Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151
Print version ISSN 0038-2361
S. Afr. j. surg. vol.57 n.2 Cape Town Jun. 2019
http://dx.doi.org/10.17159/2078-5151/2019/v57n2a2972
TRAUMA SURGERY
Advanced radiological investigations and findings amongst community assault victims admitted to a tertiary South African hospital
F du ToitI; SB Griffith-RichardsI; BC van ZylI; RD PitcherII
IDepartment of Radiology, Tygerberg Hospital, Cape Town, South Africa
IIDivision of Radiodiagnosis, Department of Medical Imaging and Clinical Oncology, Faculty of Medicine and Health Sciences, Tygerberg Hospital, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: Community assault (CA) has been increasing in certain Cape Town suburbs over the past decade. There are limited CA-related imaging data. The aim of this study was to review CA-related advanced radiological investigations and findings at a Level 1 South African Trauma Centre.
METHODS: A retrospective study at Tygerberg Hospital, Cape Town, from 1 January through 30 June 2013. All advanced radiological investigations performed on CA victims at the time of admission were retrieved and analysed by patient demographics, imaging investigations and radiological findings.
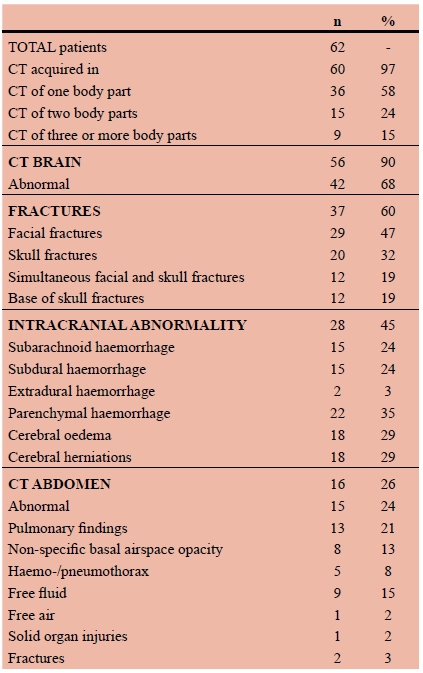
RESULTS: Sixty-two patients (n=62) with a median age of 25 years were included; CT brain was acquired in 90% (n=56) and was abnormal in 68% (n=42). Craniofacial fractures were demonstrated in 60% (n=37), with involvement of the paranasal sinuses in 32% (n=20) and the base of skull in 19% (n=12). Almost half (n=28/62; 45%) had intracranial haemorrhage, which was intra-axial in 36% (n=22/62), extra-axial in 34% (n=21/62) and both intra- and extra-axial in 23% (n=14/62). Cerebral oedema was present in 29% (n=18/62), with herniation in 10% (n=6/62). Non-cranial CT was acquired in 52% (n=32/62), of whom 19 (n=19/32; 59%) also underwent CT brain. CT abdomen was acquired in approximately a quarter of the cohort (n=16/62, 26%), demonstrating abnormalities in 15 (24%). Fifteen cervical spine CTs were performed (n=15/62; 24%) demonstrating no acute bony injury.
CONCLUSION: We recommend a high index of suspicion for severe intracranial injury in CA victims and urgent tertiary referral of those with a depressed level of consciousness. Prospective work is required to determine the long-term outlook for survivors.
Background
South Africa (SA) has amongst the world's highest levels of interpersonal violence. In 2015, there were approximately 36 homicide-related South African deaths per 100 000 people, being the highest rate in Africa and six-times the global average.1
Violent crime is most prevalent in SA's poorest urban communities and is compounded by increasing urbanization and inadequate policing.2,3 Perceiving a failure of law enforcement, communities resort to community assault (CA) or mob justice, severely beating alleged perpetrators.4,5,6 The 2015/2016 SA Police Service Crime Report ascribed 10% of murders to mob justice.7 However, CA is generally not intended to kill, but rather to injure and serve as a deterrent.6
While vigilantism has been documented in many communities across the globe,8,9 it has been increasing in Cape Town over the past decade, with an estimated current rate of 1.1/1000 person years.5,10
Recent reports have enhanced our understanding of CA injuries. Their severity is acknowledged as substantially higher than that of other assaults. Whips of animal hide, rubber or hardened plastic (sjamboks) are generally used. There is resultant severe soft-tissue trauma, rhabdomyolysis (crush syndrome) and acute renal failure. Closed head injury with a depressed level of consciousness is increasingly documented. Although bowel perforation secondary to blunt abdominal trauma has been described, there has been no detailed analysis of abdominal injuries.5,6,11-13 It has been estimated that approximately one-third of victims require management at district hospital or higher levels of care. 5
Notwithstanding this, there are very limited formal CA statistics and a striking paucity of data on the full extent of CA injuries. Although diagnostic imaging is a key component of modern healthcare, with a pivotal role in polytrauma triage, there has been no systematic description of the radiological features of CA. Such knowledge would afford a better understanding of the patterns, extent and severity of CA related injuries, and provide better insights into the long-term outlook of survivors.
Aim
To review CA-related advanced radiological investigations and findings at a Level 1 South African Trauma Centre.
Methods
This retrospective study was conducted at Tygerberg Hospital (TBH) from 1 January through 30 June 2013.
TBH is a 1386-bed Cape Town teaching hospital, affiliated to the Faculty of Medicine and Health Sciences of Stellenbosch University. It is the tertiary referral centre for those Cape Town suburbs most affected by CA, and has a Level 1 Trauma Centre, which manages approximately 22 500 acute cases annually. The radiology department is a digital, filmless and paperless environment. It performs approximately 175 000 examinations per year and has an integrated picture archiving and communication system/radiology information system (PACS-RIS).
Clinicians submit all imaging requests electronically, via the RIS. Clinical details provided by requesting clinicians are included in the radiology report and archived in the institutional PACS, with the relevant images.
Advanced radiological investigations are all studies other than plain radiographs, and include ultrasound, fluoroscopy, computed tomography (CT) and magnetic resonance (MR).
Utilizing embedded data-mining software, customised searches of the TBH PACS-RIS were conducted for all advanced imaging investigations with the term 'community assault', 'mob assault', or 'CA' included in the archived electronic request.
All advanced imaging investigations performed on CA victims at the time of admission to the Trauma Centre were reviewed, in conjunction with selected clinical details from the patient records. The primary end-points of the study were the number, nature and findings of specialised imaging investigations performed for CA victims. Secondary end-points included patient demographics, clinical indications for the respective examinations, the period of tertiary hospitalization and overall survival.
The descriptors of calvarial and intracranial abnormality utilised by Macpherson and coworkers 14 were used to stratify CT brain findings. Comminuted fractures of a single facial or calvarial bone were recorded as one fracture. Plain radiographic examinations and follow-up specialised imaging performed on CA victims were excluded from the analysis. The study was approved by the Health Research Ethics Committee of the Faculty of Medicine and Health Sciences of Stellenbosch University and TBH management.
Results
Overview
Sixty-two male patients (n=62; median age 25 years, interquartile range: 22, 29 years) were included. Sixty (n=60/62; 97%) underwent CT, one a retrograde urethrogram (n=1/62; 1.5%) and three a FAST (focused assessment with sonography in trauma) (n=3/62; 5%). (Figure 1)
CTs involved a single body region in 36 patients (58%), two regions in 15 (24%) and three or more regions in 9 patients (15%). There were 93 CTs in all, averaging 1.5 body regions per patient.
CT brain (CTB) was the commonest investigation, performed in 90% of patients (n=56/62), of whom 14 (14/56; 25%) were intubated. CT abdomen (n=16/62, 26%) and CT cervical spine (n=15/62, 24%) were each performed in approximately a quarter of the cohort. (Figure 1)
The commonest indications for any combination of CT brain/face/cervical spine were a decreased level of consciousness (n=34/56; 61%) and the suspicion of intracranial injury (n=22/56; 39%); the latter due to the extent of superficial scalp and/or facial injuries. More than a third of those undergoing CTB (n=20/56, 36%) had clinical findings suggestive of moderate or severe traumatic brain injury, as evidenced by an admission Glasgow Coma Scale (GCS) of 12 or less.
The leading indications for CT abdomen were definitive abdominal assessment in patients with low GCS (n=14/15, 93%) and/or microscopic haematuria (4/15, 27%).
The average length of tertiary-level hospitalization was 6.6 days (interquartile range: 2, 8), with overall mortality of 13% (8/62, 13%).
Radiological findings
a. CTB
More than two-thirds had abnormal findings (n=42/62; 68%). Fractures (n=37/62, 60%) and intracranial haemorrhage (ICH)(n=28/62; 45%) were the main abnormalities.
(i) Fractures
Facial fractures were demonstrated in almost half the cohort (n=29/62, 47%) and skull fractures in approximately one third (n=20/62; 32%), with coexistence in nearly one-fifth (n=12/62; 19%). The paranasal sinuses were involved in 20 patients (32%), causing pneumocranium in 13 (21%). There was extension to the base of skull (BOS) in 12 patients (19%).
Facial fractures
Sixty-two facial fractures were seen in 29 patients. The orbits (n=16/29; 56%), nasal bones (n=11/29; 38%), zygomatic arches (n=10/29; 16%) and mandible (n=5/29; 8%) were most commonly involved. Fractures were multiple in 19 patients (31%), bilateral in 14 (23%) and trans-facial (Le Fort-type) in 5 (8%). Two patients had BOS involvement. Amongst patients with an isolated facial fracture (n=8/62; 13%), one had intracranial haemorrhage, being a frontal lobe haemorrhagic contusion.
(i.ii) Calvarial fractures
There were 32 calvarial fractures (15 linear, 17 depressed) in 20 patients, mostly in the temporo-parietal region (n=20). Complex fracture patterns were commonly demonstrated (16/62; 26%), characterised by comminution (n=15/62; 24%), depression (n=11/62; 18%), multiplicity (n=9/62; 15%) or involvement of the paranasal sinuses (n=13/62; 21%), BOS (n=9/62; 15%) or cranial sutures (n=7/62; 11%).
There were 15 linear fractures in 11 patients (11/62; 18%), of whom three (n=3/11; 27%) had multiple fractures (1 = three fractures, 2 = two fractures), four (n=4/11; 36%) comminuted fractures and four (n=4/11; 36%) depressed fragments. Five linear fractures (n=5/11; 46%) involved the paranasal sinuses and seven (n=7/11;
64%) the BOS.
Seventeen depressed fractures were seen in 11 patients, of whom four (n=4/11; 36%) had multiple depressed fractures (2 = three fractures, 2 = two fractures) and four (n=4/11; 36%) coexistent linear fractures. Depressed fractures involved the paranasal sinuses in six patients (n=6/11; 55%) and the BOS in three (n=3/11; 27%). All depressed fractures showed severe comminution and were typically associated with intracranial haemorrhage (n=10/11; 91%)
(ii) Intracranial haemorrhage
Almost half the cohort (n=28/62; 45%) had ICH. Intra- (n=22/62; 36%) and extra-axial haemorrhage (n=21/62; 34 %) each occurred in approximately a third of patients, were co-existent in almost a quarter (n=14/62; 23%) and bilateral in approximately one-fifth (n=11/62; 18%).
Extra-axial haemorrhage Traumatic subarachnoid haemorrhage (SAH) and subdural haemorrhage (SDH) were each seen in 15 patients (15/62; 24%), while extra-dural haemorrhage (EDH) was present in two patients (n=2/62; 3%). There were 19 SDHs in 15 patients, of whom four had bilateral SDH and 10 coexistent SAH. Average SDH width was 5 mm (range: 2-13 mm). The EDHs measured 13 mm and 5 mm in maximum width, respectively.
Parenchymal haemorrhage
There were 45 parenchymal haemorrhages in 22 patients (35%), all of whom had at least one haemorrhagic contusion. Thirteen patients (21%) had multiple contusions, with up to 5 contusions in a single patient; nine (n=9/62; 15%) had bilateral contusions and four (6%) an associated parenchymal haematoma. The large majority of patients with haemorrhagic contusions had associated craniofacial fractures (n=20/62; 32%).
(iii) Cerebral oedema
Eighteen patients (n=18/62; 29%) had cerebral oedema (12 = diffuse, 6 = focal). Of those with diffuse oedema, four had imminent tonsillar herniation (n=4/62; 7%) and two trans-tentorial herniation (n=2/62; 3%). None of the patients with focal areas of oedema had cerebral herniation syndromes.
(iv) Midline shift
Midline shift was present in seven patients (7/62; 11%), averaged 6 mm and was complicated by subfalcine herniation in two instances (n=2/7; 29%). SDH was implicated in six patients and a temporal lobe haematoma in the remaining subject.
(v) Correlation of CTB findings with clinical outcome
All patients who demised (n=8) had profoundly depressed levels of consciousness (GCS: 3-8) on presentation. All had CTB evidence of diffuse cerebral swelling and basal cistern attenuation. Seven patients had associated intracranial haemorrhage and six had facial and/or calvarial fractures.
Eighteen CA survivors (18/62, 29%) had evidence of substantial intracranial injury, as shown by the presence of at least two of three key CTB findings, being cerebral oedema, intra- or extra-axial haemorrhage. Five of the eighteen had a profoundly depressed level of consciousness (GCS < 9) at presentation.
CT abdomen
(i) Abdominal injury
While there was free intraperitoneal fluid in nine patients (9/62; 15%), associated organ injury was unusual, with liver laceration and small bowel perforation each seen in a single patient, respectively.
(ii) Thoraco-lumbar fractures
Thoraco-abdominal fractures were present in two patients (3%), involving several lumbar transverse processes in one patient and multiple ribs in the other.
(iii) Basal pulmonary abnormality
Eight patients (13%) demonstrated non-specific dependent basal airspace opacification, which has a broad differential diagnosis, including atelectasis, aspiration, contusion or infection.
(iv) Haemo/pneumothorax
Two patients had a haemopneumothorax, two a pneumothorax and one a haemothorax demonstrated in CT abdomen. Rib fractures were implicated in one patient with a haemopneumothorax.
CT cervical spine
There were no acute cervical spine fractures.
d. Other CT investigations
CTs of other body regions were uncommon (n=6/62; 10%). There were two chest scans, one showing diffuse bilateral airspace opacification, and the other a pneumothorax, airspace disease and a T3 spinous process fracture. One neck CT angiogram (CTA) was normal, one lower limb CT angiogram showed bilateral comminuted ankle fractures but no vascular injury, and 2 wrist CTs were performed for intra-articular fractures, both showed scaphoid fractures and one additional distal radial and ulnar fractures.
e. Ascending urethrogram
The single ascending urethrogram was performed for blood at the urethral meatus and showed a bulbar urethral injury.
f. FAST
Although FAST does not form part of the standard acute trauma imaging protocol of the TBH radiology department, three were requested to assess for free intra peritoneal fluid. One patient had bilateral pleural effusions, but none showed free intra-peritoneal fluid.
Discussion
This first comprehensive analysis of the advanced radiological investigations performed in the triage of severely injured CA victims underscores the healthcare challenge of CA in endemic areas. On average, at a single Cape Town tertiary referral centre, a severely injured young male CA victim (there were no women in the cohort) was admitted every three days in the review period. The predominant mechanism of injury was repeated, blunt force to the face and/or head. It also highlights the pivotal role of CT in this setting, providing new insights into the complex patterns of CA-related craniofacial trauma and the extent of associated intracranial injury.
Substantial, direct force is required to fracture the skull. The force transmitted to the underlying brain can cause surface injury at the impact site, as well as remote cerebral damage.15-20 Linear and depressed skull fractures have different mechanisms of injury. Linear fractures typically result from a blow with a flat object, such as a heavy plank or cricket bat.17,20 With progressive increase in the force of impact, linear fractures may show comminution, and/or extension to the skull base.18,21,22 Of the fifteen linear fractures in our cohort, four showed comminution and seven extension into the skull base, as testament to the substantial force involved.
Depressed fractures mostly result from a blow with a small, round or angular object such as a stone, brick, club (knopkierrie) or hammer, or a kick with a heavy boot. The force is typically concentrated over an area of 5-13 square centimetres.21 Depressed fractures are commonly compound, comminuted and associated with dural tears.18,21,23 The depressed bony fragments are frequently driven into the underlying cerebral cortex,24 predisposing to brain abscess 22,25 and post-traumatic epilepsy.26 All depressed fractures in our cohort showed extensive comminution.
Our finding of similar numbers of linear (n=15) and depressed (n=17) fractures suggests no predominant instrument in CA head trauma, but rather spontaneous use of any implement at hand at the time. In a seminal manuscript almost 70 years ago, Gurdjian and coworkers highlighted the significance of repeated blunt calvarial trauma. Their cadaver studies showed that once the skull absorbs sufficient energy to produce a single, simple linear fracture, the loss of calvarial mechanical integrity renders it substantially more vulnerable to severe disruption when subjected to subsequent, comparable blunt force.17 It is in this context that the repeated, blunt trauma in CA is of particular import.
A direct blow to the calvarium can cause additional brain injury through the acceleration caused by linear and/or rotational forces. Rotational forces are the more clinically significant,29 causing the cerebral hemispheres to swirl within the calvarium.16 This stretches and lacerates axons, tears blood vessels and causes surface contusions as the cerebrum impacts bone.27 Additionally, the shearing strain at the grey-white interface may cause discreet punctate haemorrhages or larger haemorrhagic contusions (gliding contusions).28 Similar forces on bridging vessels in the subarachnoid and subdural spaces cause traumatic SAH and SDH respectively.27
The further a force acts from the head's centre of gravity, the greater the rotational component.15 Thus, lateral forces to the head cause more rotation and are associated with more severe neuropathological changes and worse clinical outcome.31,32,33 Of note, more than 60% of fractures in our cohort (20/32) were in the temporo-parietal region, indicative of a lateral force.
Blows to the face, particularly those with sufficient force to result in a facial fracture, have the potential to cause acceleration/deceleration injuries to the brain. This is especially true if a significant rotational force is applied at a distance from the head's centre of gravity, as in mandibular or zygomatic fractures. These accounted for almost a quarter (15/62; 24%) of facial fractures in our cohort. Additionally, extensive facial fractures may involve the base of skull in the anterior cranial fossa, with complications similar to those encountered in depressed calvarial fractures.34,37 Midface fractures, in particular LeFort type II and III, are also associated with an increased risk of cerebrovascular injury.38 Such fractures were documented in 5 of our cohort (n=5/62; 8 %).
Traumatic Brain Injury (TBI) involves both immediate mechanical damage to the brain parenchyma (primary TBI) and subsequent biochemical insult (secondary TBI).15,27 Neuron hyper-excitability from the primary brain injury initiates a biochemical cascade, causing cerebral oedema. This further increases neuron excitability, propagating a vicious cycle of cerebral damage lasting hours or even days.15 Early management of secondary TBI can significantly alter its course, especially within the first 48 hours. Neuroimaging is key in determining the presence and extent of the primary injuries, and should be seen as central to the acute management of TBI.39 Given the high incidence of primary brain injury amongst CA victims, early referral to an appropriate level of care is essential in decreasing morbidity and mortality.
Of note, one third of CA survivors in our cohort (18/54; 33%) had presentation CTB findings suggestive of substantial TBI, as demonstrated by the presence of at least two of three key CTB findings, being cerebral oedema, intra- or extra-axial haemorrhage. Chronically debilitating complications of TBI include cognitive problems, post-traumatic epilepsy, focal neurological deficits and a persistent vegetative state.16,26,41,42 Thornhill's prospective study of 769 patients with head-injury43 showed that the large majority (78%) of survivors of severe head injury were disabled at one year, and that disability was frequent amongst victims of moderate (54%) and even mild head injuries (51%).43 Prospective work is thus required to determine the long-term outlook for CA survivors.
This study was limited by its reliance on referral details. The omission of the history of CA on some imaging requests could have contributed to slight under-estimation of the number of CA victims and/or CA-related imaging studies in this review. Additionally, although it is known that brain CT can be normal in the acute phase of extensive diffuse axonal injury, despite a profoundly depressed level of consciousness, there were no such cases in our cohort.
Conclusion
This first review of the cross-sectional imaging features of CA highlights the pivotal role of CT in this setting. The high incidence, severity and complex multidirectional pattern of craniofacial injuries in CA have not been previously reported. We recommend a high index of suspicion for severe intracranial injury and urgent tertiary referral for all CA victims with a depressed level of consciousness. Prospective work is required to determine the long-term outlook for CA survivors.
Declarations
Ethics approval: Ethical clearance was obtained from the Health Research Ethics Committee of the University of Stellenbosch with reference number: S16/01/009
Competing interests: The authors declare that they have no competing interests.
Funding: Minimal stationary costs pertaining to this article were covered by the Department of Radiology, Tygerberg Hospital, University of Stellenbosch.
Authors' contributions: BCVZ, RDP and FDT were involved in data acquisition and summarized the patient data into Excel spreadsheets. FDT, RDP and SGR all substantially contributed to conception, design, analysis and interpretation of data, drafting and revising the manuscript. RDP gave final approval for the version of the article to be submitted for publication.
Acknowledgements: None.
REFERENCES
1. World Health Organization. Global health estimates 2015 summary tables: global deaths by cause, age and sex, 20002015. Geneva: WHO, 2016. Available from: http://www.who.int/healthinfo/global_burden_disease/en/. [ Links ]
2. Medical Research Council. Revised burden of disease estimates for the comparative risk factor assessment, South Africa 2000. Methodological Note. Cape Town: South African Medical Research Council, 2006. [ Links ]
3. Ward C, Artz L, Berg J, et al. Violence, violence prevention, and safety: A research agenda for South Africa. S Afr Med J. 2012;102(4):215-8. Available from: http://www.samj.org.za/index.php/samj/article/view/5544/4001 [ Links ]
4. Singh D. Resorting to community justice when state policing fails: South Africa. Acta Criminologica 2005;18(3):43-50. [ Links ]
5. Forgus S, Delva W, Hauptfleisch C, Govender S, Blitz J. Community vs non-community assault among adults in Khayelitsha, Western Cape, South Africa: A case count and comparison of injury severity. S Afr Med J. 2014;104(4):299-301. doi:10.7196/samj.7615 [ Links ]
6. Proctor M, Carter N, Barker P. Community assault - the cost of rough justice. S Afr Med J. 2009;99(3):160-1. Available from: http://www.samj.org.za/index.php/samj/article/view/3125 [ Links ]
7. Phahlane JK. South African Police Service Annual Crime Report 2015/2016: Addendum to the SAPS Annual Report. South Africa: South African Police Service (SAPS), 2016. Available from: https://www.saps.gov.za/services/c_thumbnail.php?id=282 [ Links ]
8. Monaghan R. Community-based justice in Northern Ireland and South Africa. International Criminal Justice Review. 2008;18(1):83-105. doi:10.1177/1057567708316639 [ Links ]
9. Ng'walali PM, Kitinya JN. Mob justice in Tanzania: A medico-social problem. African Health Science. 2006;6(1):36-38. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/ PMC1831959 [ Links ]
10. Herbst CI, Tiemensma M, Wadee SA. A 10-year review of fatal community assault cases at a regional forensic pathology facility in Cape Town, South Africa. S Afr Med J. 2015;105(10):848-52. doi:10.7196/samjnew.8274 [ Links ]
11. Rosedale KJ, Wood D. Traumatic rhabdomyolysis (crush syndrome) in the rural setting. S Afr Med J. 2011;102(10):37-9. doi:10.1136/emj.2010.104208 [ Links ]
12. Smith WA, Hardcastle TC. A crushing experience: The spectrum and outcome of soft tissue injury and myonephropathic syndrome at an Urban South African University Hospital. Afr J Emerg Med. 2011;1(1):17-24. doi:10.1016/j.afjem.2011.04.002 [ Links ]
13. Skinner DL, Laing GL, Bruce J, Biccard B, Muckart DJJ. Validating the utilisation of venous bicarbonate as a predictor of acute kidney injury in crush syndrome from sjambok injuries. S Afr Med J. 2017 Apr 25;107(5):446-50. doi:10.7196/ SAMJ.2017.v107i5.12213 [ Links ]
14. Macpherson BC, Macpherson P, Jennett B. CT evidence of intracranial contusion and haematoma in relation to the presence, site and type of skull fracture. Clin Radiol. 1990;42(5):321-6. doi:10.1016/s0009-9260(05)82145-2 [ Links ]
15. Bauer D, Tung ML, Tsao JW. Mechanisms of traumatic brain injury. Semin Neurol. 2015;35(1):e14-22. doi:10.1055/s-0035-1549095 [ Links ]
16. Dolinak D. Trauma. In: Prayson RA, Goldblum JR (Eds.), Neuropathology 2nd edition. Philadelphia: Elsevier Saunders; 2012. p.75-95. [ Links ]
17. Gurdjian ES, Webster JE, Lissner HR. Studies on skull fracture with particular reference to engineering factors. Am J Surg. 1949;78(5):736-42. doi:10.1016/0002-9610(49)90315-3 [ Links ]
18. Heegaard WG, Biros MH. Skull fractures in adults. In J Grayzel (Ed), UptoDate. Available from: https://www.uptodate.com/contents/skull-fractures-in-adults [ Links ]
19. Hardman JM, Manoukian A. Pathology of head trauma. Neuroimaging Clin N Am. 2002;12(2):175-87. doi:10.1016/ s1052-5149(02)00009-6 [ Links ]
20. Mogbo KI, Slovis TL, Canady AI, Allasia DJ, Arfken CL. Appropriate imaging in children with skull fractures and suspicion of abuse. Radiology. 1998;208(2):521-4. doi:10.1148/ radiology.208.2.9680586 [ Links ]
21. Eurailsafe. Head injury mechanisms. Mira 2002. Available from: http://www.eurailsafe.net/subsites/operas/HTML/Section3/Page3.3.1.2.htm (Accessed 24 January 2018). [ Links ]
22. Giannatempo GM, Scarabino T, Simeone A, et al. CT in Head Injuries. In: Carabino T, Salvolini U, Jinkins JR (eds.), Emergency Neuroradiology. New York: Springer; 2006. p. 13762. [ Links ]
23. Yousem DM, Grossman RI. Head Trauma. In: Thrall JH (Ed), The requisites: Neuroradiology. Philadelphia: Mosby; 2010. p.170-91. [ Links ]
24. Osborn A. Craniocerebral trauma. In Osborn A (Ed), Diagnostic neuroradiology. St Louis: Mosby; 1994. p. 199-247. [ Links ]
25. Jennet B, Miller JD. Infection after depressed fracture to the skull. Implications for management of nonmissile injuries. J Neurosurg. 1972;36(3):333-9. Available from: http://doi.org/10.3171/jns.1972.36.3.0333 [ Links ]
26. Evans RW, Schachter SC. Post-traumatic seizures and epilepsy. In Wilterdink JL (ed), UptoDate. Available from: https://www.uptodate.com/contents/post-traumatic-seizures-and-epilepsy [ Links ]
27. Hemphill JC. Traumatic brain injury: Epidemiology, classification, and pathophysiology. In Wilterdink JL (ed), UptoDate. Available from: https://www.uptodate.com/contents/traumatic-brain-injury-epidemiology-classification-and-pathophysiology [ Links ]
28. Lindenberg R, Freytag E. Morphology of cerebral contusions. AMA Arch Pathol. 1957;63(1):23-42. [ Links ]
29. Zhang J, Yoganandan N, Pintar FA, Gennarelli TA. Role of translational and rotational accelerations on brain strain in lateral head impact. Biomed Sci Instrum. 2006;42:501-6. [ Links ]
30. Ommaya AK, Gennarelli TA. Cerebral concussion and traumatic unconsciousness. Correlation of experimental and clinical observations of blunt head injuries. Brain. 1974;97(4):633-54. doi:10.1093/brain/97.4.633 [ Links ]
31. Gennarelli TA, Thibault LE, Adams JH, Graham DI, Thompson CJ, Marcincin RP. Diffuse axonal injury and traumatic coma in the primate. Ann Neurol. 1982;12(6):564-74. doi:10.1002/ ana.410120611 [ Links ]
32. Zhang L, Yang KH, King AI. Comparison of brain responses between frontal and lateral impacts by finite element modeling. J Neurotrauma. 2001;18(1):21-30. doi:10.1089/089771501750055749 [ Links ]
33. McIntosh AS, Patton DA, Fréchède B, Pierré PA, Ferry E, Barthels T. The biomechanics of concussion in unhelmeted football players in Australia: a case-control study. BMJ Open. 2014;4(5):e005078. doi:10.1136/bmjopen-2014-005078 [ Links ]
34. Keenan HT, Brundage SI, Thompson DC, Maier RV, Rivara FP. Does the face protect the brain? A case-control study of traumatic brain injury and facial fractures. Arch Surg. 1999;134(1):14-7. doi:10.1001/archsurg.134.1.14 [ Links ]
35. Salentijn EG, Peerdeman SM, Boffano P, van den Bergh B, Forouzanfar T. A ten-year analysis of the traumatic maxillofacial and brain injury patient in Amsterdam: incidence and aetiology. J Craniomaxillofac Surg. 2014;42(6):705-10. doi:10.1016/j.jcms.2013.12.008 [ Links ]
36. Kloss F, Laimer K, Hohlrieder M, et al. Traumatic intracranial haemorrhage in conscious patients with facial fractures-a review of 1959 cases. J Craniomaxillofac Surg. 2008;36(7):372-7. doi:10.1016/j.jcms.2007.12.002 [ Links ]
37. Rajandram RK, Syed Omar SN, Rashdi MFN, Abdul Jabar MN. Maxillofacial injuries and traumatic brain injury-a pilot study. Dent Traumatol. 2014;30(2):128-32. doi:10.1111/edt.12052 [ Links ]
38. Mayersak RJ. Initial evaluation and management of facial trauma in adults. In Grayzel J (ed), UptoDate. Available from: https://www.uptodate.com/contents/initial-evaluation-and-management-of-facial-trauma-in-adults [ Links ]
39. Lee B, Newberg A. Neuroimaging in traumatic brain imaging. NeuroRx. 2005;2(2):372-83. doi:10.1602/neurorx.2.2.372 [ Links ]
40. Johnson PL, Eckard DA, Chason DP, Brecheisen MA, Batnitzky S. Imaging of acquired cerebral herniations. Neuroimaging Clin N Am. 2002;12(2):217-28. doi:10.1016/s1052-5149(02)00008-4 [ Links ]
41. Whiteneck GG, Gerhart KA, Cusick CP. Identifying environmental factors that influence the outcomes of people with traumatic brain injury. J Head Trauma Rehabil. 2004;19(3):191-204. doi:10.1097/00001199-200405000-00001 [ Links ]
42. Rabinowitz AR, Levin HS. Cognitive sequelae of traumatic brain injury. Psychiatr Clin North Am. 2014;37(1):1-11. doi:10.1016/j.psc.2013.11.004 [ Links ]
43. Thornhill S, Teasdale GM, Murray GD, McEwen J, Roy CW, Penny KI. Disability in young people andadults one year after head injury: prospective cohort study. BMJ 2000;320(7250):1631-5. doi:10.1136/bmj.320.7250.1631 [ Links ]
 Correspondence:
Correspondence:
F du Toit
dutoit.fran@gmail.com














