Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.56 no.3 Cape Town Set. 2018
http://dx.doi.org/10.17159/2078-5151/2018/v56n3a2325
GENERAL SURGERY
Surgery for giant tumours of the breast: a 15 year review
M DayaI; T BalakrishnanII
IDepartment of Plastic and Reconstructive Surgery, Nelson R Mandela School of Medicine, Inkhosi Albert Luthuli Central Hospital, University of KwaZulu-Natal
IIPlastic and Reconstructive Surgeon in private practice
ABSTRACT
BACKGROUND: Giant tumours of the breast tend to occur in the adolescent age group. Racial predilection has been noted in the literature. The mass often occupies most of the breast, leading to its distortion. Many authors have advocated a mastectomy for benign tumours that severely distort the breast. Giant benign tumours when treated by simple excision risk persistence of asymmetry. To avoid this asymmetry, some authors have resorted to excision and immediate reduction mammaplasty. The aim of this retrospective study was a report on giant tumours of the breast presenting to a plastic surgery unit and to analyse demographic factors, clinical presentations, tumour pathology, management, complications, as well as patient and breast outcomes.
METHODS: Medical records of patients with giant tumours were retrospectively analysed for assessing demographic factors, clinical presentation, tumour pathology, the technique of surgery performed and patient and breast outcomes in a single hospital setting. Breast outcomes were rated by panel of 4 experienced plastic surgeons using the 4 Point Likert scale. Their ratings were statistically analysed for inter-rater agreement.
RESULTS: Twenty-three subjects were identified to have giant tumours of the breast. Of these South African patients, 19 were black, 3 were Indian and 1 was of mixed ethnicity. The age range was 12-49 years(y) with an average of 19y. All masses were palpable. The final pathological diagnosis was fibrocystic disease in 3, giant fibroadenoma in 14, phyllodes tumour in 4, and hamartoma in 2. The size range was 10-45 cm with a median size of 18 cm. All but one patient had simple excision followed by immediate reduction mammaplasty. Twenty patients were assessed after operation. A minimum of 1 to a maximum of 4 patients per reviewer showed unsatisfactory outcomes and a minimum of 18 to a maximum of 21patients per reviewer showed satisfactory to excellent outcomes. The overall agreement between assessors for this was 84%.
CONCLUSION: Benign giant tumours (> 10 cm) of the breast are suitably managed by excision of the mass and a reduction mammoplasty technique of reconstruction.
Keywords: Giant tumour breast reduction mammaplasty, giant fibroadenoma of breast, phyllodes tumour, hamartoma breast.
Introduction
Giant tumours of the breast can be arbitrarily defined as greater than 5 cm in diameter or as greater than 10 cm in diameter.1,2 They commonly present in the adolescent age group with unilateral breast hypertrophy, often associated with breast distortion. The differential diagnosis commonly includes fibroadenoma, phylloides tumours and lipoma.3-5 In a review of 15 publications, Neinstein found that giant benign phylloides tumours and giant fibroadenoma made up less than 1 percent of all benign tumours of the adolescent breast.6,7 This prevalence maybe higher in ethnic groups of Negroid and Indian descent.18 Chhanda assessed fibroadenoma in women in Ghana and found that 22% (n = 31) were of a giant variant (> 5 cm).9 This was more than the published data from African-American women.10 Naidu's study of 358 patients presenting to a general surgical clinic over a 6-year period, the Durban region of Kwazulu-Natal as those in the current study found that 47 (13%) had giant fibroadenoma (> 5 cm).1 Forty-two of their 47 patients were black South Africans and 5 Indian South Africans.
Strategies in management include lumpectomy, lumpectomy and reduction mammoplasty, mastectomy and mastectomy with reconstruction. A mastectomy has been advocated for benign giant tumours especially when associated with severe breast distortion, lack of breast tissue and thin breast skin.11 Simple lumpectomy when feasible is associated with a risk of persistent asymmetry. Incisions include direct, periareolar, and inframammary fold. Combining a reduction mammaplasty technique with a lumpectomy can restore the size and shape of the breast to match the contralateral normal one.5, 12-13 In this study the definition of greater than 10 cm for giant tumours of the breast was chosen to identify the breast distortion, enlargement and asymmetry for unilateral masses. Simple removal of a giant benign tumour (> 10 cm) is unlikely to correct these problems so that these patients are more likely to be referred to a plastic surgeon as were the cases in this study.
Aim
The aim of the study was a report on giant tumours of the breast presenting to a plastic surgery unit and to analyse demographic factors, clinical presentations, tumour pathology, management, complications, as well as patient and breast outcomes.
Materials and methods
Identification of patients
A retrospective database search was performed for patients with giant breast tumours referred to and managed at the Inkhosi Albert Luthuli Central Hospital (IALCH), Department of Plastic and Reconstructive Surgery, Durban. An ethical approval number, BCA 083/12 was obtained from the university's Biomedical Research Ethics committee. Data was obtained from electronic and medical files for the period of review from the year 1997 to 2012.
Method of analysis
Analysis included age, ethnicity, clinical presentation, postoperative histological findings, surgical method, complications, and aesthetic outcome. The aesthetic outcome of the breasts was rated by 4 independent senior reviewers (plastic surgeons qualified for > 9 y and who had no association with the department in which patients were managed). The reviewers were shown frontal views of comparable preoperative and final postoperative photographs of the patients. The rating scale that was used was the four point Linkert Scale (Harvard Scale) (see Table 1). This scale was modified to rate those breasts operated on for bilateral disease. Further the Fair group in the 4 Point Linkert scale was subdivided into categories A and B (see Table 1). Descriptive statistical analysis was done on the remainder of the above listed variables using Excel 2013 (Microsoft Corporation).
Method of statistical analysis of breast outcome
The breast outcomes were rated into one of 5 categories (see Table 1). For the purposes of analysis these categories were regrouped into 3, viz. excellent, satisfactory (categories Good and Fair A combined) and unsatisfactory (categories Fair B and Poor combined). Satisfactory therefore represented a breast that was aesthetically pleasing and acceptable after mass removal irrespective of its match to the contralateral one. Finally, "satisfactory" and excellent were combined and compared to "unsatisfactory". The percent agreement and Kappa coefficient and the p value for Kappa > 0 are reported. Kappa, which takes into account the possibility of agreement by chance, was used as the measure of inter-rater agreement for qualitative items
Description of local standard of care
In all cases core-needle biopsy was done preoperatively for histological assessment. The tumour excision and reconstruction by reduction mammoplasty techniques was performed by the principal author in all patients with masses greater than 10 cm diameter.
Technique of mass excision and reduction mammaplasty
Two sample cases are used to demonstrate the technique. Case 1 demonstrates a regular approach and Case 2 an adaptation in the technique, customized to overcome associated breast skin ulceration.
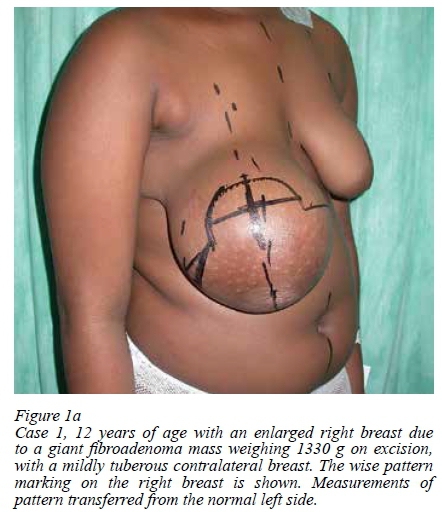
Case 1
The patient is marked in the standing position (Figure 1a). The primary aim of the surgery when achievable is to remove the mass and perform a reduction mammoplasty to match the normal opposite breast without a contralateral symmetrisation procedure. A Wise pattern is used. The limb measurements of the Wise pattern and the angle opening is simulated to match the opposite normal breast. The nipple areolar complex (NAC) position is matched and marked by elevating the breast with the hand to compensate for the skin stretch related to the size and weight of the mass. The actual marking for the new position of the NAC then as seen in its natural position, once hand support is removed, can easily be 3-4 cm lower than the opposite side. This manoeuvre overcomes creating a high riding nipple that can accompany skin shrinkage brought upon by weight reduction and removal of the source of tissue expansion stimulus that follows tumour excision.
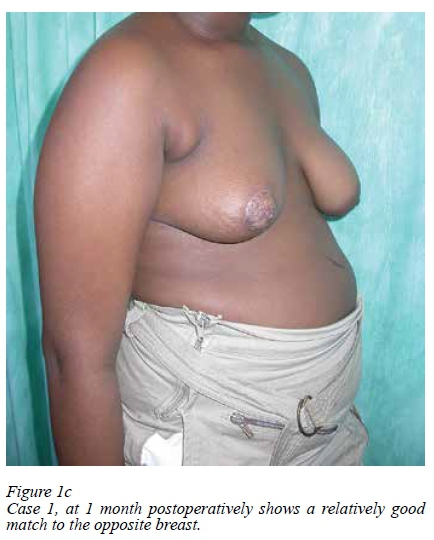
At surgery the entire section within and below the central keyhole portion of the Wise pattern is de-epithelialized, retaining a predetermined appropriately size matched NAC on a consolidated superomedial and superolateral blood supply (referred to as zone 1). The skin below the NAC carrying pedicle is excised full thickness (referred to as zone 2). The tumour mass is then removed via a transverse incision made between zone 1 and zone 2 (Figure 1b). The NAC carrying pedicle although thin, is well vascularised. Zone 2 of the breast remains vascularized by its preserved attachment to the inframammary fold. Breast tissue from this zone 2 is draped superiorly, covering and suturing it to the pectoralis muscle. The Wise pattern is then closed in the standard way anterior to the zone 2 breast tissue. Excision of any portion of the breast and subcutaneous tissue is to be avoided to maximise volume. If a prediagnosed non-benign mass requiring wide local excision is being treated, breast volume for reconstruction by reduction mammaplasty could be insufficient. In this case an appropriate technique of managing the tumour followed by an alternative reconstruction method if desired, should be considered. In this sample case demonstrated here, a good result was obtained without the need for a contralateral symmetrisation procedure (Figure 1c).

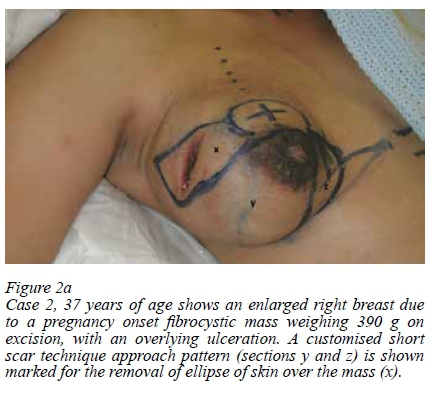
Case 2
In this case demonstration, an upper outer quadrant breast skin ulcer required a customised reduction mammaplasty approach. The skin reduction was modified to a J shaped short scar technique with the long limb of the J closure running along the lateral aspect of the inframammary fold. The NAC carrying flap, with overlying skin, was designed to be carried on an inferolateral blood supply (Figure 2a). Inferomedial to the NAC pedicle, a crescent of skin was de-epithelialized (Figure 2b). The breast mass with its overlying ulcer and surrounding ellipse of skin, superior to the NAC pedicle, was excised. In closing the created wound, the NAC carrying pedicle with overlying skin filled the outer quadrant defect created by the removal of the mass. An early postoperative result in this case showed a good result (Figure 2c).


Results
Twenty-three patients with giant tumours of the breast were identified. Of these South African patients, 19 were black, 3 were Indian and 1 was of mixed ethnicity. The age range was 12-49 years(y) with an average of 19y and a median of 18y. All patients complained of pain or discomfort in the breast and all had palpable masses. Two breasts had overlying skin ulcerations. In the 20 patients with unilateral masses, asymmetry was an obvious clinical feature. In 3 patients, masses were present bilaterally and the breast enlargement was more or less equal. The final pathological diagnosis in this group was fibrocystic disease in 2 patients and giant fibroadenoma in the other one. In the group with unilateral disease, the diagnosis was giant fibroadenoma in 16, benign phyllodes tumour in 3, malignant phyllodes tumour in 1, fibrocystic disease in 1 and hamartoma in 2 patients. In this group, 2 cases, one with a hamartoma and the other with a fibrocystic tumour, the onset of the growth was during pregnancy. The median size was (18 x 16 x 7 cm) with a range of (10 x 9 x 8 cm) to (45 x 22 x 10 cm). The median weight of the tumour was 990 g with a range of 245-3800 g. The mean weight was 1291 g.
Follow-up ranged from 1-60 months with an average of 13 months and median of 7months. All patients underwent removal of the mass by extracapsular excision. All patients except one, underwent reduction mammoplasty to reconstruct the breast. The exception was a case in the series with the smallest mass (diameter = 10 cm) and the nipple was minimally ptotic. The mass was removed through a superior periaerolar incision.
Twenty-one of the 23 patients had their breast outcomes rated. Two patients were excluded because they both did not have both preoperative and postoperative photographic records. The scores given by each reviewer as per rating scale (Table 1) are shown in Table 2. Reviewer combined scores and their means are shown in Table 3.
On statistical analysis all four raters agreed 48% (10/21) of the time; three raters agreed 33% (7/21); two raters 14% (3/21) and in only one case did three raters disagree. Therefore, in 81% of patients, the majority of raters agreed. Overall there was 70% agreement which is considered "substantial". Because there were only three regrouped categories and the Kappa adjusts for chance agreement, the Kappa Coefficient was 36.2% (p < 0.001) which according to the benchmark is "fair". Consistent with the above, Kappa was the highest for "Excellent" (kappa = 48.5%) and lowest for "Satisfactory" (kappa = 24%). If "Satisfactory" and "Excellent" are compared to "Unsatisfactory", the agreement is 84% which is "Almost Perfect", however the kappa is 24% (p < 0.003) which is again "fair".
Landis and Koch (1977) suggest Coefficient Interpretation as below14:
< 0.00 Poor
0.00 to 0.20 Slight
0.21 to 0.40 Fair
0.41 to 0.60 Moderate
0.61 to 0.80 Substantial
0.81 to 1.00 Almost Perfect
On clinical assessment, 4 patients had postsurgical asymmetry. Two patients were preselected to have a second stage contralateral breast symmetrisation procedure because it was thought that without it, symmetry could not be achieved. In the first patient, in addition the reconstructed breast "bottomed out" with a high riding nipple. A bilateral mastopexy was planned to remedy the situation but the patient defaulted follow-up. In the second patient, despite a good immediate breast result on the side with the tumour, the patient did not present for the 2nd stage. In the remaining 2 patients, symmetrisation was not planned. They were aged 13 and 15 years respectively and looked symmetrical on early follow-up. But on long term follow-up, at 3 years and 2 years respectively, a significant contribution to the asymmetry were the ptotic changes in the unoperated normal breast and in one patient there was also some bottoming out noted in the reconstructed breast.
In one patient, 24 years of age, with a preoperative diagnosis of a phyllodes tumour, malignancy was only established on complete excision of the breast mass. The patient was managed further by adjuvant radiotherapy. At one-year follow-up, local control was achieved but the patient did not return for further reviews.
Total NAC necrosis occurred in 3 breasts. Two of these occurred in a single patient with bilateral disease with mass excision of weight equalling 3800 g on each side. The nipple to sternal notch distance was greater than 40 cm. Bilateral haematoma formation requiring surgical evacuation, further compromised the NAC blood supply. The third case of nipple necrosis occurred in a patient who had a simultaneous removal of a large axillary breast (9 x 8 x 4 cm) together with the reduction mammoplasty.
Discussion
Giant fibroadenomas most commonly present in the adolescent age group. In our series both the benign phyllodes and the giant fibroadenoma showed an adolescent age distribution range of 12-20 years. Furthermore, 70% of giant fibroadenoma presented in the age range of 13-16 years. Uboro in his series of treating 22 patients with giant fibroadenomas found that 73% were in the 12-18 years age group.15
Phyllodes tumours are seen predominantly in the 4th decade of life. It is considered to be rare in adolescents and according to Erginal only 20 are reported in the literature.16 We report 3 benign cases of phyllodes tumours in our series. Histologically phyllodes tumours are differentiated from fibroadenoma by the former containing leaf-like fronds and stromal pleomorphism and cellularity. The degree of cellularity and mitotic count is responsible for the tumour grading into benign, borderline or malignant. In practice, the distinction between benign phyllodes and giant fibroadenoma is not always easy. Nambiar et al. suggested that despite a malignant histological grading, these tumours have been found to be strictly benign in behaviour in patients under the age of 20 years.11 Barrio reviewed 293 cases and showed no correlation of grading to local recurrence. The most important predictor was positive margins.17 Therefore in the one patient, a 24-year-old (referred to under results), with inadequate margins (< 1 cm), treatment by adjuvant radiotherapy only, seemed reasonable as opposed to the recommended treatment of mastectomy for a malignant phyllodes tumour.
The role of adjuvant radiotherapy for malignant phyllodes tumour of the breast (MPTB) is controversial. This emanates from the rarity of the condition and the low number of patients who receive adjuvant irradiation. Macdonald on analysing SEER data with 821 patients with MPTB found that women undergoing wide excision had similar cancer specific mortality compared with those who received mastectomy.18 Kim on analysing SEER data for period 1983-2013 with 1974 patients found that patients with more adverse prognostic factors underwent adjuvant radiotherapy. Irrespective of whether the surgical procedure was mastectomy or breast conserving surgery (BCS), the outcome for the radiotherapy group was not inferior to non-radiotherapy group.19 Mitus on analysing their data on 70 patients with MPTB found support for the use of BCS. It was concluded that mastectomy is indicated only if tumour-free margins cannot be obtained by BCS. The 5-year no evidence of disease survival rate was equal for the BCS and adjuvant radiotherapy to mastectomy.20 Barth in a prospective multi-institutional study comprising of 46 patients concluded that excision with negative margins for borderline and malignant phyllodes tumour combined with adjuvant radiotherapy was very effective treatment for local control.21 Another study analysing SEER data over a period 2000-2012 with 1238 patients with MPTB showed over time an increasing number of women received adjuvant radiotherapy, but without a randomised control trial, there may be a lack of level one evidence to support the National Comprehensive Cancer guidelines and appropriate management.
Our series also included two other rare causes of giant tumours, viz. hamartoma and fibrocystic disease/ fibroadenosis.22,23
In Cerrato's retrospective chart review of 46 patients with giant fibroadenomas, 41 of them underwent a simple enucleation of the tumour, four underwent a wide local excision of the tumour and one underwent a mass excision with a reduction mammaplasty. The commonest incision made for removal of the tumour was a periareolar incision (n = 31).24 In their survey of breast outcome, only 3 patients reported asymmetry leading them to conclude that caution should be exercised before recommending immediate breast reconstruction. In the Cerrato study giant fibroadenoma was defined as > 5 cm and the mean size in his review was 7.4 cm. In the current series the mean size of the tumour was 18 cm and all but one patient with a tumour size of 10 cm were offered an immediate reduction mammoplasty reconstruction. The size of the mass determines the indication for a simple excision or excision followed by an immediate reduction mammoplasty reconstruction to avoid breast deformity and the need for secondary revisional surgery.
When feasible, primary aim in treating unilateral disease with regards to aesthetic outcome was achieved by a reduction mammoplasty to match the opposite normal side without a planned immediate or a second stage symmetrisation procedure. The key step in planning, to avoid nipple position asymmetry post reduction mammoplasty, was to mark the nipple position lower (up to 4 cm) relative to the normal contralateral side. This step was vital to allow for the skin retraction that follows the tumour removal. NAC positioning and shaping of the breast were not planned in accordance with measurement guidelines of a classical reduction mammoplasty to achieve aesthetic ideals. Using conventional guidelines would deliver a good individual breast outcome but not symmetry. Weinzweig's case is an illustration of this.22 Despite this strategy, 4 cases had asymmetrical outcomes. In 2 of these cases, second stage symmetrisation was planned because the normal opposite breast had grade 3 ptosis. In the other 2 cases, despite a good initial symmetry, on longterm follow-up a change in the shape of the unoperated breast occurred as the teenager grew older and symmetry was reduced. Operating on immature breasts in adolescents can therefore predispose to poor long-term aesthetic outcomes.
The limitations of this study include subjective assessment of aesthetic outcome and the limited time of follow-up. However, the use of expert reviewers to rate results qualitatively did show a substantial agreement. Kappa which measures the possibility of chance showed lesser scores: with an expert panel rating outcomes, the Kappa scores may be of lesser importance. It was not possible to measure patient perception of outcomes because median follow-up of 7 months is short so that changes in the breast are not seen.
Regarding the technique of reduction mammoplasty following giant tumour excision, the Wise pattern design seems to be reproducible from patient to patient. Because large tumours are likely to always "bottom out" in the breast, the dermal pedicle carrying the NAC is best planned suspended from the key hole of the Wise pattern. As demonstrated in sample case 2, modifying the Wise pattern flaps is necessary in accommodating for breast ulcers and the relative ratio of mass to breast size in order to maintain viability of all flaps. In general, the NAC viability in the cohort of cases was very good despite very thin long dermoglandular pedicles. The 3 breasts with loss of the NAC had contributing factors of very large masses in 2 (with a greater than 40 cm sternal notch to nipple distance) and in the 3rd case axillary breast removal was done simultaneously. The inherent risk of reduced blood supply to the NAC for very ptotic breasts is real but we did not expect NAC loss with the 3rd case. NAC loss could have been avoided by using a free NAC graft and perhaps by delaying the surgical removal of the large axillary breast.
Conclusion
A simple mastectomy should only be employed as a first line management of benign giant tumours (>10 cm) of the breast, if a significant amount of normal breast tissue and/or skin is absent. Excision of the mass and a reduction mammaplasty technique of reconstruction should be considered for benign tumours greater than 10 cm. The described technique preserves residual normal breast tissue volume and breast symmetry can be frequently achieved. Removal via an inframammary fold or periareolar incisions is probably most useful for benign breast tumours less than 10 cm.
REFERENCES
1. Naidu A, Thomson S, Nirmul D. Giant fibro-adenomas in black and Indian adolescents. S Afr J Surg. 1989;27(5):171-2. [ Links ]
2. Liang MI, Ramaswamy B, Patterson CC, McKelvey MT, Gordillo G, Nuovo GJ, et al. Giant breast tumors: Surgical management of phyllodes tumors, potential for reconstructive surgery and a review of literature. World J Surg Oncol. 2008;6. [ Links ]
3. Ramirez-Montano L, Vargas-Tellez E, Dajer-Fadel WL, Espinosa Maceda S. Giant lipoma of the breast. Arch Plast Surg. 2013;40(3):244-6. [ Links ]
4. Zayen S, Amouri H, Dhouib M, Trigui D, Ben Ayed B, Guermazi M. Giant phyllodes tumor of the breast: Consequence of carelessness. Acta Oncol. 2011;50(3):468-U183. [ Links ]
5. Daya M, Mahomva O, Madaree A, Conwright K. Reduction mammoplasty in cases of giant fibroadenoma among adolescent females - Case reports and literature review. S Afr J Surg. 2003;41(2):39-43. [ Links ]
6. Chang DS, McGrath MH. Management of benign tumors of the adolescent breast. Plast Reconstr Surg. 2007;120(1):13e-9e. [ Links ]
7. Neinstein LS. Breast disease in adolescents and young women. Pediatr Clin North Am. 1999;46(3):607-29. [ Links ]
8. Organ Jr CH, Organ BC. Fibroadenoma of the female breast: a critical clinical assessment. J Natl Med Assoc. 1983;75(7):701. [ Links ]
9. Bewtra C. Fibroadenoma in women in Ghana. Pan Afr Med J. 2009;2(1). [ Links ]
10. Oluwole SF, Freeman HP. Analysis of benign breast lesions in blacks. Am J Surg. 1979;137(6):786-9. [ Links ]
11. Nambiar R, Kannan Kutty M. Giant fibro-adenoma (cystosarcoma phyllodes) in adolescent females-a clinicopathological study. BJS. 1974;61(2):113-7. [ Links ]
12. Chepla KJ, Armijo BS, Ponsky TA, Soltanian HT. Benefits of immediate dermoglandular preserving reconstruction following giant fibroadenoma excision in two patients. JPRAS. 2011;64(9):E244-E7. [ Links ]
13. Grossman J, Menes T, Lahat G, Gur E, Weiss J, Barnea Y. Use of the Oncoplastic Reduction Pattern Technique Following Removal of a Giant Breast Lipoma. Ann Plast Surg. 2011;67(2):106-8. [ Links ]
14. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-74. [ Links ]
15. Ugburo AO, Olajide TO, Fadeyibi IO, Mofikoya BO, Lawal AO, Osinowo AO. Differential diagnosis and management of giant fibroadenoma: comparing excision with reduction mammoplasty incision and excision with inframammary incision. J Plast Surg Hand Surg. 2012;46(5):354-8. [ Links ]
16. Erginel B, Celet Ozden B, Yesil Onder S, Yuksel S, Gun Soysal F, Celik A, et al. Management of a Benign Phyllodes Tumor in a 13-Year-Old Girl with Trans-position of the Nipple Areola Complex and Breast Reconstruction. Acta Chir Belg. 2015;115(3):256-9. [ Links ]
17. Barrio AV, Clark BD, Goldberg JI, Hoque LW, Bernik SF, Flynn LW, et al. Clinicopathologic features and long-term outcomes of 293 phyllodes tumors of the breast. Ann Surg Oncol. 2007;14(10):2961-70. [ Links ]
18. Macdonald OK, Lee CM, Tward JD, Chappel CD, Gaffney DK. Malignant phyllodes tumor of the female breast: association of primary therapy with cause-specific survival from the Surveillance, Epidemiology, and End Results (SEER) program. Cancer. 2006;107(9):2127-33. [ Links ]
19. Kim YJ, Kim K. Radiation therapy for malignant phyllodes tumor of the breast: An analysis of SEER data. Breast (Edinburgh, Scotland). 2017;32:26-32. [ Links ]
20. Mitus J, Reinfuss M, Mitus JW, Jakubowicz J, Blecharz P, Wysocki WM, et al. Malignant phyllodes tumor of the breast: treatment and prognosis. Breast J. 2014;20(6):639-44. [ Links ]
21. Barth RJ Jr, Wells WA, Mitchell SE, Cole BF. A prospective, multi-institutional study of adjuvant radiotherapy after resection of malignant phyllodes tumors. Ann Surg Oncol. 2009;16(8):2288-94. [ Links ]
22. Weinzweig N, Botts J, Marcus E. Giant hamartoma of the breast. Plast Reconstr Surg. 2001;107(5):1216-20. [ Links ]
23. Zhang H, Wang X-L, Ren W-D, Shi T-M. Giant Fibroadenomatoid Hyperplasia of the Breast: A Case Report. Gynecol Obstet Invest. 2014;77(2):134-6. [ Links ]
24. Cerrato FE, Pruthi S, Boughey JC, Simmons PS, Salje B, Nuzzi LC, et al. Intermediate and Long-term Outcomes of Giant Fibroadenoma Excision in Adolescent and Young Adult Patients. Breast J. 2015;21(3):254-9. [ Links ]
 Correspondence:
Correspondence:
Mahendra Daya
dayam@iafrica.com














