Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.56 no.2 Cape Town jun. 2018
ABSTRACTS
46th Meeting of The Surgical Research Society of Southern Africa
THE ROLE OF MOODLE-BASED SURGICAL SKILLS ILLUSTRATIONS USING 3D ANIMATIONS IN UNDERGRADUATE TRAINING - EXPERIENCE IN BOTSWANA
Motsumi MJ, Alemayehu GB, Ayane G
Department of Surgery, University of Botswana School of Medicine
Introduction: The cost of acquiring and maintaining customised models for procedures is prohibitive. The use of patients is not always possible. As a result, static media (e.g. PowerPoint) are used to teach procedure techniques, the method herein referred to as "traditional teaching". The literature suggests that 3D-animations are an option.
Aim(s): To find out whether there is a difference in satisfaction level and understanding between undergraduate students taught using 3D-animations vs. traditional teaching.
Methods: This is a one-year prospective comparative study was conducted at the Department of Surgery, University of Botswana. Ethical approval was granted. Participants (3rd and 5th year students) voluntarily consented. They were randomly assigned to groups A (animation) and B (traditional teaching). Five procedures were selected from the curriculum. The procedure animations, pre- and post-tests and the survey were hosted on Moodle and results captured on the back-end database. The study design is shown in the figure below.
Results: There were 88 participants. The mean difference of the pre- and post-test marks was significant for both the animation and the traditional teaching methods [t (44) = 4.532, p < 0.001; t (44) = 9.975, p < 0.001, respectively] using the paired sample t-test. However, this mean difference was significantly higher in the animation group [t (88) = -4.101, p < 0.001] using the independent samples t-test. On a scale of 1-10 (worst - superb), students gave the traditional teaching method a median rating of 5 (average) vs. 8 (best) for the animation method. Students gave the combination of the two teaching methods a median rating of 10 (superb). All students recommended the adoption of the animation teaching modality with 81/88 highly recommending it.
Conclusion/Recommendations: Students have a better level of understanding and a higher level of satisfaction when taught using 3D animations vs. the traditional teaching method. Students highly recommend the use of both modalities for augmentation.
VASCULAR COMPONENT - BREAST CANCER CELL INTERACTION INDUCES EPITHELIAL -MESENCHYMAL TRANSITION AND HEIGHTENS THROMBOTIC ENVIRONMENT
Pather K1, Dix-Peek T2, Mak D1, Klonaros D1, van der Spuy WJ1, Duarte R2, Augustine TN1
1School of Anatomical Sciences
2Department of Internal Medicine, School of Clinical Medicine Faculty of Health Sciences, University of the Witwatersrand, JHB, South Africa
Background: Thromboembolic complications are the second most common cause of death in breast cancer patients, typically occurring during metastatic spread. Transforming growth factor (TGF)-P1 is linked with heightening risk for thrombotic complications, as well as facilitating epithelial-mesenchymal transition (EMT).
Aim: We investigated these phenomena by assessing the ability of vascular components, platelet-rich plasma (PRP) and whole blood (WB), to induce EMT in MCF-7 hormone-dependent breast cancer cells, and amplify thrombosis, by assessing ultrastructural changes and TGF-P1 expression.
Methods: MCF-7 cells were cultured under standard conditions, followed by co-culture with PRP or WB obtained from six healthy volunteers (Wits University Human Research Ethics Committee clearance #M140155). Cells were processed for real-time PCR, electron microscopy, and immunocytochemistry. Micrographs were qualitatively analysed, while TGF-P1 immunolocalisation was quantified using CellProfiler software. TGF-P1 immunolocalisation and mRNA expression data were analysed with IBM SPSS.
Results: PRP/WB exposure resulted in MCF-7 cell transformation from a polyhedral shape to a spindle-like morphology, and increased (p < 0.05) TGF-P1 mRNA and protein expression indicating induction of EMT and the adoption of a more aggressive phenotype. The generation of a pro-thrombotic microenvironment was noted, with MCF-7 cells inducing the formation of fibrin networks (PRP) and denser fibrin plaques (WB), indicating activation of the coagulation cascade.
Conclusion: Our results show that the reciprocal interaction between vascular components and tumour cells facilitates EMT and induces hypercoagulation, with implications for metastatic spread and thrombotic complications.
THE COMPARISON OF C-REACTIVE PROTEIN AND WHITE CELL COUNT IN HIV-POSITIVE AND HIVNEGATIVE PATIENTS WITH ACUTE APPENDICITIS
Truter-Nel M, Pienaar BH, Montwedi OD, Bekker P
Department of Surgery, University of Pretoria, Department of Biostatistics, University of Pretoria
Introduction: Acute appendicitis presents with a wide variety of signs and symptoms. Patients with the Human Immunodeficiency Virus (HIV) may present with atypical symptoms making it even more challenging to diagnose. Supportive tests, such as inflammatory markers, used as an adjunct in the diagnosis may be blunted in immunocompromised patients.
Objectives: To determine if there is a difference in HIVpositive and HIV-negative patients presenting with appendicitis clinically, regarding white cell count (WCC) and C-reactive protein (CRP) assays.
Methods: A prospective study was conducted at the University of Pretoria (UP) academic hospitals. 149 patients with acute appendicitis were divided into the groups as illustrated in the diagram according to HIV status and histology. CRP and WCC were compared between the different groups. Ethics approval was granted by UP.
Results: The mean CRP was markedly higher in HIV-positive patients compared to HIV-negative patients, 183 mg/l vs. 117 mg/l (p = 0.02). This higher trend was seen in all the appendicitis groups. With a cut-off of 25 mg/l, sensitivity and specificity of CRP in HIV-negative patients is 80% and 77%, and in HIV-positive patients is 84% and 50%, respectively. HIV-positive patients (mean 13 500 mm3) had a significantly lower WCC in all the appendicitis groups, compared to HIV-negative patients (mean 10 900 mm3) (p = 0.01). WCC (cutoff 12 000 mm3) had a sensitivity and specificity of 65% and 72% (HIV-negative) and 63% and 100% (HIV-positive).
Conclusion: CRP is a useful adjunct in the diagnosis of acute appendicitis. Despite a higher cut-off of 25 mg/l in our study, a sensitivity of 80% was still seen. An even higher sensitivity (84%) was seen in HIV-positive patients. WCC may not be as helpful with a sensitivity of only 65% in the HIV-positive group. Although the specificity of an elevated WCC in this study was 100% for the HIV-positive group, a normal WCC cannot exclude acute appendicitis.
VTE RISK AND PROPHYLAXIS PRESRIPTION IN SURGICAL PATIENTS AT A TERTIARY HOSPITAL IN THE EASTERN CAPE
WD Rocker1, TPage2, MRocher3, D Nel4
1-4Department of General Surgery, East London Hospital Complex
4Division of General Surgery, Groote Schuur Hospital and University of Cape Town
Introduction: Venous thromboembolism (VTE) is a common complication during and after hospitalisation and is deemed to be the commonest cause for preventable death in hospitalised patients. Despite its importance, there is little data on VTE risk and adherence to prophylaxis prescription guidelines in surgical patients from the South African public sector, especially from low resourced environments like the Eastern Cape Province.
Aim: The aim of this study was to evaluate the risk and prescription of VTE prophylaxis to surgical patients at a tertiary government hospital in the Eastern Cape.
Method: A cross sectional clinical audit of general surgical inpatients was performed on two separate dates in the months of July and August 2017. Patients' VTE risk was calculated by using the Caprini Risk Assessment Model (RAM) and their current thromboprophylaxis therapy compared to American College of Chest Physicians recommendations. The study was approved by the hospital ethics review board.
Results: 179 patients were included in the study, of which 56% were male and 44% were female. The average age was 45 (range 18-83). Of the total participants, 32% were elective and 68% were emergency admissions. With application of the RAM, 77% of patients were at risk for VTE (Caprini score of 2 and above), with 81% of elective and 74% of emergency admissions being at risk. Correct thromboprophylactic treatment according to risk factor profile was prescribed to 46% of patients, with 36% of elective admissions and 50% of emergency admissions receiving the correct therapy.
Conclusion: The rate of adequate thromboprophylaxis prescription for surgical inpatients at Frere hospital is very low, and is even lower for elective as compared to emergency cases. Interventions to improve the rate of adequate prophylaxis prescription need to be evaluated for feasibility and effect in this and other South African Hospitals.
REGIONAL AND SYSTEMIC CYTOKINE RESPONSE TO ACUTE APPENDICITIS IN HIV
Wheeler N1, Mokoena T1, Steel HC2
1Department of General Surgery, Steve Biko Academic Hospital
2Department of Immunology, University of Pretoria
Introduction: Acute appendicitis is a common surgical emergency and perforated appendicitis a leading cause of mortality and morbidity. In South Africa about 18% of the population is HIV positive with 25% deaths being HIV/ AIDS-related. HIV-positive patients have a four-fold increase in appendicitis. HIV-negative appendicitis patients have a peritoneal pro-inflammatory response, precipitating a systemic anti-inflammatory response, exaggerated in severe appendicitis. In contrast, HIV infection is characterised by a constant severe systemic pro-inflammatory response.
Aim(s): Investigate for differences in the pro- and antiinflammatory response in HIV-positive and -negative patients with the same surgical stage of acute appendicitis.
Methods: Prospective observational descriptive case-control study performed at Steve Biko Academic and Kalafong Hospitals. Approval obtained from the Human Ethics Committee of the Faculty of Health Sciences of the University of Pretoria.
Results: Complicated appendicitis found in 66% of low CD4 patients (50% perforated appendixes), despite similar symptoms duration in HIV-negative patients (p = 0.012). Complicated appendicitis found in 25% of HIV-negative patients (9,3% perforated appendixes). Low CD4 patients had a stronger systemic pro-inflammatory response and much weaker peritoneal pro-inflammatory response, compared to HIV negative patients. ICU (all low CD4) patients were shown to have an unmitigated systemic pro-inflammatory response compared to other low CD4 patients.
Conclusion: Patients with low CD4 counts have a poorer peritoneal immune response against infection compared to HIV-negative patients, resulting in fewer immune cells mobilising to the area of infection, with poor local control of infection and more patients with complicated appendicitis. Patients with low CD4 counts also have a stronger systemic pro-inflammatory response, resulting in physiologically sicker patients.
LOSS OF FUNCTION OF E2F1 MAY INDUCE PANCREATIC CANCER PROGRESSION
Nweke EN1, Ntwasa MN2, Brand MB3-5 Devar JD1,4 , Smith MD 1,4 Candy GP1
1Department of Surgery, University of Witwatersrand
2Department of Life and Consumer Sciences, University of South Africa, Johannesburg
3School of Physiology, Faculty of Health Sciences, University of Witwatersrand
4Chris Hani Baragwanath Hospital, Johannesburg
5Department of Surgery, Steve Biko Academic Hospital and the University of Pretoria
Background: E2F1 belongs to the E2F family of transcription factors that play crucial roles in cell cycle regulation, induction of tumour suppressor proteins and regulation of cellular proliferation. Pancreatic cancer (PDAC) studies have shown that overexpression of E2F1 during treatment is favourable. More knowledge on the expression of E2F1 in pancreatic tumours is crucial to better understanding its roles.
Aim: We sought to investigate novel mutations in PDAC that could drive the progression of pancreatic cancer.
Methods: Ethics clearance was obtained from the University of Witwatersrand ethics committee. For a pilot study we obtained four tissue samples and performed RNA sequencing. Afterwards, variant analysis was done using Ingenuity Variant Analysis tool and wANNOVAR. We excluded frequently observed mutations like in KRAS.
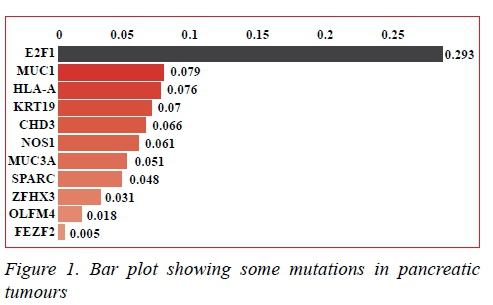
Results: We observed several mutations in pancreatic tumours including in E2F1 gene. These mutations included single nucleotide variations and non-frameshift substitutions occurring in the exonic region of the gene were predicted to result in loss of gene function.
Conclusion: The role of E2F1 in inducing cancer cell death has been observed. Loss of function of E2F1 due to mutations ensures that it does not perform its role. Future studies targeting these mutations may prove crucial for novel treatment strategies.
FACTORS AFFECTING BLOOD LOSS IN LIVER RESECTION FOR COLORECTAL CANCER LIVER METASTASES, WITH SPECIFIC REFERENCE TO MAJOR LIVER RESECTIONS
Potter MW, Kotze UK, Bernon MM, Burmeister S, Kloppers JC, Jonas E, Krige JEJ
Department of Surgery, University of Cape Town Health Sciences Faculty, Surgical Gastroenterology and HPB Unit, Groote Schuur Hospital, Observatory, Cape Town, South Africa
Introduction: Management of perioperative blood loss during resection of colorectal cancer liver metastasis (CRCLM) constitutes an important component of hepatic surgery.
Aim: This study assessed perioperative blood loss in patients undergoing hepatic resection for CRCLM in an academic centre, specifically evaluating major liver resections (MLR) and predictors of blood loss and blood transfusion requirements and their relationship with morbidity and mortality.
Method: All patients with CRCLM undergoing liver resection were identified from a prospective departmental database. Demographic data, operative management, mortality, morbidity and follow-up were analysed.
Results: Two hundred and sixteen patients (male/female 142/92), age (median, range 60, 18-81) underwent resection. MLR (> 3 segments) was required in 142 patients (5 segments n = 20, 4 n = 100, 3 n = 22) and minor resections (< 2 segments) in 74. Median operating time was 210 minutes (range: 90-465). Median blood loss was 550 mL (range: 50-3500). Intraoperative blood transfusion was required in 25 patients. Intermittent portal inflow occlusion was used in 118 patients (median duration 35.5 minutes, range 3-121). Median length of postoperative hospital stay was seven days (range 4-32). Major complications occurred in 28 (13.0%) patients. Six patients required re-operation (abscess n = 3, bile leak n = 1, small bowel obstruction n = 2). Nine patients (4.2%) died in hospital (multi-organ failure n = 2, liver failure n = 4, pulmonary embolus n = 2, pneumonia n = 1). Blood loss was significantly more in major liver resections. Analysing specific segment resections showed significantly higher blood loss in resections including segments 4a and 7. Blood loss was an independent predictor of postoperative complications.
Conclusion: Within the group of major resections the number of segments was not a significant predictor of major blood loss. However, the inclusion of S4a and 7 in a major resection was associated with significant more blood loss compared to the other segments. Blood loss was related to the risk for postoperative complications.
A RETROSPECTIVE ANALYSIS OF VIOLENCE AGAINST WOMEN PRESENTING AT AN URBAN LEVEL ONE TRAUMA CENTRE IN SOUTH AFRICA
Clift S1, Nelson RR1, McPherson D2, Edu S2, Nicol AJ2, Navsaria PH2, Morad H3, Sobnach S2
1University of Cape Town and
2Trauma Centre, Groote Schuur Hospital
3Division of General Surgery, Vancouver General Hospital and University of British Columbia
Introduction: Measuring violence against women (VAW) is difficult, and there is a paucity of research investigating VAW from the point of care. South African reports vary from rates of 35% to over 60%, exceeding global statistics.
Aim: To quantify the proportion of women presenting to Groote Schuur Hospital (GSH) Trauma Centre from 1 April 2016 to 1 March 2017 with intentional trauma.
Methods: A retrospective folder review was conducted on women attending GSH Trauma Centre for intentional trauma, between 1 April 2016 and 1 March 2017. Ethical approval was obtained.
Results: Of the 343 study participants, the mean age was 31.70 ± SD 11.33. The average delay in presentation was 1.47 days, and average hospital stay was 1.54 days. Most presented with blunt trauma (59.47%, n = 204), commonly due to bodily assault (39.36%, n = 135), assault with blunt objects (18.08%, n = 62) or stabbing (15.74%, n = 54). The commonest location of injury was the home (34.99%, n = 120). Assailants were often unknown (30.90%, n = 106). The commonest reason for assault was intoxication (13.70%, n = 47). Substance abuse (33.24%, n = 114) was common, as was HIV/AIDS (17.49%, n = 60) and chronic lifestyle diseases (14.58%, n = 50). Medical procedures included CT (54.81%, n = 188), analgesia (49.27%, n = 169) and X-rays (49.27%, n = 169). Twelve patients received blood transfusions (3.50%). 149 patients received surgical intervention, including sutures (23.32%, n = 80), washouts/debridement (6.12%, n = 21), and explorative laparotomies (4.08%, n = 14). The most frequent referral was to orthopaedics (7.00%, n = 24). Only 37 patients received social work intervention (10.79%). Discharge plans commonly included analgesia (65.72%), warning signs counselling (22.16%), and referral to local clinics (34.11%) or outpatient clinics (23.86%).
Conclusion/Recommendations: VAW remains common and under prioritised. Further research at primary or secondary institutions and healthcare worker training in history-taking and social work referral practices is recommended.
ELECTRICAL BURNS IN SOWETO CHILDREN: UNANTICIPATED CASUALTIES OF IMPROVISATION
Lack V, Estevez M, Loveland J, Westgarth-Taylor C
Department of Paediatric Surgery, Chris Hani Baragwanath Academic Hospital
Introduction: Worldwide electrical burns (EB) in children account for 2-6% of burns admissions. EB may be low voltage (LV) or high voltage (HV, including lightning strikes). At least 10% of the South African population live in informal dwellings with no amenities. As a result, access to electricity may be illegally improvised. This method of supply bypasses official infrastructure regulations and safety rules.
Aim(s): To describe the epidemiology, presentation and initial management of EB injuries experienced by children presenting to a single-centre Paediatric Burns Unit (PBU).
Methods: A retrospective review of files for children up to 10 years of age, admitted to the Paediatric Burns Unit with EB, between September 2013 and August 2016 was performed.
Human Research Ethics Committee (Medical) Clearance Certificate Number M160507.
Results: 103 cases of EB from a total of 1 449 burns admissions were identified. 91% were LV injuries with no mortalities, a male: female ratio of 3:1 and affected total body surface area (TBSA) of 0-15% (mean 2, 45%). 9% were HV injuries with six mortalities (65%), a male:female ratio of 8:1 and affected TBSA of 4%-76% (mean 36%). Mean age was 4.5 years with SD of 31 months. 56% came from areas with no formal household electrification. 81% of injuries were caused by outside wires and other illegal installations. There was a decreased frequency of injuries during winter noted in this series. 73% had biochemistry derangements, 4% electrocardiogram abnormalities, and 5% experienced haematuria. Length of stay ranged from 1-80 days (median of two days). 15% of the patients required various surgical interventions. There was no medical long-term follow-up after wound healing.
Conclusion/Recommendations: EB accounted for 7% of total burns admissions (higher than worldwide figures).
The epidemiology and presentation of these injuries is unique and poses a public health challenge. A long-term follow-up programme is required to further quantify the long-term effects of electrical burn injuries acquired in this paediatric population.
AN ANALYSIS OF PATIENT- AND DISEASE-RELATED FACTORS THAT PREDICT MORTALITY FROM BURNS IN PATIENTS AGED 60 YEARS AND OVER AT CHRIS HANI BARAGWANATH ACADEMIC HOSPITAL IN SOWETO, SOUTH AFRICA
Ede CJ1, Gemell R2, Manga J2
1University of Witwatersrand Surgical Department, Consultant in Burns Unit at CHBAH
2Medical interns
Background: Burns are a major cause of morbidity and mortality globally and in South Africa. The elderly are a vulnerable population, susceptible to burn injury.
Aim: The purpose of the study was to determine the outcome of burns patients (> 60 years old) admitted to the Chris Hani Baragwanath Academic Hospital (CHBAH) burns unit and to analyse the factors influencing these outcomes.
Methods: A retrospective analysis of elderly burn patients admitted to the CHBAH between 2011 and 2014 was conducted. Information was obtained from patient records using a data collection tool. Statistical analysis included univariate, multivariate and regression analysis.
Results: During the study period, 49 elderly burn patients were admitted with a mean age of 68.3 ± 7.8 years. The survival group exhibited a lower mean age (67.77 ± 7.39 years) compared to the demised group (69.71 ± 8.49 years) with a male to female ratio (25:24). There were a total of 22 deaths, mortality rate of 47% (22/49) of which (14/22, 63%) were female, however this was not statistically significant (p = 0.64). The mean percentage TBSA of burns was 13.35% and significantly impacted on mortality (p = 0.001) with a mean TBSA for the survivors (9.2%) and non-survivors (63.3%). Pre-existing comorbidities, female sex, presence of inhalation injuries and flame mechanism injuries were associated with an increased risk of mortality. The Baux score was not significant at predicting mortality (p = 0.08).
Conclusion: Our study indicated a high prevalence of mortality in the elderly population with a female predisposition. The significant factor predominantly influencing mortality in the study was TBSA.
A STUDY OF CHRISAL PROBIOTICS FOR MORE EFFICIENT CLEANING IN TYGERBERG BURNS UNIT AND AS A METHOD OF DECREASING NOSOCOMIAL INFECTIONS
Kleintjes WG1, Kotzee EP', Whitelaw A2, Abrahams A3, Ebrahim M1, Prag R1
1Department of Surgery, Western Cape Provincial Adult Burn Centre Unit;
2Department of Microbiology, Stellenbosch University
3Infection Prevention and Control - UCT
Introduction: Biofilm in hospital environments provides the ideal environment for pathogenic bacteria to thrive. Cleaning and disinfection does not affect bacteria 'hiding' in the biofilm. By using environmentally friendly probiotic bacteria to eliminate biofilm there may be reduced risk of hospital-acquired infection. A prospective controlled study was designed to investigate this.
Aim(s): The primary objective of the study was to determine whether probiotics can reduce hospital-acquired infections (HAIs) in the burns unit. The secondary objective was to establish a reduction and/or elimination of biofilm. The third objective was to determine the cost effectiveness and cost reductions.
Methods: The burn unit was divided into different areas and assigned a number to each test and comparative normal cleaning treatment zone in different rooms. We informed the cleaning staff to use only the probiotic products in each of the designated test areas. A baseline surface swab for culture was done in each area. Swabs were taken again weekly for culture. Ethical considerations: Stellenbosch University Health Research Ethics approval N17/04/045.
Results: The results indicate that probiotic cleansing in the hospital environment may be a cost-effective way of decreasing environmental biofilms and HAIs.
Conclusion/Recommendations: Based on the results further recommendations as to the application of probiotics are indicated, and a prospective study looking at the effects on wound cleaning is planned.
REVIEW OF UNPLANNED 30-DAY READMSSIONS OF GENERAL SURGERY PATIENTS AT WORCESTER HOSPITAL, WESTERN CAPE
Snyders P1, Swart O2, Duvenage R2
1Department of Surgery, Worcester Provincial Hospital
2Ukwanda Centre for Rural Health, Stellenbosch University
Introduction: Unplanned readmission within 30 days is currently being used in North America and Europe as a measure for quality of surgical care. Readmission rates vary in published hospital data with surgical site sepsis (SSI) and pain the most common causes. The correlation between readmission rates with mortality, increased patient volumes and complexity of surgery remain controversial.
Methods: Retrospective review of prospectively collected data of unplanned 30-day readmissions from January 2014 to December 2017 from the Department of General Surgery at Worcester Hospital, a regional hospital in the Western Cape, South Africa (Stellenbosch University HREC #N17/08/075).
Results: A total number of 9 378 patients were admitted to general surgery of whom 2.87% (270) were unplanned readmissions within 30 days. The mean age of this cohort was 44 years with 61% being male. Surgical-site infection 60.37% (163), gastrointestinal complications 24.44% (66) and blood transfusion required 7.03% (19) were the most common causes for readmission. Median initial length of stay (LOS) was four days and five on readmission. Readmissions were responsible for 1 914 added patient days costing R1.7 million in general surgical ward bed occupancy alone.
Conclusion: Worcester Hospital General Surgery had an unplanned readmission rate of 2.87% over a four-year period that correlates well with published studies. SSI was the most common reason. Using unplanned 30-day readmission rates as a quality of surgical care measure in the South African context needs further exploration.
PREVALENCE OF HELICOBACTER PYLORI AND THE INCIDENCE OF THE ASSOCIATED MALIGNANT AND PEPTIC ULCER DISEASE (PUD) AT NELSON MANDELA ACADEMIC HOSPITAL: A RETROSPECTIVE REVIEW
Molaoa SZ
Department of Surgery, WSU and Department of Health Sciences, UNISA
Background: H. pylori infection is associated with both benign and malignant gastrointestinal diseases. However, no studies have been conducted locally describing prevalence of H. pylori and its associated GIT diseases.
Objectives: The purpose of this study are to determine the prevalence of H. pylori, and the incidence of PUD and gastric malignancies among patients who are infected with H. pylori or who have stigmata of previous exposure to H. pylori.
Methods: Data was collected retrospectively from files of adult patients with upper GIT symptoms from January to December 2012. The gastric mucosal biopsy specimens were analysed for presence of H. pylori, chronic gastritis, PUD, and gastric malignancies.
Results: 156 records were analysed. There were 70 (45%) males and 86 (55%) females, with median age of 56.5.
The prevalence of H. pylori was 54.5%; 95% of 156 had chronic gastritis (CG). 97% of the 85 H. pylori positive and 93% of 71 H. pylori negative patients had CG. However, the difference was not statistically significant (97% vs. 93%, p = 0.322). The incidence of PUD was 16% and 10 (6.4%) had gastric malignancies, of which 4 (2.7%) and 3 (2%) were antral intestinal-type and proximal diffuse types, respectively. Three (2%) had gastric MALT lymphoma. The risk of both gastric malignancies and PUD was demonstrated to increase with advancing age.
Conclusion: The prevalence of H. pylori was equivalent to the global prevalence; however, high prevalence of CG may be indicative of high local infection rate. The incidence of H. pylori and/or chronic gastritis-associated intestinal-type gastric adenocarcinoma, MALT lymphoma and PUD is equivalent to that reported globally. Advancing age and active H. pylori infection or stigmata of past exposure thereto are associated with increased risk of peptic ulcers and malignant gastric diseases. A prospective study to define the group of H. pylori-positive patients or with stigmata thereof who are at increased risk of H. pylori-associated adenocarcinoma may need to be conducted in order to devise surveillance strategies aimed at early detection of gastric cancer, and therefore timely curative intervention.
A RETROSPECTIVE STUDY ON CLINICAL OUTCOMES OF PERFORATED PEPTIC ULCER PATIENTS IN A TERTIARY HOSPITAL OVER A PERIOD OF FIVE YEARS
Malefahlo MT
Department of Surgery, Steve Biko Academic Hospital
Background: Perforated peptic ulcer (PPU) is associated with high morbidity and mortality. This study looks at the described prognostic scores in PPU and evaluates the clinical outcome of patients in this setting. This could help identify areas that need improvement in our system.
Aim: To determine the clinical outcome of PPU patients up to 30 days postoperatively.
Method: A retrospective, cohort study. This study was approved by the Ethics committee.
Results: A final sample of 117 patients evaluated. Most patients (63%) had no comorbidities. The more the comorbidities, the poorer the prognosis. Most patients (65%) presented between day one to five of onset of pain, and 19% presented within 24 hours. The overall morbidity and mortality was 18% and 4.2% respectively. The study also found that patients wait very long to be evaluated by the surgeon and to be operated. Three different prognostic scores were used, Boey, ASA and MPI, and found the MPI score to be more reliable with a p-value of 0.00. Most of the patients (74%) did not need critical care. Of those who did, 6.6% were resuscitated in critical care before surgery and survived. Eighteen percent were admitted post-surgery. All the patients that died were in the group admitted postoperatively to critical care unit. Average length of hospital stay was six days. The outpatient follow up was 72%.
Conclusion: PPU management can be challenging in the setting where critical care and theatre availability is poor. Patients also present late. Mortality rate is still acceptable but morbidity is high. The MPI score in our setting seems reliable and we propose its incorporation for routine use into patients' assessment.
THE OUTCOME OF THE USE OF INTERCOSTAL DRAIN IN DR GEORGE MUKHARI ACADEMIC HOSPITAL
Okeke IC, Koto MZ
Department of Surgery, Sefako Makgatho Health Sciences University
Background: In clinical practice, the use of intercostal drain deployed as a lifesaving procedure cannot be overemphasised, however lingering concern has been on the preventable complications which are associated with its insertion or removal. This retrospective study looked at the experience at George Mukhari Academic Hospital at Pretoria North, South Africa.
Aim(s): To determine the incidence of complications encountered by the insertion and removal of the intercostal drain. Secondly, if post-intercostal drain removal chest x-ray exposure can be avoided.
Methods: A retrospective study at George Mukhari Academic Hospital, South Africa for a period of two years. All disciplines in which intercostal drains are used were included. Approximately 500 patients constituted the study population. Sample size of 174 of a two-sided 95% confidence interval of ± 5% drawn systematically from the study population and inclusion criterion are all patients in whom intercostal drain had been inserted during the specified period and exclusion criteria were missing files, poor documentation or inadequate clinical information that does not sufficiently answer the question in the data collection sheet.
Results: A total of 174 cases of admission in whom intercostal drain was used of which male patients were twice the number of females [118 (67.8%) to 56 (32,2%)], with an average age of 38 years. Trauma made up half of the cases (50.6%) as a singular indication for its use. Complications at ICD insertion observed was 5% and related more to tube placement. Recurrent pneumothorax following removal had 4% incidence rate. All patients with recurrent pneumothorax or other post ICD removal complications in the study (residual haemothorax 4% and residual pneumohaemothorax 1 (0.6%) had no further interventions and were subsequently discharged. With the 4% incidence rate found in the study for recurrent pneumothorax post ICD removal, the relevance of post-removal chest x-ray is in question.
Conclusion: Lower incidence of complication observed at the insertion of ICD may be directly related to the experience and skill and ATLS-certified medical personnel involved.
Recurrent pneumothorax incidence is significantly low, the question of the relevance of post ICD chest x-ray film exposure is questionable and can be best answered by a prospective study.
HEAD INJURY OUTCOMES IN A SINGLE TRAUMA UNIT CENTRE OVER A SIX-YEAR PERIOD: ARE WE COPING?
Moeng MS, Goosen JG
University of the Witwatersrand
Introduction: Neurosurgical facilities remain limited for our South African population. Efficient diagnosis and CT scanning in relevant cases is essential for appropriate referral to resourced units for further management. The rehabilitation burden remains an ongoing challenge and requires constant reassessment.
Aim: Evaluate the outcomes and distribution patterns of head injuries presenting to a single trauma facility in Johannesburg.
Method: Retrospective analysis of the Priority 1 (P1) head injuries seen and treated at CMJAH over a period of six years. The mechanism of injury, demographic data, injury patterns, GCS, disposition from emergency department, discharge status, in-hospital mortality were all recorded and analysed. The Trauma Bank data was used to complement the clinical notes.
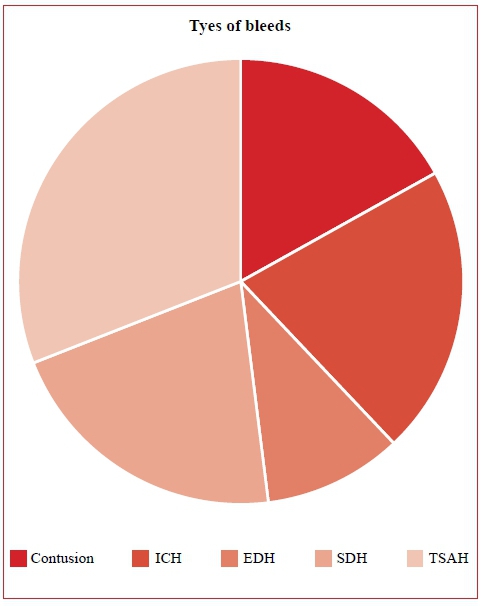
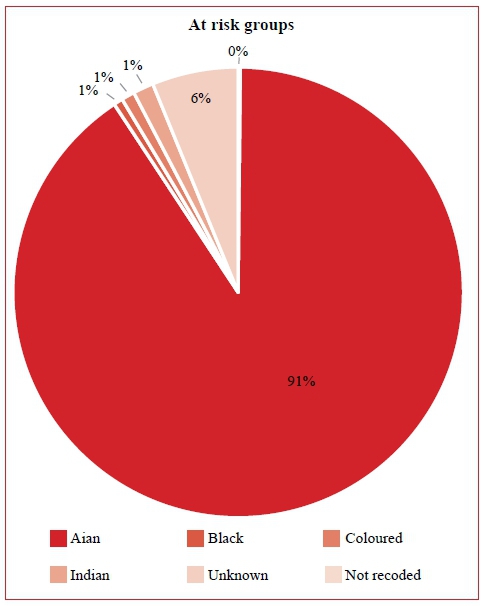
Findings: Of the 3 055 head injuries treated in the study period, 91% of which were African. Male constituted 87, 43% of the study group. The 18-45-year age group was the most predominant. Blunt trauma was responsible in 82% of the mechanisms, with PVC accounting for most injuries. Of the intracranial bleeds, TSAH occurred in 31% of the bleeds, followed by an equal number (21%) of intracerebrals and the subdural bleeds. The in-hospital mortality was high, with one in five of the patients not making it to discharge. Minor injuries did well overall and were discharged home in a good functional state.
Conclusion: The head injury load to the Johannesburg Trauma Unit was significant in the study period. The African black male remains at high risk of sustaining head injuries. Mortality remains high in these head injuries. More effort should be made to educate the community about the impact of head injuries in society. More facilities and neurosurgical facilities are required for better service.
THE CORRELATION OF CT SCAN IN THE MANAGEMENT OF PATIENTS WITH PENETRATING ABDOMINAL INJURIES
Patel S
Sefako Makgatho Health Sciences University
Introduction: Penetrating abdominal trauma contributes significantly to the burden of disease in South Africa. The role of imaging, particularly CT scan in this subset of patients has yet to be established. In this study we reviewed patients with penetrating abdominal injuries and correlated the imaging and intraoperative findings.
Methods: Over an 18-month period (June 2015 to January 2017), patient records of all patients presenting with penetrating abdominal trauma were reviewed. Patients presenting with haemodynamic instability and peritonitis were excluded from the study and immediately underwent laparatomy. Patients presenting with penetrating abdominal trauma and who were haemodynamically stable and not peritonitic, had imaging done in the form of a CT scan. The CT scan findings were then correlated with the intraoperative findings.
Results: One hundred and thirty-one patients with penetrating abdominal trauma were eligible for imaging. Fifty-two patients had positive CT scan findings as well as positive intraoperative findings. Seventy-nine (60%) had negative findings on CT scan. Off the seventy-nine patients, fifty-nine (74%) had negative imaging findings as well as negative intraoperative findings. Twenty (25%) had negative CT findings but positive intraoperative findings.
Conclusion: CT scan correlates poorly with intraoperative findings and thus is a poor modality for screening patients.
THE ROLE OF A REPEATED ABDOMINAL SONOGRAPHY IN BLUNT INJURY
Israelit SH, Monzon B, Goosen J, Moeng MS
Trauma Unit, Charlotte Maxeke Johannesburg Academic Hospital and Wits University
Introduction: FAST may enhance clinical examination of stable blunt trauma patients.
Aim: Investigate the accuracy for repeated-delayed FAST, in the subgroup of stable blunt trauma victims, with primary normal FAST.
Methods: Retrospective review of prospectively inserted data (Feb 2005 - Feb 2009) of 482 patients, who sustained fall from height. Data collected: demographics, GCS, HR, RR, SBP, RTS, AIS, and FAST, repeated-FAST, CT scans and diagnosed injuries.
Results: N = 156 stable patients with GCS 15. Mean age 30 years. Average admission HR, SBP and RR, were 81-b/ min, 127 mmHg and 20-/min respectively. Average RTSc and AIS were seven and five respectively. Ninety patients underwent FAST during resuscitation, 80 patients had a negative FAST. Ten patients with positive FAST underwent a CT scan (negative for 2 patients). Nine patients underwent repeated-FAST within 4-6 hours (8 negative) - no further investigation. One patient with positive repeat-FAST had grade-II liver laceration on CT scan. Predictive parameters for repeat FAST: Sensitivity = 78%, Specificity = 99%, PPV = 88%, NPV = 98%, Overall Accuracy = 97%.
Conclusions: FAST is a reliable screening tool for stable blunt injury. Negative repeat FAST is sufficient to rule out significant abdominal injury.
AN ANALYSIS OF AIR-CRASH INJURY PATTERNS
Pswarayi R, Moeng MS
University of the Witwatersrand
Introduction: Aviation crashes are usually fatal with few patients surviving to hospital. The description of aviation-related injuries is scarce and therefore poorly understood. This study aims to analyse the patterns of injury identified on patient-victims of air crash/aviation crash coming into a Level 1 Trauma facility. In particular, the distribution of injury and the severity grading of the injuries.
AIM: Describe the injury patterns and outcomes of subjects involved in air crash incidents who presented at a Level Trauma unit over a period of six years
Method: Retrospective data analysis of Trauma Medibank information form 01 Jan 2011 till 31 December 2017 at Level 1 Trauma Centre. The following data was collected and analysed: demographics, injuries sustained, injury severity score, surgical interventions carried out, length of stay in ICU, ventilation days, hospital length of stay, associated morbidity, 28 day mortality, outcome (discharge, death).
Findings: Twenty-two patients were recruited for the study, majority of whom were male. Average age was 43,7 years (ranging from 12-67), RTS was 5.3 (4, 1-7, 8), with average ISS 14, 7 (3-47), and NISS of 16 (3-43). Helicopter crashes were noted in 31, 8% of the cases and fixed wing crashes in 54, and 5% of cases. Muscular-skeletal injuries were the most common followed by chest injuries. Combination of injuries was very common, including spinal injuries. There were at least two burn injuries in the group. Orthopaedic surgical interventions were the most common procedures required in the study group. The mortality in the overall group was low with most of the candidates being able to be discharged home in an excellent condition.
Conclusion: Musculoskeletal injuries were the most common injuries noted. Combination of multiple injuries was not infrequent. Subjects that are well enough to make it to hospital from the crashes, have a reasonable prognosis.
WHICH TRAUMA PATIENTS ARE AT RISK OF INHOSPITAL MORTALITY AT A JOHANNESBURG TRAUMA UNIT: EIGHT-YEAR REVIEW
Pswarayi RM, Joubert IM, Goosen J, Moeng MS
Johannesburg Trauma Unit, Charlotte Maxeke Hospital and University of the Witwatersrand
Background: Trauma remains pandemic in South Africa together with the challenges of chronic illness, malnutrition and poverty. Society tends to only pay attention to the impact of mortality around major holidays with very few successful sustainable interventions instituted. TRISS methodology is the standard method used to evaluate the mortality outcomes in trauma. An in-depth review of the overall trauma mortality is essential for quality control and maintenance of clinical standards.
Aim: Analyse the in-hospital mortality distribution at the Johannesburg Trauma Unit over a sustained period.
Method: Retrospective study of the Trauma Bank data at CMJAH from 01 Jan 2005 till 31 Dec 2012. The data was correlated with the mortality and the MNM data. Demographics, mechanism of injury, ISS, NISS, ISS and NISS based probability of survival, in-hospital mortality were all analysed. Statistical analysis was done, and the p value of < 0.05 was considered significant.
Results: 18 087 trauma P1 subjects were entered in the study period, most of whom were male. The 21-45 age group was the most affected. The worst average ISS was noted in the burns group, while the worst NISS was seen in the motor bike and the blunt assault groups.
The overall mortality was 1 496 (8,27%) over the study period, with the worst mortality seen in burns group (22.56%) followed by pedestrian vehicle accident group at 15,99%. But the worst average probability of survival in those who died (1 496) was seen in both the motor vehicle and the motorbike groups, at ISS POS of 44% and NISS POS 34%.
Conclusion: Burns patients had the highest ISS and the highest mortality in our study group. The pedestrian vehicle collision group was the next highest mortality, even though they did not have the lowest NISS or ISS probability of survival scores. Concerted effort is required to target these groups and improve their mortality to relate to the overall mortality of 8,27%.
ORTHOPAEDIC SURGEON DENSITY IN SOUTH AFRICA
DellAJ1, Gray S2, Fraser R3, Held M4, Dunn R4
1Department of Surgery, University of Cape Town Health Sciences Faculty, Groote Schuur Hospital
2Medical Intern, Groote Schuur Hospital
3Busamed Private Hospital, Hillcrest, Durban
4Orthopaedic Research Unit, Division of Orthopaedic Surgery, University of Cape Town, Groote Schuur Hospital
Introduction: In the era of global surgery, there is limited data regarding the available surgical workforce in South Africa.
Aim: The aim of this study was to determine the orthopaedic surgeon density in South Africa.
Methods: This involved a quantitative descriptive analysis of all registered specialist orthopaedic surgeons in South Africa, using data collected from various professional societal national databases. This research was approved by the Human Research and Ethics Committee at the University of Cape Town (HREC 545/2017) and the Departmental Research Council for the Department of Surgery (2017/069).
Results: The results showed 1.63 orthopaedic surgeons per 100 000 population. The vast majority were male (95%) with under two-thirds (65%) being under the age of 55 years. The majority of the orthopaedic surgeons were found in Gauteng, followed by the Western Cape and KwaZulu-Natal. The majority of specialists reportedly worked either full or parttime in the private sector (95%) and the orthopaedic surgeon density per uninsured population (0.36) was far below that of the private sector (8.3).
Conclusion: Interprovincial differences as well as intersectoral differences were marked indicating geographic and socioeconomic maldistribution of orthopaedic surgeons. This parallels previous studies which looked at other surgical sub-disciplines in South Africa. Addressing this maldistribution requires concerted efforts to expand public sector specialist posts as well as quantifying the burden of orthopaedic disease in both private and public sectors before recommendations can be made regarding workforce allocation in the future.
LUNG HYDATIC CYST IN CHILDREN - OUR EXPERIENCE AT NELSON MANDELA ACADEMIC HOSPITAL
Delgado AL1, Loko EM2
1Walter Sisulu University/Nelson Mandela Academic Hospital, Department of Surgery
2elson Mandela Academic Hospital, Department of Surgery
Background: Hydatid infestation of the lung can be primary or secondary. Cystic echinococcosis is regarded as endemic in sub-Saharan Africa. Available evidence suggests that several strains within the Echinococcosis granulosis group are prevalent in sub-Saharan Africa. However, for most countries only scarce data, if any, exist.
Method: We did a retrospective study of all children suffering from lung hydatid cyst admitted in our paediatric surgery ward, from September 2015 to September 2017; we studied 11 children, collected and analysed different variables such as: age, gender, lung affected, unilateral or bilateral cyst, size of the cysts, treatment and complications; we created tables for statistical study.
Results: From those 11 children suffering from lung hydatic cysts, eight were female and three male; the group of ages more affected was that from six to ten years with five patients (45.5%), followed by the groups of five to six years and more than ten years with three children 27,2 each. The left lung was the most affected in six patients by 54, 5%, the right lung and bilateral lungs were affected only in three patients each 27%.
The surgical treatment, PAIR (punction - aspiration - injection and re-aspiration) was performed in eight children (72.7%). The broncho pleural fistula as a complication accounted for seven patients and a cyst rupture in only one child. We did not have death in our group of patients.
Conclusions: Lung hydatid cysts in our patients were observed more frequently in the left side. The surgical treatment performed was PAIR mostly in cysts more than 6 cm or with complications. Conservative treatment is an option in some cases.
SUPRACONDYLAR FRACTURE OF THE HUMERUS IN CHILDREN: FIXATION WITH TWO PARALLEL KIRSCHNER WIRES
Adu-Parko LI
Walter Sisulu University, Mthatha
Objective: To analyse and present the surgical results from unstable supracondylar fractures of the humerus in children treated by means of reduction and percutaneous fixation using two parallel Kirschner wires and open reduction of the fractures if the closed reduction failed.
Methods: A study was conducted on 65 children, taking into consideration gender, age at the time of the assessment, side affected, type and mechanism of trauma, postoperative complications and radiographic and clinic variables.
Results: Forty-seven were observed in the right arm and sixteen in the left arm. The age at the time of the fracture ranged from two to twelve years. Seven fractures were classified as type II and fifty-eight as type III. Type II were done closed reduction and percutaneous pinning and type III done open reduction and two parallel pins. Forty-one patients were male and twenty-four were female. The length of follow-up ranged from three weeks up to a year. Baumann's angle ranged from 69-100 (mean 78.3). According to the modified Flynn's criteria 65 cases represented with satisfactory outcomes: 55 excellent (85 %), seven good (10 %), and three fair (5 %).
Conclusion: Fixation of supracondylar fractures in children by two parallel Kirschner wires either by closed reduction and percutaneous pinning or open reduction and internal fixation leads to good results.
VEIN SIZE AND DEMOGRAPHICS - IS THERE A CORRELATION?
Roberts N, Pearce NE
Department of Surgery, University of the Free State
Background: In revascularisation of patients with limb-threatening ischaemia, the preferred conduit for an open infra-inguinal bypass is the greater saphenous vein (GSV), which provides the best long-term patency, is usually available in the desired length, and can be harvested swiftly. Many factors have been associated with primary graft failure, in particular the size of the conduit graft.
Aim: Our aim in this study was to demonstrate a relationship between average vein size and demographic variables like race, age and gender. Ethics approval was obtained. The study was done retrospectively, using data over the previous 10 years from January 2006 to December 2015 in patients who underwent vein mapping with ultrasound preoperatively prior to a lower limb bypass procedure in Universitas Academic Hospital. Patient demographics were found on the hospital's electronic data system.
Results: The total number of patients were 907, but two were excluded due to illegibility, one patient was below the age of 18 years and 59 patients had more than one vein mapping done on the same limb. In total, we included 845 patients and the meteorological season was used as a surrogate indicating the average temperature in the vascular suite.
Conclusion: Owing to the existing risk of small conduit size for graft failure, the results may be used to improve selection of patients suitable for surgery on demographic parameters and therefore aim to improve outcomes of revascularisation procedures and decrease complications associated with graft failure.
AN AUDIT OF LAPAROSCOPIC COLORECTAL PROCEDURES DONE AT DR GEORGE MUKHARI ACADEMIC HOSPITAL: OUR INITIAL EXPERIENCE
Molefe ED, Koto MZ
Department of Surgery, Sefako Makgatho Health Sciences University
Background: Challenges of setting up laparoscopic colorectal services in a public hospital are huge, and in this study we report our initial experience in laparoscopic surgery done at Dr George Mukhari Hospital from November 2011 to May 2017.
Methods: A total of 60 patients who had undergone laparoscopic colorectal procedures from November 2017 to May 2017 were enrolled in the study. Data was collected from theatre operation lists, files of patients from Dr George Mukhari hospital archives and Sefako Makgatho University department of surgery database using data collecting sheets. Data captured was analysed using descriptive and inferential statistics. All statistical procedures were performed on SAS, Release 9.2, running under Microsoft windows.
Results: The majority of laparoscopic procedures done were Hartmann closure - 21 (35%) [281 min], followed by right hemicolectomy - 10 (16.67%) [260 min], sigmoidectomy -10 (16.67%) [152 min], abdominoperineal resection plus TME - 4 (6.67%) [441 min], low anterior resection - 2 (3.33%) [415 min], subtotal colectomy - 3 (5%) [441 min], rectopexy - 2 (3.33%) [296 min], diverting colostomy - 4 (6.67%) [87], exploration plus biopsy - 1 (1.67%) [230 min], colpocystocoele repair - 1 (1.67%) [385 min], left hemicolectomy - 1 (1.67%) [247 min], and ileotransverse bypass - 1 (1.67%) [247 min]. The conversion rate was 10% due to difficult mobilisation of the colon, tumour spread or enterotomy. Sixteen patients had complications. Four mortalities were reported, one mortality due to anastomotic leak and stroke, one due to pulmonary embolism and two due to advanced colon cancer. Previous stoma site wound sepsis accounted for five patients, surgical site sepsis for four patients, hypokalaemia for one patient, renal failure for one patient, and postoperative diarrhoea for one patient. Twenty-five patients with missing files were excluded from the study. Return of bowel movements was measured clinically. Based on the results, return of bowel movements was day one in most cases (57.14%), day two - 25.71% and day three -17.14%. The hospital stay was variable, ranging from three to 62 days depending on the postoperative complications. The longest hospital stay was 62 days which ended in mortality and the shortest was three days.
Conclusion: The above results reflect the feasibility of laparoscopic surgery for benign and malignant conditions in adult age group and any gender. The conversion rate from laparoscopic to open was lower with low mortality and complication rate. Our study reflected early return of gut motility and low hospital stay. We highly recommend minimal invasive surgical approach to benign and malignant colorectal procedures where feasible.
INCREASED PREVALENCE OF SYSTEMIC INFLAMMATORY DISEASE IN CAROTID STENOSIS WITH TRENDING INCREASE OF POSTOPERATIVE COMPLICATIONS AND STROKE
Shalaby SY1,2, Dardik A2
1Department of Surgery, Witwatersrand University
2Department of Surgery, Yale University
Introduction: Carotid endartectomy (CEA) has an inflammatory pathogenesis and is associated with inflammatory diseases (autoimmune, autoinflammatory, or allegeric diseases) such as metabolic syndrome.
Aim: We hypothesised that a history of systemic inflammatory disease (SID) is associated with carotid stenosis and examined the prevalence of SID in patients with carotid stenosis undergone CEA.
Methods: Medical record review of all CEA patients 2002-2013. SID determined by diagnosis and/or treatment. Ultrasound of peak systolic velocity (PSV) recorded at last follow-up visit.
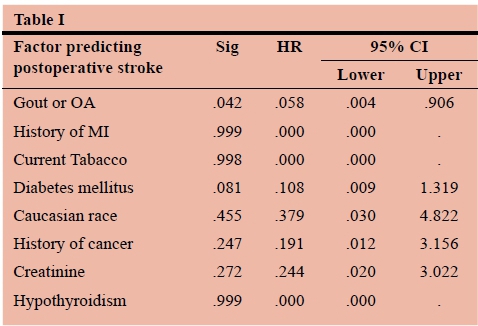
Results: Fifty-seven of 79 (72%) patients undergoing CEA had an AID, most commonly osteoarthritis (34%) or gout (15%). There were no significant baseline differences between patients without or with SID other than a trending significance of past history myocardial infarction in patients with an SID (10.5% vs. 0%; p = 0.11); there was no difference between PSV (426.7 ± 20.2 vs. 381.2 ± 31.9 cm/sec; p = 0.23) or preoperative incidence of stroke (10.5% vs. 13.6%; p = 0.69). There was no difference in perioperative complications (12.3% vs. 4.5%; p = 0.31). Duration of follow-up did not differ between the two groups (4.4 ± 0.3 vs. 4.4 ± 0.5 years; p = 0.55). Postoperative stroke was trending in patients with SID 10.5% vs. 0%; p = 0.11). Postoperative PSV on follow-up was significantly lower in patients with SID (114.5 ± 71.3 vs. 183.5 cm/sec; p = 0.01). Logistic Regression Analysis of gout or OA predicting lower risk of stroke after CEA (HR 0.06; p = 0.042) (Table I).
Conclusion: Patients with severe carotid stenosis undergoing CEA have a high prevalence of SID, trending increased comorbidities, and trending increased rates of postoperative stroke. Larger sample size is required for confirmation of results. Patients with carotid stenosis needing CEA may be a high-risk group requiring increased perioperative and postoperative resources.
OUR INITIAL EXPERIENCE IN MINIMALLY INVASIVE PANCREATIC SURGERY
Kumar N, Sardiwalla II, Balabyeki MA, Koto MZ
Department of General Surgery, Sefako Makgatho Health Sciences University
Introduction: Pancreatic procedures are formidable challenges undertaken by surgeons. An increase in the minimally invasive approach has added a new dimension to these challenging procedures. There is an increasing acceptance for a minimally invasive approach owing to the benefits conferred by this approach and the equivalent oncological results.
Aims: Review of institutional experience with minimally invasive pancreatic surgery.
Methods: The study is a retrospective review of all cases of pancreatic surgery performed laparoscopically at Dr George Mukhari Academic Hospital (DGMAH). Data was collected prospectively on a predesigned proforma and stored on a departmental database. Procedures included were laparoscopic pancreaticoduodenectomy (Whipple procedure), laparoscopic double bypass (gastrojejenostomy and hepaticojejenostomy) and laparoscopic distal pancreatectomy (with splenectomy). All incomplete records were excluded. Cases performed between January 2018 to May 2018 were collected. Data collected included patient demographics, indications for procedures, types of procedure performed, time from presentation to diagnosis, time from diagnosis to surgery, total duration of hospital stay, total stay in ICU, operative time and postoperative complications. Ethical considerations: ethics approved.
Results: A total of 10 minimally invasive pancreatic surgeries were performed between January 2018 to May 2018 at DGMAH. The procedures included three laparoscopic Whipple procedures, three distal pancreatectomy procedures and four double bypass procedures. Indications were resectable and irresectable pancreatic adenocarcinoma, solid pseudopapillary tumour of the tail of the pancreas and pancreatic fracture as a result of trauma (Grade III blunt pancreatic injury). The average duration of hospital stay for the laparoscopic Whipple procedure was 10 days, for the double bypass was seven days and for the distal pancreatectomy was five days. Average operating times for the Whipple procedure was eight to ten hours, for the double bypass was four to five hours and for the distal pancreatectomy was three to four hours.
Postoperative complications included: one case of collections (double bypass group); one case of wound sepsis (Whipple group); one mortality (Whipple group) due to cardiac tamponade.
Conclusion: Laparoscopic approach to pancreatic surgery is a challenging surgical skill. Our initial experience has highlighted this steep learning curve.
HYPERCOAGULABILITY USING BIOPHYSICAL PARAMETERS IN HIV-POSITIVE VERSUS HIV-NEGATIVE PATIENTS WITH DEEP VEIN THROMBOSIS
Jackson BS1, Pretorius E2, Mokoena T3
1Department of Surgery, Kalafong Tertiary Hospital, University of Pretoria
2Physiological Sciences, Stellenbosch University
3Department of Surgery, Steve Biko Academic Hospital, University of Pretoria
Introduction: Patients infected with the human immunodeficiency virus (HIV) are more prone to developing a hypercoagulable state. This may be due to an upregulated inflammatory system resulting in a different coagulation profile.
Aim(s): To compare the coagulation profile of HIV-positive patients to HIV-negative patients.
Methods: A descriptive comparative prospective study recruiting symptomatic confirmed deep vein thrombosis (DVT) adult patients with HIV status. There were three groups (controls, HIV-negative, and HIV-positive) analysed with a thromboelastogram, light microscopy smears and the scanning electron microscope. Approval by University of Pretoria ethics committee.
Results: DVT patients have a hypercoagulable viscoelastic profile but no significant difference between HIV-positive and HIV-negative groups. The light microscopy demonstrated red blood cell changes in the DVT groups, which were more extreme in the HIV-positive group. These findings were confirmed and more pronounced when examining the ultrastructure of red blood cells. Morphological changes were also seen in platelets and the fibrin network.
Conclusion/Recommendations: The ultrastructural changes of the red blood cell, platelets and fibrin fibre network indicate that there are specific differences in patients infected with HIV. HIV-positive patients do have a different coagulation profile compared to HIV-negative patients which can result in hypercoagulability and DVT.
USE OF COLONIC STENTS AT DR GEORGE MUKHARI ACADEMIC HOSPITAL (DGMAH)
Kumar N, Sardiwalla II, Balabyeki MA, Koto MZ
Department of General Surgery, Sefako Makgatho Health Sciences University
Introduction: Colonic stents have traditionally been used to stent obstructing left-sided colonic tumours. Unique in their flexible nature, their use has also been expanded to stent duodenal masses. A few case reports have also been published about the use of colonic stents to facilitate surgery for right-sided tumours.
Aim(s): Review of the use of colonic stents at DGMAH.
Methods: The study is a retrospective review of all cases of the use of colonic stents at DGMAH. A prospectively maintained database, Olympus Endobase®, is used in the endoscopy suite and was used to collect the data. All cases that used colonic stents between January 2018 to May 2018, were included. All incomplete records were excluded. Data was collected on a proforma data collection sheet and included details on patient demographics, tumour location, any complications from the procedure, success of the procedure as well as subsequent surgical intervention.
Ethical considerations: Ethics approved.
Results: A total of 35 colonic stents were attempted during the study period. Twenty-five stents were used for colonic pathology and 10 for duodenal pathology. For colonic stenting, 20 were performed for palliation of advanced cancer and five for temporary purposes as a bridge to subsequent surgical intervention. Of the five colonic stents placed for temporary purposes, four patients received left-sided stents and subsequently received laparoscopic left hemicolectomy, while one patient had a right-sided stent placed and subsequently received a laparoscopic subtotal colectomy (with en-block cholecystecetomy). There were no stomas and no complications in the operated patients. The 10 duodenal stents were placed for palliation of advanced cancer with associated gastric outlet obstruction. There was 100% success rate in all cases where the stent was attempted.
Conclusion/Recommendations: Colonic stents are a versatile tool that play an important role in palliative management of advanced malignancy. They are also useful in bridging to surgery and facilitating laparoscopic surgery as well as decreasing stoma rates on the left.
LONG-TERM OUTCOME OF CATHETER-DIRECTED THROMBOLYSIS FOR ILIOFEMORAL DEEP VENOUS THROMBOSIS
Rampai T, Mulaudzi TV, Tsotetsi S, Sikhosana M
Department of Surgery, Unit of Vascular and Endovascular Surgery, Steve Biko Academic Hospital, University of Pretoria
Introduction: Post-thrombotic syndrome (PTS) is a chronic complication of proximal deep vein thrombosis (DVT). More than 50% of patients managed with anticoagulation alone will have significant symptoms. PTS results in significant disability and impaired quality of life. The goal of the study is to assess the long-term outcome of patients who had been managed with catheter-directed thrombolysis for iliofemoral deep venous thrombosis
Aim(s): To assess incidence and the severity of post-thrombotic syndrome after catheter directed thrombolysis and to assess iliac veins patency.
Methods: A retrospective cohort study of patients who were managed with CDT for iliofemoral DVT for the last 11 years. These patients are assessed clinically and had a venous duplex performed. Ethics Reference No: 529/2017 University of Pretoria.
Results: A total of 23 patients were managed with catheter-directed or pharmacomechanical thrombolysis. Predominantly female 19 (82.6%), mean age 34.4 years. Sixteen (69.6%) had left ileofemoral DVT, only two (8.7%) had thrombus extension into the IVC. CDT used on 16 (69.6%), angiojet, angioplasty and stenting (30.4%, 52.1% and 8.70% respectively). Eight patients died, one in hospital from intracranial bleeding; the other deaths were not related to DVT. On ultrasound seven (30.4%) had no residual thrombus and 16 (69.5%) had residual thrombus. Seven (30.5%) developed PTS, of which three (13.0%) moderate and four (17.3%) severe.
Conclusion/Recommendations: It would appear from this study that CDT does reduce the incidence and severity of PTS.
OUTCOMES OF LAPAROSCOPIC HARTMANN'S PROCEDURE REVERSALS AT THE DR GEORGE MUKHARI ACADEMIC HOSPITAL
Ngema SS1, Ghoor F2
1General Surgery Registrar
2Head of Colorectal Unit, Sefako Makgatho Health Sciences University
Introduction: Restoration of bowel continuity post Hartmann's procedure is a major surgical procedure which typically requires a laparotomy. It is associated with significant morbidity and potential mortality.
Aim: Review our experience with laparoscopic Hartmann's procedure reversals.
Methods: We retrospectively reviewed the medical records of patients who had undergone laparoscopic Hartmann's procedure reversal between July 2014 and March 2018.
Results: Twelve patients were identified. The cases were performed by consultants or registrars under consultant supervision. The average age of the patients was 48 years (range 26 to 78) with a 1:1 male to female ratio. The indications for the Hartmann's procedure were predominantly sigmoid volvulus (50%), followed by trauma (33.3%), sigmoid tumour (8.3%) and diverticular perforation (8.3%). The laparoscopic approach was successful in 11 of the 12 patients (conversion rate of 8.3%). The reason for conversion was extensive adhesions. The mean operative time was 288 minutes. Three (25%) patients sustained enterotomies of which two were detected intraoperatively and repaired. The third patient with an enterotomy was picked up on a relook laparotomy and ended up with an ileostomy which was later reversed. This constituted the only re-operation case (rate 8.3%). The rate of surgical site infection was 25%. The average length of hospital stay was 12.9 days (range 5 to 61 days). Full feeds were commenced on an average 2.28 days. There were no anastomotic leaks, re-admissions and no mortality.
Conclusion: Hartmann's procedure reversals can be performed laparoscopically with reasonable safety. The added advantage for surgical trainees is the enhancement of the laparoscopic skills of adhesiolysis, mobilisation of the left colon including the splenic flexure and the use of a circular stapler.
PRESENTATION OF MULTINODULAR GOITRE AFTER UNIVERSAL IODINATION OF TABLE SALT: THE CHRIS HANI BARAGWANATH ACADEMIC HOSPITAL EXPERIENCE
Luvhengo T1,3,5, Hale MJ2,4,5, Dundun O5, Kgosi T6, Kiluba J5, Lefika C5, Mabaso S5, Maluleke N5, O'leary C5, Snyman J5, Tsai WJ5, Semedo LV5, Whitehead K5
1Department of Surgery
2Department of Anatomical Pathology
3Charlotte Maxeke Johannesburg Academic Hospital
4National Health Laboratory Services
5University of the Witwatersrand
Introduction: Most common cause of MNG is iodine deficiency. Campaign to eradicate iodine deficiency has been implemented worldwide and has led to a reduction in the incidence of endemic goitre.
Aim: To study the pattern of presentation of MNG at CHBAH after introduction of the programme universal iodination of table salt in South Africa.
Methods: Retrospective study based on an audit of histology records of patients who had thyroidectomy for MNG from 01 January 2010 to 31 December 2012. Data retrieved included patients' demography, preoperative thyroid function test result, preoperative FNAC, type of thyroidectomy and histological findings. Chi-square test and Student t-test were used where appropriate, to compare findings; and significance was set at p-value < 0.05.
Results: A total of 121 records were found and 46 met the criteria. The mean age of presentation of MNG was 45.1 ± 7.5 years. 67.4% (31/46) of patients were euthyroid preoperatively and 4.3% (2/46) were hyperthyroid. 82.6% (38/46) had FNAC performed before thyroidectomy. Subtotal thyroidectomy and total thyroidectomy were performed equally, 43.5% (20/46) for each. Common histopathological findings were haemorrhage 73.9%, fibrosis 47.8%, inflammation 43.5%, cysts formation 37.0% and calcification 32.6%. Cancer was found in 4.3% and all were papillary carcinomas.
ANATOMICAL PARAMETERS OF THE ROUVIERE'S SULCUS FOR LAPAROSCOPIC CHOLECYSTECTOMY
Lazarus L1, Luckrajh JS1, Mewa Kinoo S2, Singh B2
Discipline of Clinical Anatomy, School of Laboratory Medicine and Medical Science, University of KwaZulu-Natal; 2Discipline of Surgery, School of Clinical Medicine, University of KwaZulu-Natal
Introduction: The implementation of laparoscopic cholecystectomy has seen an increase in common bile duct (CBD) injury. This may be attributed to the inherent limitations of laparoscopy. Rouviere's Sulcus (RS), a transverse cleft on the visceral surface of the liver has been identified as a suitable anatomical landmark that may mitigate the risk of CBD injury, as it lies in the same plane as the CBD. During laparoscopic cholecystectomy the induced pneumoperitoneum and the medial retraction of the gall bladder allows for the visualisation of RS. Identification of the RS will alert the surgeon to the superior extent of the CBD; thus, dissection above the plane of the RS creates a surgical "safe-zone".
Aim(s): This study aimed to describe the incidence, morphology and morphometry of RS.
Methods: A total of 75 formalin-fixed adult livers were dissected to identify and quantify the parameters of RS.
Ethical considerations: Kindly note that ethical clearance has been applied for (awaiting approval from UKZN Institutional Offices).
Results: RS was present in 82.67% of cases. The morphology of the sulcus was classified into three types viz.: Type 1A (44%) describes RS as a deep sulcus that is continuous medially with the hilum of the liver; Type 1B (6.67%) describes RS as a deep sulcus that is fused medially. Type 2 (25.33%) was slit-like, superficial and narrow. Type 3 describes RS as a scar since it appears as a fused line. RS had an average length of 3.16 cm, average breadth of 0.16 cm and an average depth of 0.78 cm.
Conclusion/Recommendations: The use of RS as an anatomical landmark may mitigate the risk of iatrogenic injury during laparoscopic cholecystectomy. Notwithstanding the value of RS as a surgical landmark, its demonstration may not be consistent in situations such as extensive gallbladder disease with adhesions and scarring, cirrhosis of the liver and fatty disease of the liver.
A TOPOGRAPHICAL AND SURGICAL ANATOMICAL DESCRIPTION OF THE RECURRENT LARYNGEAL NERVE IN ADULT AND PAEDIATRIC POPULATIONS OF SOUTH AFRICA
Kiluba J1,4, Small C1,4, Luvhengo T1,3,5, Mazengenya P1,4
1Department of Anatomical Sciences
2Department of Surgery
3Charlotte Maxeke Johannesburg Academic Hospital
4University of the Witwatersrand.
Background: Injury to the recurrent laryngeal nerve (RLN) remains among the most severe complications of a thyroidectomy and neck surgeries. The prevalence of post-surgical injury of the RLN is at most 11%, despite the overwhelming amount of literature on the anatomy of the RLN and the advent of intraoperative neural monitoring
Aim: The study was conducted to assess the normal anatomy and anatomical variations of the recurrent laryngeal nerve in a cadaveric cohort of paediatric cadavers.
Methods: Prospective study based topographical and anatomical information derived from cadaveric dissections of both male and female cadavers, donated for learning and research to the school of Anatomical Sciences at the University of the Witwatersrand. A sample of 50 cadavers, in total 100 sides, were dissected and analysed. Inferential statistics was done using Pearson Chi-square test. The level of significance was set at p-value below 0.05. Ethical permission was granted.
Results: The mean age and standard deviation of the whole group was 77.7 ± 12 years and their ages ranged from 45-95 years. All the cadavers were Caucasian. On the right side the recurrent laryngeal nerve (RLN) coursed posterior to the inferior thyroid artery (ITA) 52% of the time, with 26% and 26% coursing anterior and in-between the branches of the ITA respectively. On the left side the RLN coursed anterior to the ITA 42% (21/50), with 10% and 48% coursing posterior and in-between the branches of the ITA respectively.
The relationship of the recurrent laryngeal and its posterior course to the ITA in male and female cadavers statistically significant.
Conclusion: The recurrent laryngeal nerve is a highly variable nerve with poor predictability. The knowledge of its anatomy and variations remains the most important tool to prevent injury to this nerve in neck surgical interventions.
EVALUATION OF FACTORS AFFECTING THE OUTCOME OF RADIO-IODINE TREATMENT FOR HYPERTHYROIDISM
Docrat F1, Mokoena T1, Ankrah AO2
1Department of General Surgery
2Department of Nuclear Medicine, University of Pretoria
Introduction: Hyperthyroidism occurs due to excessive production of thyroid hormone by the thyroid gland. One modality of treatment is radio-iodine ablation but there is uncertainty of the factors that influence its effectiveness.
Aim(s): 1) Determine the cure rate in hyperthyroid patients treated with radio-iodine ablation from six months onward. 2) Identify factors which influence outcome such as: dose, antithyroid drugs, type of hyperthyroidism, age or gender of patient.
Methods: Retrospective analysis of patient record from Steve Biko Academic and Kalafong Hospitals with approval from the Human Ethics Committee of the Faculty of Health Science of the University of Pretoria.
Results: There were 205 patients collected with a female predominance of 83.8%. Females presented older compared to males (67% females vs. 40% males were 40 years or older). Graves' disease was most commonly diagnosed, 88.6%. Cure rate was 90.8%, with no statistical difference between the different gender and ages. Patients who received a second dose had a poorer outcome (r = 0.32, p < 0.001). Cure rate for those that received one dose was 94.8% (147/155) and those who received two doses was less, 60% (12/20). Patients older than 60 years tended to require only one dose of radio-iodine ablation (p = 0.027). A Chi-squared test showed an association between dose and cure rate, low dose (< = 15 mCi) 86% vs. high dose (> 15 mCi) 96% (p = 0.05). Antithyroid drugs resulted in higher number of treatment failures (pre-ablation p = 0.04 and post-ablation p < 0.001) and correlated with the number of doses received (r = -0.38, p < 0.01), implying the patient was more likely to receive a second dose.
Conclusion: Patients who received antithyroid treatment or received more than one dose of radio-iodine ablation did poorly. These outcomes can help clinicians to identify patients at risk of failure and increase the initial dose of radio-iodine ablation.
CORRELATION BETWEEN THYROID ULTRASOUND FINDINGS AND FINAL HISTOLOGY IN PATIENTS WITH INDETERMINATE FINE NEEDLE ASPIRATION CYTOLOGY RESULTS
Khalushi RE1, Jackson BS2
1Department of Surgery, Steve Biko Academic Hospital, University of Pretoria
2Department of Surgery, Kalafong Tertiary Hospital, University of Pretoria
Introduction: Most patients with indeterminate fine needle aspiration are subjected to thyroidectomy in the fear of malignancy but only 20-30% of this group is found to be malignant. Therefore 70-80% of patients are subjected to unnecessary operations which puts them at risk of complications of thyroid surgery.
Aim(s): To determine the value of thyroid ultrasound in diagnosing malignancy in patients with indeterminate fine needle aspiration cytology (FNAC) results.
Methods: A retrospective review of patient records was done from 2001 to 2015 in all patients above 18 years of age who presented with a nodular thyroid goitre, had an ultrasound, FNAC and in whom a thyroidectomy or lobectomy was performed. Approval by the University of Pretoria ethics committee.
Results: Final histology was available in 101 out of 104 patient records. Malignancy was identified in 23 (22.8%). The overall sensitivity and specificity of thyroid image reporting and data system (TIRADS) score in this study were 69.5% and 61.5% respectively. The TIRADS score had high sensitivity amongst the indeterminate 26 patients with sensitivity and specificity of 85.7% and 52.6% respectively, however it was not statistically significant with a p-value of 0.28.
Conclusion/Recommendations: For patients presenting with a thyroid nodular goitre in which the FNAC has an indeterminate result (Bethesda III and/or Bethesda IV), there is no significant correlation observed between the TIRADS score and malignancy or between the TIRADS score and the final histology. The ultrasound could therefore not diagnose cancer in these patients.
THE FREQUENCY OF MULTINODULAR GOITRE AND THYROID NEOPLASMS AFTER THE INTRODUCTION OF UNIVERSAL IODINATION OF SALT IN SOUTH AFRICA
Luvhengo T1,3,5, Hale MJ2,4,5, Dundun O5, Kgosi T6, Kiluba J5, Lefika C5, Mabaso S5, Maluleke N5, O'leary C5, Snyman J5, Tsai WJ5, Semedo LV5, Whitehead K5
1Department of Surgery
2Department of Anatomical Pathology
3Charlotte Maxeke Johannesburg Academic Hospital
4National Health Laboratory Services
5University of the Witwatersrand
Background: Both deficiency and excess iodine states predispose to benign and malignant diseases of the thyroid gland. The programme of universal iodine supplementation was introduced in 1995 in South Africa.
Aim: The study was conducted to evaluate demography and histopathological findings in a cohort of patients who had thyroidectomy after the introduction of iodine supplementation programme.
Methods: Retrospective study based on an audit of histopathology records of patients who had thyroidectomy over an 11-year period was conducted. Data retrieved included demographics and histopathological findings. The sample was split into three age groups for further analysis. Inferential statistics was done using Pearson Chi-square test and logistic regression. The level of significance was set at p-value below 0.05. Ethical permission was granted as an extension of MNG study done at Chris Hani Baragwanath Academic Hospital.
Results: A total of 693 records were found and 86.1% (593/693) of the patients were females. The mean age of the whole group was 48.1 ± 15 years and their ages ranged from 20-90 years. 57.0% (395/693) of the thyroidectomies were for neoplastic conditions. 0.2% (2/693) of thyroidectomies was for Graves' disease whereas 2.3% (16/693) were for Hashimoto's thyroiditis. Thyroid cancer was found in 3.6% (25/693) of the specimens and 64.0% (16/25) were papillary carcinomas. 25.0% (4/16) of papillary carcinomas occurred in the background of Hashimoto's thyroiditis.
Patients in the age groups 41 to 60 and over 60 years accounted for 81.1% of thyroid cancers. The difference in cancer occurrence in the 20 to 40 compared to over 60 years was statistically significant with p-value of 0.029.
Conclusion: An overwhelming majority of thyroidectomies are still done for benign conditions. More thyroidectomies are performed for Hashimoto's thyroiditis than for Graves's disease. The most commonly reported cancer is papillary carcinoma and 25% occur in the background of Hashimoto's thyroiditis.
MORTALITIES IN LIVER TRAUMA AT A JOHANNESBURG TRAUMA UNIT: WHAT CAN WE LEARN?
Joubert IM, Oyomno MD, Jonas L, Pholosi M, Gyebi S, Goosen J, Motilall SR, Moeng MS
Trauma Unit, Charlotte Maxeke Hospital, Universty of Witswatersrand, Johannesburg
Introduction: Liver trauma can have devastating outcomes despite optimal care. Multiple factors, including physiological derangements and injury severity, may impact on outcome. Investigating the specific factors influencing outcomes of liver trauma in our unit will afford us an opportunity to identify factors that require improvement, to optimise future patient care.
Aim: Identify factors associated with mortality in patients with liver injuries presenting at CMJAH.
Method: Severe trauma patients who presented with liver injuries at the trauma unit from 01/06/2005 to 30/04/2011 were included in the study. Demographic data, mechanism of injury, injuries sustained, physiological parameters including RTS, ISS, percentage survival based on ISS and mortality outcomes were all analysed. A p-value of < 0.05 was considered statistically significant.
Findings: A total of 714 patients were recruited. Penetrating trauma accounted for 50.6% (n = 361) of the study population. Patients were predominantly male; 85% (n = 307) of the penetrating and 72% (n = 255) of the blunt trauma group. Blunt trauma had a higher median ISS (29 vs. 17), lower predicted percentage survival (51.5% vs. 98%), lower RTS (4.6 vs. 6.4), higher actual mortality (52.4% vs. 21.6%). Blunt trauma patients were more likely to have associated injuries than the penetrating injuries - severe chest injuries in 50.1% vs. 34.1%, severe pelvic fractures in 16.1% vs. 0%, severe head injuries in 43.3% vs. 1.3%). However, blunt trauma patients had slightly fewer complex liver injuries (49.6% vs. 51.8%), and major intra-abdominal vascular injuries (5.38% vs. 21.1%).
Conclusion: Mortality was higher in blunt liver injuries compared to penetrating injuries. This is probably due to the higher incidence of associated severe head, chest and pelvic injuries. Early recognition of associated injuries may impact on mortality.
THE EFFECT OF HUMAN-IMMUNODEFICIENCY VIRUS STATUS ON OUTCOMES IN PENETRATING ABDOMINAL TRAUMA - AN INTERIM ANALYSIS
Macpherson D, Neuhaus V, Edu S, Nicol AJ, Navsaria PH
Trauma Centre, Department of Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
Background: The purpose of this study was to determine whether the outcomes of haemodynamically stable patients undergoing exploratory laparotomy for penetrating abdominal trauma differed as a result of their HIV-status.
Methods: This was an observational, prospective study from February 2016 to May 2017. All haemodynamically stable patients with penetrating abdominal trauma requiring a laparotomy were included. The mechanism of injury, the HIV status, age, the penetrating abdominal trauma index (PATI), and the revised trauma score (RTS) were entered into a binary logistic regression model. Outcome parameters were in-hospital death, morbidity, admission to intensive care unit (ICU), relaparotomy within 30 days, and length of stay longer than 30 days.
Results: A total of 209 patients, 94% male, with a mean age of 29 ± 10 years were analysed. Twenty-eight patients (13%) were HIV positive. The two groups were comparable. Ten (4.8%) laparotomies were negative. There were two (0.96%) deaths, both in the HIV-negative group. The complication rate was 34% (n = 72). Twenty-nine patients (14%) were admitted to ICU. A higher PATI, older age, and a lower RTS were significant risk factors for ICU admission. After 30 days, 12 patients (5.7%) were still in hospital. Twenty-four patients (11%) underwent a second laparotomy. The PATI score was the single independent predictor for complications, relaparotomy and hospital stay longer than 30 days.
Conclusions: Preliminary results reveal that HIV status does not influence outcomes in patients with penetrating abdominal trauma.
FACTORS PREDICTING OUTCOME IN ADULT TRAUMA PATIENTS ADMITTED TO A TERTIARY ICU
Ndaku RB, Pearce NE
Department of Surgery, University of Free State
Introduction: Trauma remains the single most important cause of mortality and morbidity in South Africa. Unnatural causes account for up to 42% of mortality in the youth aged between 20-24 years. The overall mortality of trauma patients in Intensive Care Unit (ICU) has been shown to be between 13.9% -66%.
Aim: The aim of this study is to correlate the outcome of patients that are admitted to ICU following trauma of any mechanism. In this study, outcome is measured by: 1) Morbidity and 2) The length of stay in both ICU and the total stay in the hospital.
Methods: Retrospective analysis of records of 322 admissions over a period of five years.
Results: 322 patients met our inclusion criteria. The mean age of our study population was 33. There were 262 males (81%) and 62 females (19%). The total readmissions was 1.86% (n = 6) of which 33% of the patients survived (n = 2) and 66% died (n = 4), all within five days of readmission. Motor vehicle accident was the most prevalent mechanism of injury (35%) with domestic violence being the least (2%). Peak presentation time of patients was between 08:00-08:59. The highest mortality rate was seen amongst burn patients (78.8%), p-value 0.0001; and the lowest in orthopaedic patients. Longer ICU stay, mechanical ventilation and sepsis correlated with outcome.
Conclusion: Mechanism of injury, neurosurgical trauma and age of patient predict outcome of trauma patients in ICU in our study; this correlates with international norms.
OUTCOMES OF MAJOR TRAUMA PATIENTS RECEIVING PRE-HOSPITAL ADRENALINE FOR HAEMODYNAMIC INSTABILITY AT CHARLOTTE MAXEKE JOHANNESBURG ACADEMIC HOSPITAL
Kinandu K, Nel M, Moeng MS
Department of Surgery, University of Witwatersrand
Introduction: Trauma is a major cause of morbidity and mortality in South Africa. Currently more than five million people lose their lives as a consequence of major trauma. Current fluid resuscitation guidelines for shock are acceptable to most centres, but there is still debate on the role of vasopressors. This is even more so for vasopressor use in the prehospital setting. Some studies have indicated that early vasopressor usage maybe associated with increased mortality, though prehospital data is limited.
Aim: To determine if prehospital adrenaline use in major trauma patients with hypotension results in higher in-hospital mortality in the South African context.
Methods: This was a retrospective study of patients 18 years and older, who presented at CMJAH trauma unit, after major trauma with prehospital BP < 90 mmHg. Study period was 72 months (2011-2016). Demographic, physiological, prehospital adrenaline use, 24 hr and 30 day mortality data were collected. Statistical analysis was done using STATA V14, and p-value of < 0.05 was considered significant. [Wits Ethics Number M160750]
Results: Four hundred and sixty (460) of the eligible 8 210 major trauma patients were included. Thirty two (32) received prehospital adrenaline; 428 did not. The 24 hr mortality rate and 30 day mortality in patients receiving prehospital adrenaline was 37.5 % and 37.5% respectively in comparison to 7.2% and 12.4% in patients not having received adrenaline. Patients receiving adrenaline were found to be 7.7 times more likely to have 24 hr mortality than patients not receiving adrenaline (p-value = 0.21) and patients receiving adrenaline were 4.2 time more likely to have 30 day mortality than patients not receiving adrenaline (p-value = 0.52).
Conclusion: The prehospital adrenaline use in our study was associated with a higher 24 hourr and overall 30 day mortality, though these results were not statistically significant.
INDICATIONS, MORTALITY, AND LONG-TERM OUTCOMES OF 50 CONSECUTIVE PATIENTS UNDERGOING DAMAGE CONTROL LAPAROTOMY FOR ABDOMINAL GUNSHOT WOUNDS
Twier K1, Hartford L1, Nicol AJ1, Edu S1, Roberts S2, Ball CG2, Navsaria PH1
1Trauma Centre, Groote Schuur Hospital and University of Cape Town
2Trauma and Acute Care Surgery, University of Calgary, Foothills Medical Center, Calgary, Alberta
Background: Outcomes of patients undergoing damage control laparotomy (DCL) for abdominal gunshot wounds (GSWs) remains relatively unknown. The aim of this study was to evaluate the impact of DCL on long-term morbidity and survival.
Methods: A retrospective study of patients undergoing a damage control laparotomy for abdominal GSWs was conducted. Data was collected on 50 consecutive trauma patients over a 4.5-year period between 01 August 2004 and 30 September 2009. Patients were stratified by age, perioperative physiological parameters, trauma indices, numbers of abdominal GSWs, and critical care unit and hospital length of stay, morbidity and mortality. Unadjusted and adjusted estimates of the association between these factors and the odds of survival were computed with univariate and multivariate logistic regression.
Results: Most patients were male (96%) with a mean age of 29.7 years and had a single abdominal gunshot wound (60%). Liver injuries (58%) followed by small bowel (44%), majors venous (40%), and colonic (38%) trauma were seen. The overall mortality was 54%. The mean of length of intensive care unit stay and mean hospital length of stay was seven and thirteen days respectively. Factors associated with a decreased odd of survival included Penetrating Abdominal Trauma Index (PATI) > 25, intraoperative blood lactate level > 8 mmol/L, and massive transfusion > 10 units PRBCs.
Conclusion: The overall mortality was 54%. Amongst this cohort, there is significant evidence that after controlling for confounding factors, a PATI score of > 25 is associated with decreased odds of survival (OR: 0.20, p-value 0.04).
THE SELECTIVE NON-OPERATIVE MANAGEMENT OF PENETRATING CERVICAL VENOUS TRAUMA IS SAFE AND EFFECTIVE
Madsen AS, Bruce JL, Oosthuizen GV, Bekker W, Laing GL, Clarke DL
Pietermaritzburg Metropolitan Trauma Service, Department of Surgery, University of KwaZulu-Natal; College of Health Sciences, and Department of Surgery, University of the Witwatersrand, Johannesburg, South Africa
Background: This paper reviews our experience with penetrating cervical venous trauma and aims to validate the selective non-operative management (SNOM) of these injuries.
Methods: This was a retrospective review of a prospectively maintained registry. All patients presenting alive with an injury to the internal jugular vein, subclavian vein or innominate vein following a PNI were reviewed for a six-year period.
Results: Among 817 patients admitted for the management of PNI, 76 (9.3%) had a venous injury. Of these, 37 (48.7%) patients were managed non-surgically, 20 (26.3%) required immediate surgical exploration, seven of whom had an associated arterial injury, and 19 (25%) underwent surgery following a diagnostic CTA, 16 of whom had an associated arterial or aero-digestive injury. In total, only 16 (21.1%) of the 76 patients required exploration for venous injury alone. The majority (63.2%) of patients had a history of severe bleeding or haemodynamic instability prior to arrival, but only 20 (26.3%) required immediate exploration.
Two (2.6%) patients died as a result of venous injury. No patients developed complications related to the venous injury.
Conclusions: SNOM is applicable to a well-defined subset of patients with isolated penetrating cervical venous trauma to the IJV and SCV identified on CTA.
PROCALCITONIN-GUIDED ANTIBIOTIC THERAPY FOR SUSPECTED AND CONFIRMED SEPSIS OF PATIENTS IN A SURGICAL-TRAUMA INTENSIVE CARE UNIT
Chomba R, Lowman W, Moeng MS
Johannesburg Trauma Unit, Charlotte Maxeke Hospital and University of the Witwatersrand
Introduction: Procalcitonin (PCT) can be used to make a decision to stop antibiotics based on declining PCT values. However, most studies involve medical patients in developed countries. There is paucity of data regarding PCT-guided antibiotic algorithms in surgical trauma patients and patients from developing countries.
Aim: Evaluate PCT in a surgical trauma ICU.
Method: A prospective study was conducted in the surgical trauma intensive care unit (ICU) at Charlotte Maxeke Johannesburg hospital in 2015 in a two-period cross-over design. In the first period, 40 patients were recruited as controls and antibiotics were stopped as per standard of care. In the second period, 40 patients were recruited into the intervention group and antibiotics were discontinued if the PCT decreased by > 80% from the peak PCT level, or to an absolute value of less than 0.5 μg/L. Patients were followed up for 28 days after the first sepsis event.
Results: The intervention group had a mean antibiotic duration of 9.3 days while the control group was treated for a mean duration of 10.9 days for the first sepsis event. Clinician compliance to the PCT algorithm was 62.5%. The intervention group had more antibiotic free days (7.8 days) compared to the control group (3.9 days) (p = 0.004). There were no differences between the two groups in terms of relapse of infection, length of ICU stay, hospital stay or 28-day mortality.
Conclusion: Our data supports the use of a PCT-guided algorithm for antibiotic stewardship in surgical trauma patients. Clinician compliance will increase the benefits observed in our study.
SELECTIVE NON-OPERATIVE MANAGEMENT OF PHARYNGO-OESOPHAGEAL INJURIES SECONDARY TO PENETRATING NECK TRAUMA: A SINGLE-CENTRE REVIEW OF 86 CASES
Madsen AS1, Oosthuizen GV1, Bruce JL1, Bekker W1, Laing GL1, Clarke DL2
1Pietermaritzburg Metropolitan Trauma Service, Department of Surgery, University of KwaZulu-Natal, Nelson R Mandela School of Medicine, Pietermaritzburg, KwaZulu-Natal, South Africa
2Department of Surgery, University of the Witwatersrand, Johannesburg, South Africa
Introduction: This paper describes our experience with penetrating pharyngo-oesophageal injuries (PEI) in the light of a selective conservative approach, and has the objective to define criteria for non-operative management (NOM).
Aim: We tested our hypothesis that NOM is safe for haemodynamically stable patients with PEI, who have no competing indications for exploration, have no established sepsis and who have a water-soluble contrast swallow (WSswallow) either showing no- or a contained extravasation.
Methods: This was a retrospective single-centre review of patients with penetrating neck injury (PNI) treated for confirmed PEI over a six-year period. Patients were identified from a prospectively maintained trauma registry. Ethics approval was given.
Results: Eighty-six (9%) patients with PEI (oropharynx: 17, hypopharynx: 40, oesophagus: 29) out of 948 patients with PNI were included. Of the cohort, 38 (44%) underwent NOM (oropharynx: 15 [88%], hypopharynx: 18 [45%], oesophagus: 5 [17%]) and 48 (56%) were managed operatively. The median length of stay (LOS) was 12 days (IQR: 19-8). Fifteen (17%) had a persistent leak and six (7%) mediastinitis. Five (6%) patients died but only one (1%) had isolated PEI. Retrospectively, 27 patients fulfilled our proposed criteria for NOM of which 23 had been treated actively by NOM (oropharynx: 8, hypopharynx: 12, oesophagus: 3). For these patients the LOS was 10.0 days (IQR: 13-6) and none developed deep wound sepsis, mediastinitis, persistent leaks, or died. Of the remaining patients treated by NOM without fulfilling the proposed criteria, two were palliated (oesophagus) and 13 managed actively (oropharynx: 7, hypopharynx: 6). Only four of these patients (oropharynx: 1, hypopharynx: 3) were assessed with WS-swallow, which showed non-contained extravasation, and three complicated with persistent leaks.
Conclusions: NOM of PEI is safe for a carefully selected subgroup of patients. However, most injuries to the caudal part of the cervical digestive tract mandate urgent exploration.
EFFECTIVE RADIATION DOSE RECEIVED BY SEVERELY INJURED TRAUMA PATIENTS DURING EMERGENCY INVESTIGATIONS
Booi Z, Moeng M, Candy G
University of the Witwatersrand
Background: Assessment of severely injured (P1) trauma patients include extensive investigation of all the injuries sustained with an intent to minimise missed injuries. Amongst the investigations conducted are radiological studies that invariably expose these patients to radiation with its possible complications. In our setting these include LODOX, x-rays and computed tomography (CT) scans. In this study we quantitatively estimated the amount of radiation received by P1 trauma patients during their admission to ED.
Materials and Methods: A retrospective study. The data collected included P1 patients, over the age of eighteen, admitted to CMJAH trauma ED over a period of six months. The primary end point was to estimate the amount of radiation received by these patients during radiological investigations. The amount of radiation received was also compared according to mode of injury sustained.
Results: Out of the 6623 patients seen in CMJAH ED
during the six-month period of the study, only 1173 patients met all the inclusion criteria. P1 trauma patients received a considerable amount of radiation during their admission to ED. CT scans were responsible for most of the radiation received. On the other hand, LODOX exposed patients to the least amount of radiation. Patients with blunt trauma received more radiation compared with patients with penetrating trauma.
Conclusion: Radiological investigations expose P1 trauma patients to a considerable amount of radiation. Requesting these investigations, critical as they may be in the management of severely injured trauma patients, must be done with full cognizance of the amount of radiation they impose on these patients. LODOX, because of its low radiation and its ability to scan the whole body, makes it a favourable equipment to have in an emergency department. Focused x-rays can then be done as suggested by findings from the LODOX, correlating this with the clinical picture of the patient.
PENETRATING FEMORAL ARTERY INJURIES: AN URBAN TRAUMA CENTRE EXPERIENCE
Rayamajhi S1, Murugan N1, Nicol A1, Edu S1, Klopper J2, Naidoo N,3 Navsaria P1
1Trauma Centre
2Division of Surgery and Vascular Surgery
3Groote Schuur Hospital and Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa
Aim: This study reviews a single-centre experience with penetrating femoral artery injuries.
Methods: The records of all patients with femoral artery injuries admitted to the trauma centre at Groote Schuur Hospital from January 2002 to December 2012 were reviewed. These were analysed for demographics, injury mechanism, perioperative, and surgical management. Outcome was categorised by limb salvage.
Results: One hundred and fifty-eight (158) patients with femoral artery injuries were identified. There were 144 (91%) men and 14 women with a mean age of 28 years. Ninety-five percent (n = 150) sustained penetrating injuries. The superficial femoral artery (87%) was most commonly injured. The most common type of arterial injury was a laceration (39%) and transection (37%). Eighty-one (51%) patients had a primary repair, 53 (33%) patients had a vein interposition graft, and 16 patients (10%) had a prosthetic graft. There were 78 (51%) concomitant venous injuries, 11 were repaired, and one vein patch repair was performed (15.4%). There were four (2.5%) primary amputations and 10 (6.5%) secondary amputations.
There were no deaths. Statistically significant risk factors for secondary amputation derived by univariate analysis were: ischaemia (p < 0.0001), neurological deficit due to ischaemia (p < 0.001), temporary vascular shunting (p < 0.001), and the absence of a palpable pulse post-repair (p < 0.01).
Conclusion: This study has a primary and secondary amputation rate of 2.5% and 6.5%, respectively. There was greater than 90% limb salvage rate. The outcome of threatened limbs due to femoral artery injury is good, provided that there is no delay to surgery.
WHICH TRAUMA INJURY GROUP SHOULD BE THE MAIN FOCUS OF OUR PREVENTION STRATEGY BASED ON THE JOHANNESBURG TRAUMA DATA OVER EIGHT YEARS
Pswarayi RM, Monzon BI, Goosen J, Moeng MS
Johannesburg Trauma Unit, Charlotte Maxeke Hospital and University of the Witwatersrand
Background: Trauma is a preventable disease. However, the resource constraints, and the multiple needs of the country dictate that we should be able to prioritise the strategy for an effective solution. We wanted to assess which of the prevention groups will most benefit from a well-planned prevention strategy. This information may guide the outreach responsibilities of the unit and help refocus on the group to be targeted the most.
Aim: Analyse the load of trauma to a busy Johannesburg trauma unit to guide prevention strategy policy of the unit.
Methods: Retrospective study of all P1 patients seen at the CMAJH. Data collected from 01 May 2005 till 31 December 2012. Demographics, mechanism of injury, the ISS, NISS and probability of survival were analysed. Data was also compared over the different years for pattern recognition. The mechanisms were also assessed according to the four age groups. Statistical analysis was done and the p-value of < 0.05 was considered significant.
Results: The age group of 21-45 were the most injured in the 18 087 study sample. Penetrating trauma was seen in 48,64% of cases, blunt in 47,16%, burns in 1, 06% and miscellaneous in the remaining 3.14%. The average ISS of the mortalities ranged from 26 to 41, and NISS from 46 to 49. Stab injuries constituted of 32.3% of the cases, even though their mortality was only 2,22%. They were followed by GSW at 16,34%, although their mortality was 10.67%. Pedestrian vehicle collisions contributed 13.31% of cases with mortality of 15,99%. Motor vehicle collisions were the fourth highest group (12,95%) with 11,5% mortality.
Conclusion: Although the stab injuries were the most common, they had the lowest mortality. Blunt trauma had much higher mortality figures. Prevention strategy aimed at penetrating trauma will reduce the most number of casualties but not necessarily of mortalities.
INTERPERSONAL VIOLENCE PRESENTATION AT THE JOHANNESBURG TRAUMA UNIT - WHO IS AT RISK IN OUR EIGHT-YEAR ANALYSIS?
Pswarayi RM, Goosen JG, Moeng MS
Johannesburg Trauma Unit, Charlotte Maxeke Hospital and University of the Witwatersrand
Background: Trauma in South Africa is a major challenge with up to 60% of the victims known to their assailants. It is important to evaluate the load and distribution patterns of the presenting trauma cases, in order to plan better and offer a holistic trauma care. CMJAH sees significant load of GSW, stab and assault cases per annum. Closer look at these injuries will offer an opportunity to understand the patterns of injuries seen.
Aim: Audit and compare outcomes in victims of interpersonal violence presenting at the CMJAH over an eight-year period.
Methods: Retrospective study from 01 May 2005 till 31 December 2012. Trauma bank data, and clinical notes and mortality figures will be analysed. Demographics, mechanism of injury, ISS and NISS, age distribution, in-hospital mortality were recorded and analysed. The GSW, stabs and common assault cases were further compared to each group over the study period. Burns were excluded in this analysis.
Results: Of the 18 087 subjects entered in the study, 10 793 (59, 67%) were involved in interpersonal violence. Stabs accounted for 54, 06% of the group, followed by GSW in 27, 45% and blunt assault in 18, and 49%. The 21-45 age group was the most vulnerable of the three groups, majority of whom were male. GSW had the highest mortality of 10,67% with the average ISS of 22 and NISS of 42 in the mortality group, even though the blunt assault mortality group had the highest average ISS of 26 and NISS of 49. This is despite the GSW having the highest average predictability of survival of 70% on ISS and 64% on NISS.
Conclusions: Interpersonal violence accounts for approximately 2/3 of the trauma load at the Johannesburg trauma unit. Stabs are the most common mechanism of interpersonal injury, but GSW have the highest mortality despite better probability of survival in the unit.
A RETROSPECTIVE COMPARISON BETWEEN OPERATIVE AND NON-OPERATIVE MANAGEMENT FOR MULTIPLE RIB FRACTURES
Monzon BI, Fingleson LM, Ortega M, Markovic S, Moeng MS
University of the Witwatersrand and Sunninghill Hospital
Background: Surgical rib fixation is gaining popularity as an alternative to the standard of care for multiple rib fractures. Recent literature suggest that rib fixation offers advantages over non-operative management by reducing ICU and hospital stay, facilitating early return to normal productive activities as well as shortening time on ventilator and some reduction in the incidence of pneumonia.
Methods: A retrospective descriptive review of the initial results of surgical rib fixation compared to non-operative management in patients with rib fractures over a 24-month period in a private trauma unit.
Results: Thirty-five patients with rib fractures were admitted over the study period, 11 females and 24 males, majority between the ages of 31 and 45 years. The most common causes of fractures in our population were motorcycle crashes (12/35, 34.2%), and falls (11/35, 31.4%). Over 70% of cases had three or more rib fractures, and nine patients (25.7%) had flail chest. Fourteen (40%) of the 35 patients were considered candidates and offered surgical fixation based on the number, location and symptoms related to the ribs fractured. Surgery was performed in the first seven days after admission in 85.7% of cases. The overall length of ICU and hospital stay was 6,5 and 8,5 days respectively. There were no differences between the two groups regarding: number of fractured ribs, injury severity score, ICU or hospital stay. Patients treated without operation needed longer to return to normal activities compared to those operated (seven weeks versus three weeks). Overall there were eight complications recorded; only two (2) were directly attributable to surgery. There were no deaths.
Conclusions: Despite the small number of patients in our study, surgical fixation of the ribs seems a viable alternative to the conventional non-operative management of ribs fractures.
MORBIDITY AND MORTALITY IN PAEDIATRIC SURGERY AT NELSON MANDELA ACADEMIC HOSPITAL THREE YEARS OF STUDY
Loko EM, Delgado A, Mpikashe M
Nelson Mandela Academic Hospital
Introduction: Children account for about 30% of the South African population of 15 years aged. Globally, surgical volumes are large. However, there is scarce data on surgical morbidity and mortality in the paediatric surgical population in South Africa.
Aim: To determine the causes of morbidity and mortality in our health facility.
Methods: We did a retrospective study on morbidity and mortality of paediatric patients in emergency and elective cases, admitted and treated from January 2015 to April 2018 in our centre. Variables studied in our patients were: age group, gender, diagnosis, emergency surgical indication vs. elective surgery.
Results: 1 615 patients were included in our study; of these 1 519 were more than 28 days old and less than 13 years, and 96 were neonates. In the neonatal group 72% were male and 28% female; by a ratio of 2.57/1, anorectal malformation (ARM) was the anomaly more frequently found (34.37%), followed by intestinal atresia with 11.46%. The mortality rate of surgical neonate cases was 16.67%; of these the higher mortality rate was seen in patients with gastroschisis (40%) followed by intestinal atresia with 27% and bowel malrotation 25%.
Among the 1 519 patients aged more than 28 days, the emergency surgical causes represented 55%. Among this group acute appendicitis was observed in 51%, and, as cause of admission, represented 93% of the non-trauma emergencies, followed by the trauma cases (3%) and elective cases (22%) of all admissions. Four percent of admissions resulted from snake bite and 5% from foreign body ingestion. Thus the mortality rate in this group was 0.53% of all cases.
Conclusion: Acute appendicitis and ARM were the more frequently observed. The surgical volume of paediatric patients was large, however the mortality rate was low.
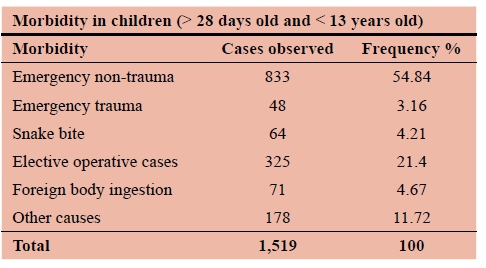
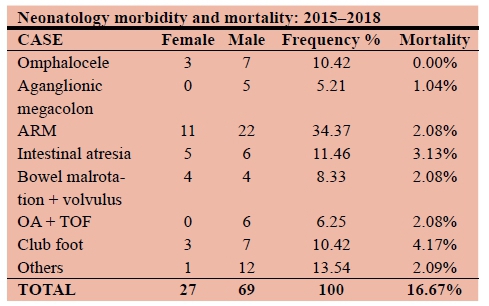
METABOLIC SURGERY IN SOUTH AFRICA -AN INITIAL ACADEMIC HOSPITAL EXPERIENCE
Webner A, Lubbe J, Potgieter A, Odendaal WJ, Cooper CE, Lambrechts AVV
Department of Surgery, Tygerberg Academic Hospital and Stellenbosch University, SA
Introduction: In South Africa, 42% of adult females, and 13.5% of adult males are classified as obese, the highest recorded numbers in sub-Saharan Africa. Metabolic surgery has been proven to be a safe and effective treatment, yet due to demand on government resources has only been performed to a limited extent in public hospitals.
Aim(s): The aim of this study was to describe the experience with metabolic surgery at a single academic hospital.
Methods: This was a single-centre retrospective review of all metabolic surgery procedures performed from October 2011 to September 2017. Ethics approval by the Stellenbosch University Health Research Ethics Committee.
Results: A total of 57 patients underwent laparoscopic metabolic surgery, 56 (89%) Roux and Y gastric bypass, and 1 (2%) sleeve gastrectomy. The follow-up rate at one year was 97%. Mean preoperative BMI was 59 kg/m2, and comorbidities included type 2 diabetes mellitus (42%), hypertension (60%), and dyslipidaemia (37%). There were no conversions to open surgery and at one year mean percentage total weight loss was 27.62+/-8 and mean percentage excess body mass index loss was 50.4+/-15.78. Overall morbidity was 14%, with 3 (5%) classified as major and 5 (9%) as minor.
Conclusion/Recommendations: This study confirms that metabolic surgery can be performed safely in an academic hospital in South Africa. As outcomes are closely related to both surgeon and centre volume, as well as long-term patient compliance, and taking into account both the socio-demographic index and the increased obesity numbers in South Africa, the role of metabolic surgery remains to be determined. Larger scale studies and cost analyses are needed to answer these questions.
THE SURGICAL MANAGEMENT AND OUTCOME OF GASTROINTESTINAL STROMAL TUMOURS AT TYGERBERG ACADEMIC HOSPITAL AND ITS DRAINAGE AREA
Leitch AM, Hofmeyr S
Department of Surgery, University of Stellenbosch
Introduction: Gastrointestinal stromal tumours (GIST) are uncommon. Local data concerning their presentation, management and outcome are limited.
Aims: To describe the mode of presentation, surgical management, anatomical location, histopathological characteristics and survival of GIST managed at Tygerberg Academic Hospital and its drainage area.
Methodology: A retrospective cohort study of cases identified from the NHLS anatomical pathology database dating back the last 20 years. University of Stellenbosch Health Research Ethics Committee approval was obtained (HREC S16/07/137)
Inclusion criteria: Age > 13 years; patients treated at Tygerberg Academic Hospital and its referral hospitals. Exclusion criteria: incomplete clinical records and patients without histopathological confirmation of GIST.
Results: Of 85 patients identified, 71 met the inclusion criteria. The median age presentation was 64 years (range 30-84). Female:male ratio was 1,5:1. Gastrointestinal bleeding and abdominal pain were the most common presenting complaints. Twenty-eight percent of GIST were larger than 10 cm. Sixty-eight percent of specimens had a low mitotic count (< 5/50 HPU). The stomach was involved in 68%, small bowel 10%, large bowel 4%, duodenum 4% and other 14%. Metastases were present in 14 patients (20%). Imatinib use was infrequent (14%). Five-year overall survival was 67%. (International OS = 70.2%)
Conclusions: GIST presented at a similar age to international data. The large size of GIST at presentation suggests that our cases present late. The distribution of GIST and presence of metastases and overall survival were similar to international findings.
Recommendations: Collaboration between institutions will recruit larger numbers for the study of uncommon tumours and conditions.
PREVALENCE OF HUMAN PAPILLOMA VIRUS IN BREAST CANCER
Maroga N1, Mhlongo LN1, Mokoena TM1, Bida NM2, Nyila M2
1Department of General Surgery
2Anatomical Pathology and Life and Consumer Science, University of Pretoria
Introduction: Human papilloma virus (HPV) varies greatly between geographic variations. Different countries have different HPV genotypes. The prevalence data of HPV in breast cancer is much higher in areas with high incidence of HPV. There is no data regarding HPV association with breast cancer in South Africa.
Aim: To study the prevalence of HPV in breast cancer at Steve Biko Academic Hospital with the aim of getting guidelines for management and preventative public health approach to reduce breast cancer incidence.
Methods: Ethics approval for conducting the study was obtained from the University of South Africa ethics committee, Head of the Anatomical Patholoy Department, Head of General Surgery and CEO of Steve Biko Academic Hospital.
Results: Of 60 formalin-fixed paraffin embedded breast tissue samples studied, 22 sample tested negative for human β-globin DNA and were excluded for HPV. The detection of HPV DNA in any of the 38 human β-globin-positive samples was 0, resulting in 100% HPV DNA negative. We however, do not deny the possibility that the undetected HPV play a role in breast carcinogenesis in Steve Biko Academic hospital patients.
Conclusion: The complete absence of HPV DNA in the breast cancer samples does not support the etiological role of oncogenic HPV in the pathogenesis of breast cancer in the study population.
Abstract 55_
THE CLINICOPATHOLOGICAL SPECTRUM OF APPENDICITIS MANAGED AT KING EDWARD VIII HOSPITAL
Simelane PB, Aldous C, Madiba TE
Department of Surgery, University of KwaZulu-Natal, Durban
Introduction: Appendicitis is a common surgical condition which requires accurate and early diagnosis. If complicated it can be a deadly condition.
Aim: To describe the presenting pattern and clinicopathological spectrum of appendicitis at King Edward VIII Hospital, Durban.
Methods: This was a retrospective descriptive study involving a review of 244 patients' files from 2010 and 2012 at King Edward VIII hospital. Data collected and analysed included demographics, clinical picture, and delay in presentation, operative findings and outcome. Ethical approval was obtained from UKZN, Ref: BE082/14.
Results: A total of 244 patients were included in the study. The M:F ratio was 1.7:1. The mean age was 26.62 (6.70). Pre-hospital delay was 3.08 (1.53). Pre-hospital delay was < 1 day in 28 patients and > 1 day in 216 patients. Presenting symptoms were right iliac fossa (195), classical pain (30), and peritonitis (48), nonspecific pain (25) and generalised abdominal pain (39), appendix mass (6) and appendix abscess (61). 179 patients underwent appendectomy via Lanz incision and the rest underwent laparotomy. Intraoperative findings were inflamed appendix (119) and complicated appendicitis (125). There were no deaths in patients with simple appendicitis and eight patients died among the patients with complicated appendicitis (8.6%). No deaths occurred in patients with delay < 1 day compared to eight patients (3.7%) in patients with delay > 1 day. Ten patients required critical care admission with median ICU stay of 3.5 days (1-7days); all ten patients had prolonged pre-hospital delay and complicated appendicitis. Hospital stay was 5.3 + 3.4 days (3.8 + 1.9 days for simple appendicitis and 6.8 + 4 days for complicated appendicitis).
Conclusion: Classical symptoms were uncommon. Complicated appendicitis and prolonged pre-hospital delay were associated with admission to critical care, mortality and prolonged hospital stay.
EXPERIENCE WTIH THE MANAGEMENT OF ANORECTAL FISTULAE
Dube GQ, Aldous C, Madiba TE
Department of Surgery, University of KwaZulu-Natal, and Colorectal Unit, Inkosi Albert Luthuli Central Hospital, Durban
Introduction: Anorectal fistula is a common condition but its management is challenging for the surgeon.
Purpose: To describe our experience with the management anorectal fistulae.
Methods:
• Study setting: Colorectal Unit, Inkosi Albert Luthuli Central Hospital, Durban.
• Study population: Patients referred to the Colorectal Unit for the management of anorectal fistula between 2005 and 2017 form the basis of this study.
• Study design: Retrospective analysis of a prospectively collected data of patients with anorectal fistulae. Simple fistulae were managed with fistulotomy. Complex fistulae with an internal opening had seton insertion followed by definitive procedure. Complex fistulae without an internal opening underwent fistulectomy ab initio. Ethical approval was obtained from UKZN (Ref. BE230/13).
Results: A total of 122 patients were analysed over the 13-year period, M:F ratio was 2.5:1 and mean age was 43.7 + 11.9 years. Aetiology was cryptoglandular (116), tuberculosis (4), trauma (1), and surgery (1). HIV status was negative (25), positive (37). Median number of previous operations was 2 (range 1-14). The number of fistulae per patient ranged from 1-4. The fistulae were left-sided (61), right-sided (25), bilateral (20) and central (12). There were 17 horseshoe abscesses. Two patients had an associated RVF. Definitive procedures undertaken were fistulectomy (9), excision of chronic abscess (3), LIFT (37), fistulotomy (6), removal of seton + completion fistulotomy (30), Modified Hanley Procedure (9) and non-operative (1). Eleven patients have not reached the stage of definitive procedure and two patients with failed treatment have been lost to follow-up.
Complications were residual anal incontinence (6), iatrogenic simple fistula (3), perineal numbness (1), and pelvic haematoma (1). Primary healing rate was 85% over 1-7 months. No patients died during treatment.
Conclusion: The vast majority of fistulae were cryptoglandular in origin. Current management confers benefit and is associated with acceptable outcome in our setting.
DIABETIC FOOT AMPUTATION IN EGYPT: WHY SHOULD EVERY US VASCULAR SURGEON CARE?
Shalaby SY1,2, Dardik A2
1 Department of Surgery, Witwatersrand University
2Department of Surgery, Yale University
Introduction: With Egypt making the top 10 ranking of diabetes mellitus, prevalence of retinopathy is 20.5%, neuropathy at 21.9%, however, diabetic foot complications 1%. How does this contrasting trend between diabetic foot complications and other diabetic complications compare to the United States (US) to determine healthcare expenditure in preventing major diabetic foot amputations?
Methodology: Estimation of diabetic population at risk of lower limb amputation in Mansoura, Egypt (aged 25+ years old) in the year 2008-2013 was determined using percent Growth Rates equation. Prevalence of diabetic lower limb amputations in Mansoura was estimated using recorded total (below and above knee) diabetic lower limb amputations in Mansoura University hospital from 2009-2012. Based on these measures, the prevalence of diabetic foot amputation in Mansoura is estimated. Egypt's overall prevalence of diabetic foot amputation was estimated as a larger scale of Mansoura's prevalence of diabetes taking in account the difference in diabetic population. The results and other published trend in Egypt were compared to all Medicare Parts A and B Fee-forService Cohort Population.
Results: After calculating Egypt's prevalence of major diabetic foot amputation, there is consistent decrease in major diabetic foot amputations with an average of 0.3% of the diabetic population (0.5% average for all diabetic foot amputations in other large studies in Egypt). Comparing this phenomenon to prevalence of diabetic foot amputations in the US, the prevalence is much higher, with 1.3% and 1.8% of diabetic patients undergoing a major or lower extremity amputation. However, diabetic foot in Egypt at 6.9%, is still lower than the US.
Conclusion: Prevalence of diabetic foot amputation is decreasing both in Egypt and the US but with a much larger prevalence rate in the US. This may be accounted for by environmental or personal habits that may play a pivotal role in preventing diabetic foot amputations.
ANAL SQUAMOUS CELL CARCINOMA IN KWAZULU-NATAL. FACTORS INFLUENCING OUTCOME
Zuma N1, Ngidi S1, Madiba TE2
1Departments of Radiation Oncology
2Surgery, University of KwaZulu-Natal, Durban
Introduction: Anal cancer is a rare malignancy, of which squamous cell carcinoma (SCC) is the more common. However, the incidence in certain populations, is increasing.
Purpose: To determine the clinicopathological spectrum of SCC in HIV-positive and -negative patients.
Methods: This is a retrospective analysis of prospective collected database spanning a period of17 years. Data analysed included demographics, clinical picture, stage, pathology, and treatment outcome. The study outcome measures were clinicopathological spectrum, treatment outcome and follow-up. Data were extracted onto an Ms Excel Spreadsheet and analysed. Ethical approval was obtained from UKZN, Ref.: R057/04.
Results: Among the 327 patients with anal cancer diagnosed between 2000 and 2017, 258 (79%) had SCC and 69 had anal adenocarcinoma. Among the 258 with SCC, 137 accepted VCT, of whom 108 were HIV infected and 29 were HIV negative. Median age at presentation was 39 years among HIV-positive patients and 52 years among HIV-negative patients. Staging is shown in Table I.
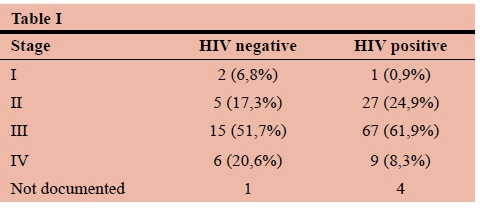
Of the HIV-positive patients 54% received definitive chemoradiation, and 32% received palliative treatment, with 6% undergoing resection. The outcome was complete response (12%) and partial response (14%). Overall survival was 95 months and disease-free survival (DFS) 41 months.
Among the HIV-negative patients, 45% had definitive chemoradiation, 35% had palliative radiation, and 17% underwent resection. The outcome was complete response (17%) and partial response (21%). Overall survival was 146 and DFS was 75 months.
Conclusion: There were more HIV-positive than HIVnegative patients. HIV-positive patients presented at a younger age than HIV-negative patients. There were more HIV-positive patients with locally advanced disease and survival was poorer.
THE EFFECTS OF MALIGNANCY ON HERNIA RECURRENCE AND PERIOPERATIVE OUTCOMES OF LAPAROSCOPIC VENTRAL HERNIA REPAIR (LVHR)
Shalaby SY1,2, Gutierrez DB2, Menzo EL2, Szomstein S2, Rosenthal R2
1Department of Surgery, Witwatersrand University
2Department of Surgery, Cleveland Clinic, Florida
Introduction: LVHR is associated with fewer complications and shorter length of stay (LOS) than open hernia repair. However, history of cancer is not well defined with regards to prevalence, complications, and risk of recurrence in LVHR.
Methods: The records of all patients who underwent a laparoscopic hernia repair between November 2012 and February 2016 at the Cleveland Clinic Florida Hospital were included in this retrospective review. The groups were frequency-matched on age. Patients were considered to have a malignancy diagnosis using International Classification of Diseases codes for diagnosis. Recurrence was both self-reported and found on clinical revisit and defined as recurrence when verified by a clinician and/or radiologist.
Results: A total of 53 of 103 patients (51%), female reproductive system (breast, ovarian, cervical, and uterine) were the predominant malignancies (41.5%) followed by gastrointestinal (GI) malignancies, colon and rectum, (22.6%), skin (18.9%), prostate (13.2%), renal cell carcinoma (7.5%), liver (3.8%), lung (3.8%), transitional cell carcinoma (1.9%), and Kaposi sarcoma (1.9%). Patients had similar demographics and comorbidities except for history of occurrence of postoperative surgical site infection (7.5% vs. 0%, p = 0.03), diabetes mellitus (DM) (35.8% vs. 17.5%, p = 0.01), hernia area (46.0 ± 58.7 cm2 vs. 28.6 ± 45.8 cm2, p = 0.008), number of prior of hernia repairs (2.0 ± 1.1 vs. 1.3 ± 0.6, p = 0.01), and an enlarging hernia as a primary indication of surgery (52.8% vs. 26.2%, p = 0.001). Patients with cancer had marginally significant longer operative time (5.7% vs. 1.0%, p = 0.08), increased mesh use (94.3 vs. 82.7%, p = 0.04), larger mesh implanted (340.4 ± 27.5 cm2 vs. 270.4 ± 17.6 cm2, p =0.03), and longer hospital stay (2.9 ± 0.5 days vs. 2.0 ± 0.2 days, p = 0.02). History of cancer was significantly associated with hernia recurrence (HR = 2.18, 95 % CI = 0.21 - 4.16, p = 0.03) after adjusting for age, gender, diabetes, body mass index (BMI), and history of occurrence of postoperative surgical site infection.
Conclusion: Patients with history of cancer may be considered a high risk group for LHR and history of a cancer diagnosis is an independent risk factor for hernia recurrence. Larger studies are required to validate these results.














