (13%), for diabetic foot sepsis (14%) and for necrotising fasciitis (27%).
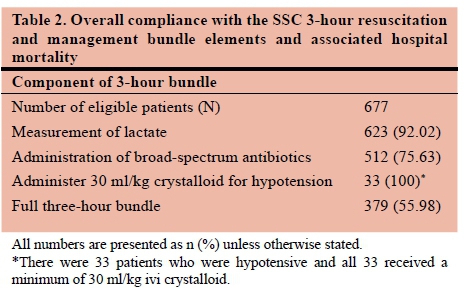
Compliance with the SSC 3-hour bundle metrics
Table 2 shows the overall compliance with the 3-hour SSC bundle and the associated mortality. Compliance with all components of the 3-hour bundle metrics was achieved in 379/677 patients (56%), and not achieved in 298/677 patients (44%). Table 3 and Table 4 show the differences between the compliant and the non-compliant groups. The only significant difference, between the compliant and the non-compliant groups was respiratory rate, which was greater than 22 breaths/minute (131 vs 71, p = 0.002) in the compliant cohort. Amongst the compliant cohort 77/379 patients (20%) were admitted to ICU, whilst 41/298 patients (13.7%) in the non-compliant cohort were admitted to ICU. This difference was statistically different (p = 0.026). There was no difference in the median length of hospital stay between the two groups. Fifty-five patients in the compliant cohort died (15%), whilst 31 (10%) of the patients in the non-compliant cohort died. This difference was not statistically different (p = 0.111).
Discussion
In 2004, the SSC published guidelines for the management of sepsis and septic shock. These included graded recommendations on the diagnosis, initial resuscitation, supportive care and monitoring of patients with sepsis and suspected sepsis.14 They were initially based on the concept of early goal-directed therapy15 and aimed to reduce the global number of sepsis related deaths by a quarter over the next five years. The guidelines have been updated at four yearly intervals and are presented as "bundles of care". They cover the essential interventions for the early diagnosis and treatment of septic shock. Studies have demonstrated that the implementation of these sepsis bundles decreases the crude, in-hospital and 28-day mortality of patients with sepsis and septic shock.1013 Despite this, there has been patchy uptake of the sepsis bundles, especially in resource-restrained environments.38 Only a small percentage of sub-Saharan African institutions have the required facilities, equipment, drugs and disposable materials to implement the SSC guidelines in their entirety.3-8
A number of recommendations have been provided to assist in the management of sepsis in resource-limited settings.16 Leisman et al.17 showed that aggressive adherence to a 3-hour sepsis bundle, which included taking blood cultures before administration of antibiotics, parenteral antibiotics within 180 minutes of diagnosis, lactate measurement within 90 minutes and 30 ml/kg IV crystalloid bolus within 30 minutes of time-zero, is associated with improved survival and cost savings. In the current study, compliance with the components of the 3-hour bundle was only achieved in 56% of cases, yet this did not seem to translate into a difference in clinical outcomes. Although there was a significantly higher rate of admission to ICU in the compliant group, there was no difference between the two groups with respect to hospital length of stay, or mortality. It is difficult to explain these observations. It is possible that these findings might reflect greater disease severity in the patients whose care included compliance with all the metrics of the 3-hour bundle, however the two cohorts were similar in terms of demographics and presenting physiology. The only significant clinical differences between the compliant and the non-compliant cohorts was that more patients in the compliant group had a respiratory rate greater than 22 breaths/minute.
Although this study has limitations, it is one of the few studies to report on the rate of compliance with the 3-hour SSC bundle in patients with surgical sepsis in a resource-limited setting and to attempt to critically review the impact of these bundles of care. The fact that compliance did not translate into improved outcomes is counter-intuitive and there are several potential explanations. Most of the studies which report on improved outcomes in centres in which there is high compliance with the SSC guidelines do not focus solely of patients with surgical sepsis. In patients with surgical sepsis, surgical source control remains paramount. The SSC guidelines, however, focused on early goal-directed therapy and excluded patients who required immediate surgery.15 The SSC guidelines recommend source control within 12 hours in appropriate patients.9 These recommendations have tended to under-emphasise surgical source control, and it is important to be aware of this when implementing these protocols in patients with surgical sepsis.18,199 Delay in achieving surgical source control has been shown to impact negatively on outcomes for surgical sepsis. Azuhata et al.21 showed that in patients with gastrointestinal perforation associated with septic shock, time to source control is a crucial determinant of survival, and that source control may be required as early as 6 hours from admission. In addition, the importance of the impact of time delay to source control on the outcome of surgical sepsis has been emphasised in a number of recent consensus publications.22,23 This is particularly the case in low-resource settings where access to surgical care is limited and delays to definitive treatment may be prolonged. Patients with sepsis in LMIC countries encounter numerous barriers to care and tend to present with advanced disease.8,1819 The SCC bundles are described as useful in the early management of sepsis, and the delays which patients in this study may have experienced prior to presentation may render the bundles less efficacious. These factors all emphasise the need for further ongoing research on the appropriate management of surgical sepsis in our setting.
Conclusion
Compliance with the SCC 3-hour bundle did not seem to improve mortality outcomes in our setting. This observation cannot be adequately explained with our current data and further work looking at management of surgical sepsis in our setting is required. Time to surgical source control is probably the single most important determinant of outcome in patients with surgical sepsis and other aspects of the care bundle are of secondary importance.
Conflicts of interest
The authors declare no conflicts of interest.
Ethics approval
BE 207/09, 221/13
Orcid
MTD Smith © http://orcid.org/0000-0002-6954-153X
JL Bruce φ http://orcid.org/0000-0001-8666-4104
GL Laing © http://orcid.org/0000-0001-8075-0386
DL Clarke © http://orcid.org/0000-0002-6954-153X
REFERENCES
1. Singer M, Deutschmann CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-10. [ Links ]
2. Fleischmann C, Scherag A, Adhikari NK, et al. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am J Respir Crit Care Med. 2016 Feb 1;193(3):257-72. [ Links ]
3. Bhagwanjee S. Sepsis in Low and Middle Income Countries. Critical Care Canada Conference 2013. Available from: http://www.criticalcarecanada.com/presentations/2013/sepsis_in_low-middle_income_countries.pdf. Accessed 23/10/2016. [ Links ]
4. Bhagwanjee S, Scribante J, Perrie H, Paruk F. PISA: the prevalence of infection in intensive care units in South Africa. Crit Care. 2007 March 22; 11(Suppl 2):66. Available from: https://doi.orgV10.1186/cc5226 [ Links ]
5. Jacob ST, West TE, Banura P. Fitting a square peg into a round hole: are the current Surviving Sepsis Campaign Guidelines feasible for Africa? Crit Care. February 2011;15:117. Available from: http://ccforum.com/content/15/1/117 [ Links ]
6. Rello JL, Leblebicioglu H. Sepsis and septic shock in low-income and middle-income countries: need for a different paradigm. Int. J Infect Dis. 2016;11:e0151408. [ Links ]
7. Baelani I, Jochberger S, Laimer T, Otieno D, et al. Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Crit Care. January 2011;15:R10. Available from: http://ccforum.com/content/15/1/R10 [ Links ]
8. Becker JU. Surviving sepsis in low-income and middle-income countries: new directions for care and research. Lancet Infect Dis. Sept 2009;9(9):577-82. Available from: https://doi.org/10.1016/S1473-3099(09)70135-5 [ Links ]
9. Dellinger RP, Levy MM, Rhodes A, Annane D, et al. Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup. Intensive Care Med. 2013 Feb;39(2):165-228. doi: 10.1007/s00134-012-2769-8. Epub 2013 Jan 30. [ Links ]
10. Levy MM, Rhodes A, Hillis GS, et al. Surviving Sepsis Campaign: association between performance metrics and outcomes in a 7.5yr study. Crit Care Med. 2015 Jan;43(1):3-12. doi: 10.1097/CCM.0000000000000723 [ Links ]
11. Damiani E, Donati A, Serafini G, Rinaldi L. Effect of Performance Improvement Programs on Compliance with Sepsis Bundles and Mortality: A Systematic Review and Meta-Analysis of Observational Studies. PLOS One. 2016 May 6; 10(5):e0125827. doi:10.1371/journal.pone.0125827 [ Links ]
12. Levy MM, Dellinger RP, Townsend SR, et al. The surviving sepsis campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010;36:222-231. [ Links ]
13. Gao F, Melody T, Daniels DF, et al. The impact of compliance with 6-hour and 24-hour sepsis bundles on hospital mortality in patients with severe sepsis: a prospective observational study. Crit Care. 2005 Nov 11;9:R764-R770. doi:10.1186/cc3909 [ Links ]
14. Dellinger RP, Carlet JM, Masur H, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 2004;32:858-73. [ Links ]
15. Rivers E, Nguyen B, Havstad S, et al. Early Goal-Directed Therapy Collaborative Group: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-77. [ Links ]
16. Dünser MW, Festic E, Dondorp A, et al. Recommendations for sepsis management in resource-limited settings. Intensive Care Med. 2012 Feb;38:557-74. doi:10.1007/s00134-012-2468-5 [ Links ]
17. Leisman DE, Doerfler ME, Ward MF, et al. Survival Benefit and Cost Savings From Compliance With a Simplified 3-hour Sepsis Bundle in a Series of Prospective, Multisite, Observational Cohorts. Crit Care Med. 2016:XX. doi:10.1097/ ccm.0000000000002184 [ Links ]
18. Ozgediz D, Jamison D, Cherian M, McQueen K. The burden of surgical conditions and access to surgical care in low-and middle-income countries. Bull World Health Organ. 2008 Aug;86(8): 646-7. doi:10.2471/BLT.07.050435 [ Links ]
19. Papali A, McCurdy MT, Calvello EJ. A "three delays" model for severe sepsis in resource-limited countries. Crit Care. 2015;30:861.e9-861.e14. Available from: http://dx.doi.org/10.1016/j.jcrc.2015.04.003 [ Links ]
20. Martinez ML, Ferrer R, Torrents E, et al. Impact of Source Control in Patients With Severe Sepsis and Septic Shock. Crit Care Med. 2017;45:11-19. doi:10.1097/ccm.0000000000002011 [ Links ]
21. Azuhata T, Kinoshita K, Kawano D, et al. Time from admission to initiation of surgery for source control is a critical determinant of survival in patients with gastrointestinal perforation with associated septic shock. Crit Care. 2014;18:R87. Available from: http://ccforum.com/content/18/3/R87 [ Links ]
22. Sartelli M, Chichom-Miferi A, Labricciosa FM, Hardcastle T, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg, 2017;12:29. doi: 10.1186/s13017-017-0141-6 [ Links ]
23. Sartelli M, Kluger Y, Anseloni L, Hardcastle TC, et al. Raising concerns about the Sepsis-3 definitions. World J Emerg Surg. 2018;13:6. doi: 10.1186/s13017-018-0165-6 [ Links ]
 Correspondence:
Correspondence:
Professor Victor Kong
victorywkong@yahoo.com














