Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.55 no.4 Cape Town Nov. 2017
ABSTRACTS
Cape Town Trauma Congress (TSSA/SAOTS) Congress Abstracts
ANALYSIS OF THE COMPLICATIONS OF VOLAR PLATE FIXATION FOR THE TREATMENT OF DISTAL RADIUS
S Xaso, M Ramokgopa, S Magobotha
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: Distal radius fractures constitute 15% of all fractures. A certain percentage of these fractures require open reduction and internal fixation using a volar plate. This may result in some of the patients experiencing complications. There is no study done yet in South Africa aimed at analysing these complications. The literature review from oversees studies shows a wide range of complication incidence but more or less similar rate for each complication.
Aim: The aim of the study is to evaluate the incidence of complications after open reduction and internal fixation using a volar plate in distal radius fractures. The hypothesis is that complications after open reduction and internal fixation using a volar plate for distal fractures occur less in patients treated at Chris Hani Baragwanath Academic Hospital compared to the results shown in the current literature.
Objectives: The study objectives: 1) To establish the incidence of complications post volar plate application; 2) To establish the relationship between complications, and surgical and patient related factors; and 3) To establish the functional outcome using DASH score and handgrip dynamometer.
Method: This is a retrospective study with a prospective recall that will be conducted at Chris Hani Baragwanath Academic Hospital. The study population will include patients from 18 years of age and above who were managed operatively with volar plating between January 2015 and December 2016. The study is looking at sample size of 120 patients with minimum follow up of six months.
The discussion for the congress will detail more the results of the current literature review of the complications after volar plate application for distal radius fractures, and the analysis of the results obtained thus far as the study is still underway.
A NOVEL APPROACH TO THE MANAGEMENT OF FRACTURE BLISTERS
M van Heukelum, T Bason, T Franken
Stellenbosch University, South Africa
Ethics approval: Needs to be acquired
Purpose of Study: Fracture blisters are a frequently encountered challenge facing orthopaedic surgeons. The management their off remains a clinical dilemma.
According to the literature, their true etiology is unknown, their occurrence and location is unpredictable and no consensus exists in terms of treatment of fracture blisters or their impact on subsequent surgery.
The study presents a current literature review on fracture blisters and aims to evaluate the outcome of using Aquacell dressings in the management thereof as well as the subsequent effect of surgical incision in close blister proximity (photographic catalogue of cases).
Description of Methods: A case series is under way at a district orthopaedic unit looking at fracture blister management. All blisters are initially cleaned with betadine solution and then de-roofed. The Exposed blister bed is then covered with a layer of Aquacell (Fibrous Hydrocolloid) dressing.
Underlying fracture are temporarily stabilised and elevated.
Dressings are removed at one week and fracture specific ORIF is performed.
All fractures with surgical incisions through or close to fracture a blister are then followed up to assess wound healing, tissue breakdown, surgical site sepsis and fracture healing.
Summary of results: To date 25 patients have been managed in this way, all have shown remarkable re-epithelialisation of the blister bed after 5-7 days. 10/25 (40%) of them requiring incision through blister site. So far we have experienced one case of wound break down.
Conclusion: Fracture blisters are a clinical dilemma for orthopaedic surgeons. There is no universal consensus on the appropriate treatment of this soft tissue injury when treating the underlying fracture. The most serious concerns with fracture blisters are skin compromise following surgical incisions and infection.
We suggest a novel way to manage this condition which is cost effective, minimises the delay to surgery, and provides good clinical outcomes.
A RETROSPECTIVE COMPARISON BETWEEN OPERATIVE AND NON-OPERATIVE MANAGEMENT FOR MULTIPLE RIB FRACTURES
B I Monzon, L M Fingleson, S Markovic, M S Moeng
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Background: Surgical rib fixation is gaining popularity as an alternative to the standard of care for multiple rib fractures. Recent literature suggest that rib fixation offers advantages over non operative management by reducing ICU and hospital stay, facilitating early return to normal productive activities as well as shortening time on ventilator and some reduction in the incidence of pneumonia.
Methods: A retrospective descriptive review of the initial results of surgical rib fixation compared to non-operative management in patients with rib fractures over a 24-month period in a private trauma unit.
Results: 35 patients with rib fractures were admitted over the study period, 11 females and 24 males, with the majority between the ages of 31 and 45 years. The most common causes of fractures in our population were motorcycle crashes (12/35- 34.2%), and falls (11/35-31.4%). Over 70% of cases had three or more rib fractures, and nine patients (25.7%) had flail chest. 14 (40%) of the 35 patients were considered candidates and offered surgical fixation based on the number, location, and symptoms related to the ribs fractured. Surgery was performed in the first seven days after admission in 85.7% of cases. The overall length of ICU and hospital were 6,5 and 8,5 days respectively. There were no differences between the two groups regarding: number of fractured ribs, injury severity score, ICU or hospital stay. Patients treated without operation needed longer to return to normal activities compared to those operated (seven weeks versus three weeks). Overall there were eight complications recorded; only two were directly attributable to surgery. There were no deaths.
Conclusions: Despite the small number of patients in our study, surgical fixation of the ribs seems a viable alternative to the conventional non-operative management of ribs fractures.
A SURVEY OF THE USE OF TRACTION BY SPECIALISTS FOR THE REDUCTION OF CERVICAL DISLOCATIONS
N Kruger, M Workman
University of Cape Town, South Africa
Ethics approval: Needs to be acquired
Introduction: There is an increasing body of literature supporting early decompression of spinal cord injuries especially in low energy cervical dislocations. Closed cervical reduction is a safe and rapid mechanism to achieve this, however, its use and acceptance amongst specialists is poorly described.
This study aimed to assess the training, experience, and decision making of trainees and surgeons who manage cervical spine dislocations with the goal of implementing further training and refresher courses as necessary.
Methods: Orthopaedic and neurosurgery registrars and specialists in South Africa were emailed a questionnaire consisting of 13 questions related to their training, experience, and management of cervical dislocations. Data was analysed using descriptive statistics. We reported categorical data in tables with frequencies and percentages. Normality of the data was tested qualitatively and responses were compared.
Results: 79% of surgeons were taught closed reduction during specialist training. Of the neurosurgeons, 92% covered spine trauma compared to 66% of orthopaedic surgeons. Of those surgeons who provide trauma cover, 64% are comfortable performing closed cervical reduction but 36% would refer to a colleague accepting a two hour delay in treatment. 60% of respondents feel confident in completing closed cervical reduction in under four hours. 38% of neurosurgeons vs of 3% orthopaedic surgeons preferred MRI prior to closed reduction. 51% of surgeons thought that the risk of worsening neurology during traction was up to 25% but 69% of surgeons felt ER doctors could safely perform closed cervical reduction with training. 81% of surgeons do not think surgical reduction is routinely possible in under four hours.
Conclusion: There are some misconceptions around cervical traction which may affect clinical practice and optimum management. It is a safe procedure that does not require prior MRI and carries an extremely low risk of worsening a patient's condition. Closed cervical traction reduction is the most rapid, safe mechanism to reduce cervical dislocations and requires education of undergraduates, emergency doctors, and specialists to increase awareness of the reduction process.
A SURVEY OF THE USE OF TRACTION BY SPECIALISTS FOR THE REDUCTION OF CERVICAL SPINE DISLOCATIONS
M Workman, N Kruger
University of Cape Town, South Africa
Ethics approval: Needs to be acquired
Introduction: Literature supports early decompression of low energy cervical spine dislocations. Closed reduction can safely and rapidly achieve this. However, its use and acceptance amongst specialists is poorly described. This study aimed to assess the training, experience and decision making of trainees and surgeons who manage cervical spine dislocations with the goal of implementing further training and refresher courses as necessary.
Methods: Orthopaedic and neurosurgery registrars and specialists in South Africa were emailed a questionnaire consisting of 13 questions related to their training, experience and management of cervical dislocations.
Results: 79% of surgeons were taught closed reduction during specialist training. Of neurosurgeons, 92% covered spine trauma compared to 66% of orthopaedic surgeons. Of surgeons covering trauma, 36% would refer, accepting a two hour delay in treatment. 38% of neurosurgeons vs 3% of orthopaedic surgeons preferred MRI before closed reduction. 51% of surgeons thought that the risk of worsening neurology during traction was up to 25%. 69% of surgeons felt ER doctors could safely perform closed cervical reduction with training. 81% of surgeons do not think surgical reduction is routinely possible in under four hours.
Conclusion: There are some misconceptions around cervical traction which may affect clinical practice and optimum management. It is a safe procedure not requiring prior MRI and carries a low risk of worsening a patient's condition. Closed cervical traction reduction is the most rapid, safe mechanism to reduce cervical dislocations and requires education of undergraduates, emergency doctors, and specialists to increase awareness of the reduction process.
A VALIDATION OF THE SIMPLIFIED MOTOR SCORE IN THE ASSESSMENT OF PATIENTS WITH TBI IN SOUTH AFRICA.
J J P Buitendag1, A Ras1, V Kong1, J Bruce1, D Clarke1, P Brysiewicz2
1Pietermaritzburg Metropolitan Trauma Service, Department of Surgery, University of KwaZulu Natal, Durban, South Africa
2School of Nursing & Public Health, University of KwaZulu-Natal, South Africa
Ethics approval: Needs to be acquired
Introduction: This study uses data from a large prospectively entered database to assess the efficacy of the M score component of the GCS and the Simplified M Score (SMS) at predicting overall outcome in patients with a TBI. The aim is to simplify the scoring system used to assess level of consciousness of trauma patients in the acute setting.
Methods: A retrospective observational review of the Pietermaritzburg Metropolitan Trauma Service Hybrid Electronic Medical Registries database performed for the period January 2013 to December 2015 . Patients were classified into three groups using GCS as an injury severity score. These were mild TBI (GCS13-15), moderate TBI (GCS 9-12), and severe TBI (GCS9). Glasgow Motor Score was specifically evaluated to determine the relationship between individual motor component and outcome of patients.
Results: A total of 830 patients were used during this study. The GCS score for these patients were broken down, and the M score analysed. There is a decline in survival rate when the M score on admission is four or less. The decline is more significant when M score is three or less. A total of 41 patients with an M score of one were treated, only 11 (26,8%) survived. A total of 22 patients with a M score of two were treated, only 14 (63,6%) survived. A total of 23 patients with a M score of three were treated, only 13 (56,5%) survived. A survival rate of 56,5%. A total of 25 patients with a M score of four were treated and 20 (80%) survived. A total of 128 patients with a M score of five were treated and 121 (94,5%) survived. Finally 591 Patients with M score of six were treated, of which 580 (98%) survived. As SMS deteriorated so mortality rose dramatically. This was highly significant. When plotting M score against mortality out of 830 patients there was a correct prediction in 769 cases. The accuracy was 92.7%, sensitivity 67.6% and specificity 95%. The areas of the ROC was 0.9037 with a std. Dev. (Area) = 0.0227. When comparing Simplified M score against mortality the accuracy was 77.1% the sensitivity 84.5% and specificity: 76.4%. The fitted ROC Area: 0.891 and empiric ROC Area: 0.86.
Conclusion: The M score component of the GCS and the SMS accurately predicts the outcome of patients with TBI. In cases where full GCS is difficult to assess the M score and SMS can be safely used as a triage tool.
ABDOMINAL INJURY IN THOSE WITH TRAUMA ABOVE DIAPHRAGM OR BELOW THE PELVIC DIAPHRAGM
D J J Muckart1,2, M Mayet3, T C Hardcastle1
1 University of KwaZulu-Natal, South Africa
2 Inkosi Albert Luthuli Central Hospital, South Afica
3 University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Objective: To determine the incidence of intra-abdominal injury using CT angiography in patients sustaining blunt trauma with obvious injuries above the thoracic and below the pelvic diaphragm.
Methods: In a retrospective analysis de-identified patient data were extracted from an approved prospective database of patients admitted to the Trauma ICU at Inkosi Albert Luthuli Central Hospital for the period from April 2007 to March 2011. All blunt polytrauma patients with injuries above the diaphragm and below the pelvic floor were included, provided they were investigated by a full-body trauma Computed Tomography Contrast Study or had to undergo emergency laparotomy due to haemodynamic instability and/or those judged to have clinically obvious intra-abdominal injury. Simple statistical data analysis techniques were used with descriptive statistical methods.
Results: Of 284 patients with injuries above the thoracic and below the pelvic diaphragm, 202 (71.1%) had no intraabdominal injuries, and in 82 (28.8%) intra-abdominal injury was identified. From those 82 patients, 38 (46.3%) were treated non-operatively, and 24 (29.2%) were treated surgically with regard to their abdominal injuries, while 20 (24.4%) of those 82 patients demised (four as a result of intra-abdominal injuries and 16 as a result of extra-abdominal injuries).
Conclusion: Less than one-third of patients with injuries above the thoracic and below the pelvic diaphragm have concomitant intra-abdominal injuries. Of these, just over half required laparotomy. In the haemodynamically stable patient CT scanning identifies the need for surgical intervention.
ASSESSMENT OF ELBOW FUNCTIONAL OUTCOME AFTER CLOSED REDUCTION AND PERCUTANEOUS PINNING OF DISPLACED SUPRACONDYLAR FRACTURES IN CHILDREN
A B Rutarama, G B Firth, Y Ramguthy
Ethics approval: Needs to be acquired
Purpose of the study: To assess elbow functional outcome after closed reduction and percutaneous pinning of displaced supracondylar fractures in children.
Methods: A prospective cohort study was done at two Academic Hospitals in South Africa. All patients with unilateral Gartland Grade 3 supracondylar fractures aged 5-14 years between 30 April 2016 and 30 July 2016 were recruited, follow up ended 14 January 2017.Range of movement (ROM) included flexion, extension, pronation and supination and was measured at three, six, 12 and 24 weeks after surgery using a goniometer. Control measurements were taken from the contra-lateral normal elbow. X-Rays were taken at six weeks. Wilcoxon paired tests were used to compare ROM at six versus control and versus 24 weeks. Mann - Whitney paired t test was used to assess influence of age on ROM. The Paediatric Outcome Data Collection Instrument (PODCI) was used at 24 weeks. Complications were noted.
Results: 38 patients were included in the study. The mean age of the cohort was 7.5 years (SD 2.5). 25 patients were male. 29 patients had left sided fractures.At six weeks versus controls, Elbow Extension was significantly reduced (p 0.0094).There was a significant improvement in all ROM for the cohort between six and 24 weeks (p 0.0001). At 24 weeks, ROM was still significantly reduced (p 0.0001). Patients under seven years of age recovered elbow Extension fastest(p 0.0011). Six patients had Ulnar nerve palsy, three patients had a Volkmann's ischaemic contracture, one had a compartment syndrome and one had a radial nerve palsy. Nerve injuries recovered spontaneously by the 12th week. Regarding the PODCI, 95% of parents were satisfied with the results at 24 weeks.
Conclusion: Significant improvement in ROM was observed between six and 24 weeks. At six weeks versus control, Elbow Extension was noted to be the most affected. Patients under the age of seven recovered elbow Extension the fastest. 95% of parents were satisfied with the outcome. Those with open injuries and compartment syndrome had a fixed flexion deformity more than 30 degrees.
BURDEN OF LOWER LIMB LONG BONE FRACTURES TREATED IN CHRIS HANI BARAGWANATH ACADEMIC HOSPITAL
S M Tlhabane, N Iqbal
Ethics approval: Needs to be acquired
Introduction: Long bone fractures are both a burden to the private state hospitals. They cost both the state and private health care a lot of money annually. Adequate human and financial resources are required for optimal management of this injuries. In South Africa the incidence of motor vehicle accidents remains exceedingly high despite the government road safety measures. World wide, road injuries cause over 1.3 million deaths and one in ten injuries involve femoral shaft fractures treated with surgery (Kiran et al). South african Road Federation(SARF) says South Africa still has the second highest road accident fatality rate per 100 000 population in Africa. Femoral shaft fractures have bimodal distribtuion with annual incidence in USA of 10 per 100 000 population and tibial diaphyseal fracture estimated to be 109 per 100 000. There are no South African statistics and the study was aimed at determining the number of this fractures treated in CHBAH per year and the cost thereof.
Aim and objectives: To determine the number of intramedullary nails, external fixators, plate and screws used to treat femur and tibia shaft fractures.
To determine the costs of treatment of this injuries.
Methods: It's a retrospective study over a two year period. The lower limb weekly clinical audits were reviewed restrospectively from January 2015 - December 2016. Finacial records were requested from hospital finance deparment to analyse the cost of treatment of this injuries per year.
Results: Long bone fractures of the lower limb that required surgery accounted for approximately a third of all lower limb injuries admitted over the two year period. Average implants price was found to be 12 000 rand per patient.
Conclusion: Long bone fractures are a burden to the hospital and put a strain to both human and financial resources. We concluded that the burden is related to the high incidece of road accident crashes per year.
C1 OPTIMAL MASS SCREW INSERTION -A COMPUTER AIDED ANALYSIS
R Krassnig1, G M Hohenberger1, U Berzins1, E Tackner1, A Schwarz2, P Puchwein3
1 Medical University of Graz, Austria
2 Allgemeine Unfallversicherungsanstalt - Trauma Hospital Graz, Austria
3 Medical University of Graz, Austria
Ethics approval: Needs to be acquired
Background: Surgical stabilisation of C1 ring fractures is usually favored in highly unstable fractures. Motion preserving techniques are increasingly used especially in young patients. Therefore lateral mass screws are inserted in the second vertebra and connected by a rod. Safe screw positioning is important to avoid harm to the medulla oblongata or the vertebral artery.
Purpose: The purpose of this study was to determine safe zones regarding the vertebral arteries and the medulla oblongata for optimal lateral mass screw positioning when fusing the C1-ring.
Study Design: Basic scientific anatomic and radiologic study.
Methods: Images of the cervical spine of 50 patients (64-line CT scanner) were evaluated and virtual screws were positioned in both lateral masses of the first vertebra using 3D-reconstructions of CT-scans. The length of the screws, the insertion angles in two planes, the distance to the vertebral artery, and the spinal canal were investigated. Descriptive statistics was used, gender depend differences were calculated using student-T-test. A diameter of 4 mm was chosen for the screws.
Results: The mean screw length was 30.0 ± 2.3 mm on the right and 30.1 ± 2.1 mm on the left side. The arithmetic mean for the transverse angle was 16.4 ± 5.6° on the right and 15.6 ± 6.3° on the left, the sagittal angle averaged 8.3 ± 3.8° on the right and 11.0 ± 4.9° on the left side. The mean distance between screw and spinal canal has been determined on the right with 2.4 ± 0.7 mm and 2.2 ± 0.6 mm on the left side. The distance from the C1 lateral mass screw to the vertebral artery was on average 7.1 ± 1.5 mm on the right side (significant correlation with gender, p-value: 0.03) and 7.5 ± 1.4 mm on the left side.
Conclusion: Due to the required high precision technique intraoperatively multiplanar 2D or 3D imaging is recommended to avoid harm to the vertebral artery or the spinal canal.
CIVILIAN GUNSHOT WOUNDS TO THE CHEST: A CLINICOPATHOLOGICAL ANALYSIS OF AN ANNUAL CASELOAD AT A LEVEL 1 TRAUMA CENTRE
V M Meijering, A T Hattam, P H Navsaria, A J Nicol,
S Edu
University of Cape Town, South Africa
Ethics approval: Needs to be acquired
Background: Gunshot wounds (GSW) to the chest are common presentations to trauma centres in South Africa. The clinical management and outcome of GSW to the chest are significantly altered by missile trajectory and the associated anatomical structures injured making them challenging injuries to treat. Currently, the management of GSW chest is based on scant evidence and treatment is typically according to algorithms based largely on the anecdotal experience of high volume institutions and experienced clinicians.
Aims: To utilise an established prospective database of one of world's busiest Trauma Centres to analyse the clinicopathological aspects of all patients with GSW to the chest. This work may strengthen the body of knowledge pertaining to the treatment of GSW to the chest and may then contribute to an evidence-based, management algorithm for such injuries.
Materials and Methods: Ethical approval was obtained for this study. The Electronic Trauma Health Registry (eTHR) Application of the Trauma Centre at Groote Schuur Hospital in Cape Town was interrogated for the year 2015 for all patients with GSW chest. The data was then analysed using descriptive statistics.
Results: A total of 141 patients with GSW to the chest were admitted to the Trauma Centre with a median age of 26 years. More than half of the patients, 53, 2% (n = 75) sustained an isolated GSW to the chest. Overall, 29, 1% (n = 41) patients sustained a thoraco-abdominal injury, which accounts for a significant higher amount of emergency surgeries compared to patients with non thoraco-abdominal injuries (54% vs 15%, p =<0, 01). 9, 2% (n = 13) of all patients required an emergency thoracotomy or emergency chest surgery of which five patients survived. Overall mortality was 7,1% (n = 10) of which five patients died from a thoracic cause.
Conclusion: Civilian GSW to the chest are common injuries seen in Cape Town, often with concomitant injuries leading to increased morbidity. Significantly more emergency surgeries were done in patients with thoraco-abdominal injury. Overall few patients needed chest-related emergency operative intervention (9, 2%) with a survival rate of 38, 5%. Overall mortality of patients with GSW chest who reached the hospital was 7,1% of whom 50% died from a thoracic cause.
CORRELATION OF KNEE MRI AND ARTHROSCOPIC FINDINGS AND THE EFFECT OF TIME ON DIAGNOSTIC RELIABILITY
T Ncube, S Magobotha
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: The knee is indispensable in everyday life and injuries to it can be debilitating and significant loss of earnings may be incurred. Clinical diagnosis may not always be made with certitude and Magnetic Resonance Imaging (MRI) helps further elucidate intra-articular injuries. This study aims to test the diagnostic reliability of MRI done in a teaching hospital for the evaluation of anterior cruciate ligament and meniscal injuries using arthroscopy as the gold standard. Due to the long patient waiting times to have surgery we set out to determine if there is a change in the reliability of an MRI result as time elapses.
Methods: A retrospective review of records of patients who had knee arthroscopies at an urban teaching hospital in Johannesburg, South Africa was done. Consecutive adults (16 - 60 years) with one major event of trauma to the knee and had MRI done prior to surgery at the above institution were included. Arthroscopy was done by tw senior surgeons or by residents under their direct supervision. Arthroscopic findings of anterior cruciate ligament (ACL) and medial (MM) or lateral meniscal (LM) injuries were compared to MRI findings. Data was analysed by STATA 13.1 to determine injury demographics, sensitivity, specificity and diagnostic accuracy of MRI. The effect of time interval from MRI to surgery on the diagnostic accuracy was determined.
Results: A total of 72 patients (74 knees) qualified for review. The median age was 35 years (IQR 26-43) with a significant difference between males and females (28 vs 41 years, p = 0.0019). Leading causes of injury were traffic accidents (32.4%), falls (27.0%), and sports injuries (17.6%). Median interval from MRI to surgery was 71.5 days (IQR 29-143). The sensitivity of MRI for ACL, MM and LM injuries was (63.6%, 58.8% and 52.6%), specificity (92.7%, 86.0% and 80.0%) and diagnostic accuracy (79.7%, 79.7% and 73.0%) respectively. The patients were divided into subgroups of early (16 weeks) post-MRI. There were marked differences in the diagnostic accuracy in the three groups for the ACL (70.8% vs 92.6% vs 73.9%) and LM (62.5% vs 81.5% vs 73.9%). This was unremarkable for the MM (75.0% vs 81.5% vs 82.6%).
Discussion: MRI findings correlate well with arthroscopic findings making it a reliable preoperative screening tool for ACL and meniscal injuries. However, its diagnostic accuracy appears to change with time. It is apparent that the diagnostic accuracy is higher between 6-16 weeks post MRI. A bigger cohort would help determine a waiting time interval that leads to significant depreciation in MRI diagnostic accuracy.
Conclusion: Despite the good correlation between MRI and arthroscopic findings, surgeons should be aware that the reliability of an MRI result decreases with time.
EARLY FACTORS PREDICTING OUTCOME OF DAMAGE CONTROL LAPAROTOMIES (DCL)
R du Toit, M S Moeng, C P Candy, J Goosen, K D Boffard
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: Damage control surgery carries a high mortality, and the decision to do so may be made too late. There is a need for early decision-making both the emergency room and theatre. The surgeon needs key parameters to aid decision-making.
Aim: To identify early predictors of mortality due to inadequate organ perfusion (first 48 hours after injury), and predict the need to perform (earlier) damage control surgery.
Materials and Methods: Retrospective review of damage control laparotomies recorded on the trauma registry of Charlotte Maxeke Johannesburg Academic Hospital Trauma Unit (01/05/2005- 31/12/2009). Parameters shown in Table 1 were compared between survivors and non-survivors. p-value of <0.05 was deemed statistically significant.
Results: Gunshot wounds were the most common mechanism of injury in both groups. Survival at 48 hours was 55% (n = 100/181). Key results are tabulated:
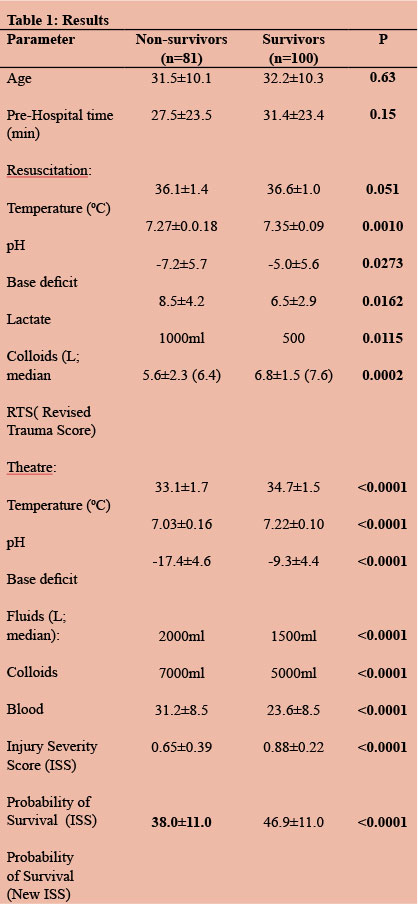
Regression analysis showed the best predictors of mortality to be: resuscitation pH (0.0003), intra-operative volume of colloid (p=0.0078) and blood (p <0.0001) temperature, pH base deficit (all <0.0001) and blood loss (p = 0.0025).
Conclusions: Emergency room parameters which significantly predicted mortality, and the need for damage control surgery, were: pH, base deficit, lactate, and RTS. Intraoperative parameters which significantly predicted mortality were: Temperature, metabolic acidosis, volume of colloid and/ or blood transfused.
EMERGENCY HYBRID TREATMENT OF A TRAUMATIC AORTIC ARCH PSEUDOANEURYSM
M Marone, I d'Alessio, A lista, R Vercelli, B Palmieri
Vascular surgery ASST grande ospedale metropolitano Niguarda, Italy
Ethics approval: Needs to be acquired
Introduction: Blunt thoracic aortic injury (BTAI) is a rare occurrence (incidence 1-2%) and only 8-18% of them occur at the aortic arch level. We present the case of a 51-year-old man, selected from the 42 cases we dealt with between 2004 and 2010 with BTAI at arch level injuried by a high energy precipitation. The patient suffered from hypercholesterolemia and mild diastolic hypertension, both in treatment.
Methods: The patient reached the ER with BP 110/80, HR 80, SatO2 98%, RR 12/min, Hb 9.4 g/dL, Lat 1.5 mmol/L, GCS 15, ISS 50. CT scan showed the presence of a 17 mm mid aortic arch pseudoaneurism, associated with 16 mm mediastinal hematoma, in addition we found a first rib fracture, Tile B basin fracture and left femoral fracture. Given the proximity of the pseudoaneurysm to the left carotid artery, it was decided to perform a frontal carotid-carotid bypass (PTFE 8 mm) with tangential clamping and NIRS monitoring. Then we excluded the pseudoaneurysm deploying a GORE CTAG 31-26-100 with proximal landing near to the anonymous trunk.
The postoperative period required 72 hours in Intensive Care Unit followed by repair of orthopedic injuries.
Results: Post-operative CT monitoring demonstrated the exclusion of the pseudoaneurysm and the patency of the bypass. The patient was discharged on day 73 and subsequent imaging (CT at 6-12 months) showed an unchanged clinical picture.
Conclusions: BTAIs are rare and complex lesions to handle; they require an open or hybrid therapeutic approach. The presence in our hospital of an Hybrid Room allowed us to solve the problem with a single intervention on the lesion, minimising anesthesiologic, intra and postoperative risks in a politraumatised patient.
FACILITIES FOR TRAUMA CARE IN BOTSWANA - AN ASSESSMENT
T Hardcastle1,2, M Mwandri1
1 University of KwaZulu-Natal, South Afica
2Inkosi Albert Luthuli Central Hospital, South Africa
Ethics approval: Needs to be acquired
Introduction: On the one hand Botswana faces a high incidence of trauma, and on the other hand lack resources for mitigating the scourge of these injuries. The World Health Organisation (WHO), recommends studying local capacity and determinants for improving trauma care. This study evaluates trauma-resources as per WHO recommendations.
Method: Two main-referral and 1-district hospitals were convenience-sampled using a questionnaire with 87-items assing for the presence of equipment and consumables for airway, breathing and circulation problems; laboratory, and radiology-services: and knowledge of providers assessed based on ATLS®.
Results: Assessment of resources for initial airway and breathing management found 16 out of 18 components available in two hospitals, and 18 out of 18 in the third hospital. Four components (emergency-room theater, Intraosseous needles, arterial, and venous pressure monitoring) out of 13 for management of circulatory-problems were absent in all three hospitals. Assessment of providers' knowledge with randomly selected doctors and six nurses in two shifts (total six doctors and 12 nurses) revealed that none of the doctors or nurses had undertaken any of trauma-courses, including ATLS®. All nurses and half of the doctors scored below 50%. The district hospital could only perform six out of 30 essential-surgical-procedures considered important in a major hospital based on Essential Trauma Care and DSTC™ guidelines. The referral-hospitals could perform 28 out of 30 procedures. There was presence of the necessary, and supporting services for trauma-care such as: theater, rehabilitation, orthotic, occupational and social-work services, arterial blood gases-analysers, and ventilators in the emergency-room. None of the hospitals had a designated trauma-team, or any organisational-structures particular to trauma-care.
Conclusion: Botswana underperforms on some elements according to WHO trauma-care guidelines. Remediation of deficiencies could be improved by following these guidelines.
FACTORS INFLUENCING MORBIDITY RATES AFTER PANCREATIC STAB WOUNDS
H Bookholane, J E J Krige, E Jonas, U K Kotze, M Bernon, M Burmeister
University of Cape Town, South Africa
Ethics approval: Needs to be acquired
Background: Penetrating injuries of the pancreas may result in serious complications. This study assessed the factors influencing morbidity after stab wounds of the pancreas.
Methods: A retrospective univariate cohort analysis was done of all pancreatic stab wounds documented in a prospective dedicated departmental pancreatic injury database of 475 patients treated between 1982 and 2016.
Results: 87 (80 men) patients, median age 26 years (range 16-62) had stab wounds of the pancreas. Median RTS was 7.8 (range 2.0-7.8). Injuries involved head/uncinate process (n = 16), neck (n = 2), body (n = 40) and tail (n = 29) of the pancreas. All 87 patients underwent a laparotomy. 68 patients had AAST grade I or II injuries and 19 had grade III, IV, or V pancreatic injuries. Eight (10.3%) of 78 patients had an initial damage control operation. 74 (85.1%) patients had drainage of the pancreas only, 11 had a distal pancreatectomy and two had a Whipple resection. 14 patients developed pancreatic complications, of which 8 were fistulae. Four (4.6%) patients died. Grade of pancreatic injury (AAST grade I-II vs grade III-V injuries; p <0.01), presence of shock on admission (p <0.01), need for a blood transfusion (p <0.01) and an associated visceral vascular injury (p <0.001) had a significant influence on the development of general complications.
Conclusions: Although mortality was low after a pancreatic stab wound, morbidity was high. Increasing AAST grade of injury, shock on admission to hospital, need for blood transfusion and an associated vascular injury were significant factors related to morbidity.
FIVE YEAR ANALYSIS OF 10 892 PATIENTS CLASSIFIED AS P1 IN A SINGLE CENTRE: THE CHARLOTTE MAXEKE JOHANNESBURG ACADEMIC HOSPITAL EXPERIENCE
C Livhebe, I M Joubert, J G Goosen, M S Moeng
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduciton: Trauma remains a pandemic in RSA despite the HIV/AIDS, Chronic diseases and infectious diseases. It accounts for significant mortality in the young and potentially productive members of society. Despite this reality, there is still no national Trauma statistics to assist in analysing this pandemic and contribute to constructive preventative strategies. We, at Charlotte Maxeke Johannesburg hospital Johannesburg Trauma unit embarked on a creating a computerised data entry to have a clearer understanding of trauma in the unit.
Aim: Evaluation of injury patterns and outcomes of P1 patients admitted at a Johannesburg Trauma unit over a five year period.
Methods: All P1 patients who were admitted to Johannesburg Trauma unit from 01 January 2005 till 31 December 2009 were included in the study. The demographic data (age, sex), physiological parameters (BP/ISS/NISS), mechanism of injury (MVC,PVC, stabs, GSW etc) was entered. Days of the week of presentation to emergency department and time spend in the department were also documented. Confirmed diagnoses and anatomical regions injured were also documented. Mortality outcomes and sites were also analysed. Procedures performed in emergency department or theatre, were documented. Length of time spend in emergency department was documented. Statistica V8 will be used as a tool for analysis.
Results: A total of 10 892 were captured on the Medibank electronic system. 2009 had the highest number of P1 patients (n = 2370) and 2007 was the lowest (n = 1920).
Majority of the patients presented over the weekend (n = 6 383), peaking on Saturday (n = 2 594). Midweek, Wednesday was the overall quietest day (n = 1 046). More male patients were seen in this period than females (n = 9 473 v/s n = 1 419), accounting for 86.3% of the study population. Age ranged from less than 1 years old to greater than 90 years of age. The 21-30 year-old group was most predominant (n = 5 587), followed by 31-40 year old (n =2 739). Penetrating trauma accounted for 52.1% of the mechanism of injury (n = 5 677), with the stabs predominating (n = 3 444).Most stab were experienced in year 2009 (n = 806), GSW in year 2006 (n = 532), PVC in year 2009 (n = 308) and MVC in year 2008 (n = 307). Procedures included n = 1069 laparotomies with 5.43% negative laparotomy rate. Surgery to hollow viscus was performed 1188 times, followed by liver procedures in 269 cases. Neck exploration was performed in n = 127 and thoracotomy in n = 185. The orthopaedic and neurosurgical procedures were not analysed. Average ISS was 16 for blunt trauma and 9 for penetrating trauma, whereas the NISS was 23 and 13 respectively. ISS>25 was noted in 11.7% (n=1274) of the patients and NISS in 22.8% (n = 2480). Actual mortality rate of 11.43% was noted, compared to an ISS predicted mortality of 11.75% and NISS of 16.32%. Burns had the worst mortality of 42.86%, followed by PVC at 21.2%. The least mortality was in stabs at 3.42%.
Conclusion: RSA still experiences an increased burden of disease due to Trauma. Penetrating trauma still dominates the mechanism of injury. Emergency visceral abdominal surgery was required in 9.8% of the cases, neck exploration in 1.16% and chest surgery in 2.2% of the study population. More attention needs to be given to the management of burns patients. A national data base will go a long way to improve trauma outcomes.
FOLEY-CATHETER BALLOON TAMPONADE (FCBT) FOR PENETRATING NECK INJURIES (PNI) AT GROOTE SCHUUR HOSPITAL: AN UPDATE
P Navsaria1,2, M Scriba1,2, S Edu1,2, A Nicol1,2, A A Sayari1,2
1 Groote Schuur Hospital, South Africa
2 University of Cape Town, South Africa
Ethics approval: Approved
Background: A previous study from Groote Schuur Hospital (GSH) highlighted the success of FCBT (PNI). This study is an update highlighting the management trends and outcomes.
Methods: The records of all patients with PNI requiring FCBT for a neck injury presenting to GSH within an 11-month study period were reviewed. Prospectively captured data on the Electronic Trauma Health Record Application (eTHRApp), was retrospectively analysed. Analysed data included demographics, clinical signs on admission, imaging, management, and major outcomes.
Results: Over the 11-month study period, 311 patients with PNI were seen, of which 47 patients (15.1%) required FCBT. All were male; mean age of 28.6 (range 18 - 48) years. Most injuries were caused by stab wounds (91.5%) while four patients (8.5%) suffered gunshot wounds. The majority of catheters (85.1%) were inserted by the referral institution. A total of 14 arterial injuries were identified, of which only one had ongoing active bleeding with haemodynamic compromise requiring immediate surgical intervention without prior imaging. The remaining 46 patients were imaged with computerised tomography angiography (CTA). A total of eight major arterial injuries were found, of which six were surgically repaired; and one carotid injury was stented. A further six minor arterial injuries were identified and managed expectantly. A further four patients required surgery for their neck injuries: two had major venous injuries ligated and two required surgery for aerodigestive injuries. The remaining patients had their catheter successfully removed at 48-72 hours. There was no significant bleeding observed in any of these patients. There was one mortality caused by a large cerebral infarct from a common carotid artery injury.
Conclusion: This series shows an increasing use of FCBT for PNI. Major differences from the previous series include the increased use of CT angiography, and less reliance on formal angiography for diagnostic purposes. FCBT remains a simple, easy-to-use, yet effective technique.
GUNSHOT TIBIA FRACTURES TREATED WITH INTRAMEDULLARY NAILING: A SINGLE CENTRE RETROSPECTIVE REVIEW
N Kruger1, T Hilton1, Karen Wiese2, Case Martin3, Sithombo Maqungo1
1 University of Cape Town, South Africa
2 Worcester Hospital, South Africa
3 University of Texas, United States of America
Ethics approval: Needs to be acquired
Background: Open tibia fractures are notoriously difficult to treat, with a high rate of union problems and infection. Gunshot wound-associated fractures of the tibia compound these issues further by causing extensive bone comminution and soft tissue damage. No universally accepted management protocol exists, but intramedullary (IM) nailing of these injuries is an attractive treatment strategy. It provides stable internal fixation and limits further insult to the soft tissue envelope. It also allows complete access for wound management and early range of movement of the adjacent joints. This study aims to review the results of patients treated with IM nailing for gunshot wound (GSW) tibia fractures to assess whether this is a viable treatment option for this injury.
Methods: A retrospective folder review was performed of all adult patients who sustained a GSW tibia fracture treated with intramedullary nailing between January 2009 and December 2014. Parameters evaluated included time to theatre, time to wound closure, radiographic extent of fracture comminution, anatomical alignment, time to union, and incidence of chronic osteomyelitis.
Results: 22 patients were eligible for inclusion; however, nine were lost to follow-up. The remaining 13 patients achieved union over an average of 26 weeks. Three cases developed osteomyelitis, all of which had radiographic zones of comminution exceeding 120 mm. No cases of malunion were reported and no other significant trends noted.
Conclusion: Treatment of tibial gunshot fractures must be individualised according to both the soft tissue injury and radiographic zone of comminution in order to achieve a favourable outcome. Intramedullary nailing is an effective treatment strategy for low Gustilo-Anderson grade injuries, with minimal complications.
HIV AND PENETRATING ABDOMINAL TRAUMA: DOES HIV INFLUENCE THE OUTCOME?
D McPherson, V Neuhaus, S Edu, A Nicol, N Almgla, P Navsaria
University of Cape Town, South Africa Ethics approval: Approved
Introduction: Human immunodeficiency virus (HIV) infection and trauma are significant contributors to the burden of disease in South Africa. There are conflicting reports about the influence of HIV in outcomes after surgery. In addition, there have been no studies to date that have compared HIV positive and negative patients with penetrating abdominal wounds requiring an explorative laparotomy. The purpose of this study was to determine whether the outcome of hemodynamically stable patients undergoing explorative laparotomy for penetrating abdominal trauma differed in HIV positive versus HIV negative patients.
Methods: This was an observational prospective study from February 2016 to May 2017. All hemodynamically stable patients with penetrating abdominal trauma requiring a laparotomy were included in the study. Outcome parameters were in-hospital death, morbidity (defined as one or more distinct complications during hospitalization), admission to intensive care unit (ICU), relaparotomy within 30 days, and length of stay longer than 30 days. Variables were sought in bi- and multivariate analysis.
Results: A total of 209 patients, 94% male, with a mean age of 29 ± 10 years were analysed. 28 patients (13%) were HIV positive. The two groups were comparable except for race. All patients underwent explorative laparotomy of which 10 (4.8%) laparotomies were negative. There were two (0.96%) deaths, both in the HIV negative group. The complication rate was 34% (n = 72). PATI score was the single independent predictor for complications in multivariate analysis. 29 patients (14%) were admitted to the ICU. A higher PATI, advancing age, and a lower RTS were significant risk factors for ICU admission. After 30 days, 12 patients (5.7%) were still in hospital. PATI was the single independent predictor in multivariate analysis. 24 patients (11%) underwent a second laparotomy and PATI was again the only significant predictor of outcome.
Conclusion: The incidence of HIV in our cohort is 13%; which is similar to the incidence of HIV in the Western Cape of 12%. Our results showed that HIV status was not an independent predictor for morbidity, admission to ICU, relaparotomy, prolonged hospital stay or mortality. The patient's HIV status does not influence their outcomes in penetrating abdominal trauma.
HOW MANY PATIENTS COULD BENEFIT FROM THE INSTALLATION OF A REBOA IN PREHOSPITAL CARE? A RETROSPECTIVE STUDY OF PATIENTS RESCUED BY THE PARIS FIRE BRIGADE
T Oscar1, K Bertho1, E Rozenberg1, N C Roche2, D Jost1, J P Tourtier1
1 Emergency Department - Paris Fire Brigade, France
2 Cardiology department - Begin Military Hospital
Ethics approval: Needs to be acquired
Introduction: The resuscitative endovascular balloon occlusion of the aorta (REBOA) is a technique used primarily in trauma centers to control hemorrhage by placing a retrograde catheter in the artery and inflating a balloon at its tip. This retrospective study is aimed at evaluating the proportion of injured people in Paris, France, who could have benefited from this efficient technique before their hospitalisation, on the scene or during transport.
Methods: The cases were selected based on medical intervention sheets (MIS) filled in by the physician who was in charge of the patient before hospitalisation. Eligibility criteria were: patients over 18 years of age with bleeding of supposedly abdominal and/or pelvic and/or junctional origin, uncontrolled hemorrhagic shock or cardiac arrest with attempted resuscitation.
Results: During the year 2014, 37 patients (28 men) out of a total of 1 159 MIS (3.2 %) were eligible. Median age was 43.5 years (age span 32-58). Death on scene rate was 83.8 % (n = 31) and six patients had a beating heart when they arrived at the hospital. Ten out of the 37 patients had spontaneous circulatory activity. Among them, four people died on the scene or during transport. 36 out of 37 patients were intubated, one benefited from the use of a hemostatic dressing and one benefited from a tourniquet. The median pre-hospitalisation duration was 55 minutes, while other studies have shown that the median duration for placing the endovascular balloon is eight minutes.
Conclusion: REBOA can be seen as an effective non-surgical solution to ensure complete hemostasis during the pre-hospitalisation period. It can be used in extreme conditions by emergency doctors.
IN ACUTE LIMB INJURY, DELAYED PRESENTATION IS THE MAJOR IMPEDANCE: NICVD REVIEW
M M Islam
National Institute of Cardiovascular Diseases, Dhaka, Bangladesh
Ethics approval: Needs to be acquired
Background: Outcome of acute limb ischaemia depends on the timely intervention. In an ischaemic organ or tissue, following revascularisation, a cascade of pathophysiological events often occurs known as Reperfusion Injury. Delayed repurfusion of an acute occlusive limb ischaemia causes local and systemic serious consequences and is the major cause of morbidity and mortality in these patients. Late presentation of acute limb ischaemia was defined as occlusion occurring 72 or more hours after initial menifestation of patient complaint related to the affected ischaemic extremity.
Materials and Method: A retrospective study evaluated time of reporting and management in a consecutive series of 62 patients with ALI between July 2013 to July 2016 in National Institute of Cardiovascular Diseases, Dhaka. ALI was defined as symptoms within two weeks of presentation. Time of presentation, Grades of ischaemia, co-morbidities, morbidities, and mortality were recorded.
Results: During the study period, 62 patients were included, 35 male (56.45%) and 27 female (43.55%). Average age was 63 years ( 30 years-87 years). Four patients (6.45%) reported within six hours of symptom, 10 patients (16.13%) within 24 hours, 20 patients (32.26%) within 72 hours and 28 patients (45.16%) after 72 hours. On admission, 30 patients had grade-III ischaemia, 22 had grade-IIb, and 10 had grade-IIa. 10 patients (16.12%) died and 30 patients (45.16%) had amputation. The risk factors of amputation were grade of ischaemia, extremity (lower limb 45% vs. upper limb), age and co-morbidity.
Conclusion: Late presentation of acute occlusive ischaemia carries high morbidity and mortality. Lack of awareness and negligence of symptoms delay the reporting time to hospital.
INTERPRETATION OF EMERGENCY CT SCANS IN POLYTRAUMA: TRAUMA SURGEON VS RADIOLOGIST
T Hardcastle1,2, P Parag1
1 Univesrity of KwaZulu-Natal, South Africa
2 Inkosi Albert Luthuli Central Hospital, South Africa
Ethics approval: UKZN BREC Ethics approval BE488/15
Introduction: Time is critical in the trauma setting. Emergency CT scans are usually interpreted by the attending doctor and plans to manage the patient are implemented before the formal radiological report is available.
Objectives: To investigate the discrepancy in interpretation of emergency whole body CT scans in trauma patients by the trauma surgeon and radiologist and to determine if the difference in trauma surgeon and radiologist interpretation of emergency trauma CT scans has an impact on patient management.
Method: This prospective observational comparative study, (UKZN BREC Ethics approval BE488/15) was conducted over a six month period (01 April - 30 September 2016) at the Inkosi Albert Luthuli Central Hospital which has a Level 1 trauma department. The study population comprised 62 polytrauma patients who underwent a multiphase whole body CT scans as per the trauma imaging protocol. The trauma surgeons' initial interpretation of the CT scan and radiological report were compared. All CT scans reported by the radiology registrar were reviewed by a consultant radiologist. The time from completion of the CT scan and completion of the radiological report was analysed.
Results: Since the trauma surgeon accompanied the patient to radiology and reviewed the images as soon as the scan was complete, the initial interpretation of the CT was performed within 15-30 minutes. The median time between the CT scan completion and reporting turnaround time was 75 (16-218) minutes. Critical findings were missed by the trauma surgeon in 4.8 % of patients (bronchial transection, abdominal aortic intimal tear and cervical spine fracture) and non-critical/ incidental findings in 14.5%. The trauma surgeon correctly detected and graded visceral injury in all cases.
Conclusion: There is no significant discrepancy in the critical findings interpretation of whole body CT scans in polytrauma patients by the trauma surgeon and radiologist and hence no negative impact on patient management. The turnaround time for the radiology report does not allow for timeous management of the trauma patient.
INTRA-ABDOMINAL VASCULAR INJURY
V Kong
University of KwaZulu-Natal, South Africa
Ethics approval: Needs to be acquired
Background: Intra-abdominal vascular injury (IAVI) is uncommon but continues to be associated with a high mortality, despite technological advances in the past decades.
Methods: A retrospective review was conducted over four-year period at a major trauma centre in South Africa.
Results: 110 patients were included, of which 98 sustained penetrating injuries (43 stab wounds and 55 gunshot wounds).
There were 84 arterial injuries and 69 venous injuries. Arterial injuries were: renal (21), aortic (8), external iliac (7), superior mesenteric (6), inferior mesenteric (6), common iliac (5), splenic (5), hepatic (2), internal iliac (2), miscellaneous arteries (22). Venous injuries were: renal (21), inferior vena cava (17), common iliac (11), external iliac (6), internal iliac (4), superior mesenteric (4), inferior mesenteric (3), portal (2), hepatic (1), and miscellaneous veins (8). 52% required intensive care admission. The overall mortality was 28%. Mortality was 60% for aortic injuries and 47% for inferior vena cava injuries.
Conclusions: The mortality rate for IAVI remains high, despite decades of operative experience in high volume centres. Open operative techniques alone are unlikely to achieve further reduction in mortality and integration of endovascular techniques may provide an alternative strategy to improve the outcome.
KILLING TWO BIRDS WITH ONE STONE: A COMBINATION OF NOVEL DEVICES FOR THE MANAGEMENT OF TRAUMATIC BRAIN INJURY.
H Uchino, N Tamura, K Ninomiya, M Kikukawa, T Fukuoka
Kurashiki Central Hospital Emergency and Critical Care Center, Japan
Ethics approval: Needs to be acquired
Introduction: Adequate ventilation and temperature management are the essential part of neuroprotective strategy to avoid second hit for the patient with traumatic brain injury (TBI). Intellivent-ASV (Hamilton Medical, Switzerland) is fully automated closed-loop ventilation that adjusts ventilation and oxygenation parameters. And coolline catheter with Thermogard system (Asahi Kasei ZOLL Medical, Japan) is an advanced core endovascular cooling system which has been implemented for therapeutic temperature management. We have commenced using these devices for the patients requiring neuroprotective strategy following TBI. The aim of this study is to seek the advantages of these devices during neuroprotective management.
Methods: We conducted a retrospective study comparing the TBI patients managed with Intellivent-ASV and Thermogard (intervention group) from January 2016 to May 2017 and managed with conventional techniques (control group) in 2014 when these devices had not been implemented. Patients under 18 years of age or demised within 24 hours were excluded. Level of PCO2, temperature itself, and the maximum and minimum temperature difference during the neuroprotective period, and the numbers of manual intervention required to control the PCO2 and temperature were assessed.
Results: A total of 15 patients are included. Intervention group had eight patients, five patients used both Intellivent-ASV and Thermogard, two patients used Thermogard only and one patient used Intellivent-ASV only. Control group had seven patients, four patients applied targeted temperature management. The numbers of manual intervention were significantly lower in intervention group using Intellivent-ASV and Thermogard (1.0 [1.0-2.0] vs 5.0 [3.0-7.0]; P=0.001 and .0 [0-1.0] vs 5.0 [3.3-10.5]; P = 0.006). Maximum and minimum temperature difference is also significantly smaller in intervention group (1.0 [0-1.0] vs 2.0 [1.25-2.75]; P = 0.024). However, the level of PCO2 and temperature were not different between groups (39.5 [38.8-40.5] vs 42.0 [40.045.0]; P = 0.073 and 36.0 [36.0-37.0] vs 37.0 [36.3-37.8]; P = 0.164).
Conclusions: Novel devices are feasible or even more efficient when managing TBI patients requiring neuroprotective strategy. The reduced numbers of the manual intervention decrease workload, the risk of human errors, and will save not only the patients but also the doctors and nursing staffs.
LAPAROSCOPY FOR BLUNT ABDOMINAL TRAUMA: ARE WE READY?
K Ninomiya, H Uchino, N Tamura, M Kikukawa, T Fukuoka
Kurashiki Central Hospital Emergency and Critical Care Center, Japan
Ethics approval: Needs to be acquired
Introduction: As experience in laparoscopy for trauma has accumulated, not only diagnostic but therapeutic interventions for patients with abdominal trauma have been advocated. However, the actual role of laparoscopy for the diagnosis and treatment of patients with blunt abdominal trauma (BAT) has remained undefined. We have introduced laparoscopy for BAT with specific indications in our unit since 2014. The aim of this study is to review our experiences in using laparoscopy for BAT patients.
Methods: This is a retrospective observational study conducted at a tertiary referral hospital in Japan from April 2014 to March 2017. All patients sustained BAT requring surgical intervention were included. The indications for laparoscopy were adult, hemodynamically stable, isolated abdominal trauma, and equivocal or negative initial CT finding. We collected data from our electronic medical records.
Results: 53 patients were included. The median age [IQR] was 61 [37-73], 38 (71.7%) patients were male, and the median ISS [IQR] was 24 [15-34]. Laparoscopy was performed in three cases (5.7%). All of them had equivocal CT findings and they all complained abdominal pain. Case 1: An 18 year old male, was involved in motor vehicle collision (MVC). Necrotic ileum with mesenteric injury was found and bowel resection was performed laparoscopically. He discharged on POD6 without complication. Case 2: A 68 year old male, was crushed under the heavy barrel. Perforation of the ileum with localised contamination was found. Conversion to laparotomy with small incision was performed for the resection of the perforated bowel and complete washout. He discharged on POD11 without complication. Case 3: A 41 year old female, was involved in MVC. Exploratory laparoscopy was thought to be negative. However, due to its uncertainty, laparotomy was performed, ended up with negative laparotomy. She suffered surgical site infection and required further management.
Conclusions: Laparoscopy can provide the advantages of minimally invasive surgery for hemodynamically stable patients with BAT when used adequately. However, due to its heterogeneity of patient populations and less frequent incidence, to define the actual indications and to obtain the advanced skills in laparoscopy are key issues to be challenged.
MANAGEMENT OF THORACIC GUNSHOT WOUNDS
A Hattam, M Meijering, S Edu, P Navsaria, A Nicol
Trauma Centre, Groote Schuur Hospital, Cape Town, South Africa
Ethics approval: Approved
Background: Computed tomography angiography (CTA) guided non-operative management remains contentious in patients with gunshot wound (GSW) tracts involving the thorax. The aim of this study was to assess the feasibility and safety of CTA-guided non-operative management in patients with thoracic GSW and associated injuries.
Methodology: A 12-month prospective study was undertaken to examine all patients admitted to a Level-1 trauma centre with a thoracic GSW. Clinically stable patients with isolated thoracic (± extra-thoracic) GSW without indication(s) for immediate (intra-or-extra thoracic) surgery underwent serial clinical and radiological examination, plus selective thoracic ± extra-thoracic CTA. Thoracic GSW patterns were generated for each patient (1. Isolated hemi-thorax, 2. Mediastinal, 3. Trans-Mediastinal, and 4. Thoraco-abdominal) and an injury severity score (ISS) was calculated. Outcome parameters included the need for delayed surgical intervention, hospital length of stay (LOS), and survival. Results are presented as mean ± standard deviation with significance defined as p 0.05.
Results: Of the n = 144 patients admitted with thoracic GSW during the study period, n = 24 required emergency surgery, and n = 117 patients underwent formal radiological examination and non-operative management. 81 patients were discharged without surgery (n = 1 death) (ISS = 22±10), while n = 36 (n = 2 deaths) required delayed surgery (ISS = 31±13). Need for delayed surgery was associated with significantly higher ISS (p 0.05) and a longer hospital LOS (14±14 days) compared to non-operative patients (7±7 days; p 0.05). Overall, mortality for non-operative patients having delayed surgical, or non-operative, management was 8% and 3%, respectively. In contrast, mortality of patients undergoing emergency surgery (ISS = 33±9) was 21% (p 0.05 versus the non-operative cohort). No statistically significant associations were identified between thoracic GSW pattern and need for surgery, or survival.
Conclusion: The management of thoracic GSW without surgical intervention is feasible, with an overall success rate of 70%. Calculated ISS may prove useful in risk stratifying patients with thoracic GSW who may eventually require delayed surgery.
MORTALITIES IN LIVER TRAUMA AT THE JOHANNESBURG TRAUMA UNIT: WHAT CAN WE LEARN?
I M Joubert1,2, M D Oyomno1,2, L Jonas1,2, M Pholosi1,2, S Gyebi1,2, J Goosen1,2
1 Trauma Unit, Charlotte Maxeke Johannesburg Academic Hospital, South Africa
2 University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: Liver Trauma can have devastating results despite optimal care. Multiple factors including physiological derangements and injury severity may impact on outcome. Unpacking the specific factors influencing outcomes in our unit will allow us an opportunity to identify factors that warrant improvement, to optimise future patient care.
Aim: Analyse factors associated with mortality in patients with liver injuries presenting at CMJAH.
Method: Severe Trauma patients (P1), who presented with liver injuries at the Trauma unit were recruited for the study from 01/06/2005 till 30/04/2011. Demographic data, mechanism of injury, injuries sustained, physiological parameters including RTS, ISS, percentage survival based on ISS, and mortality outcomes were all included. Data was entered on an Excel worksheet. Statistica V8 was used as a tool for statistical analysis. P value <0.05 was considered statistically significant.
Findings: A total of 714 patients were recruited for the study with penetrating trauma accounting for 50.6% (n = 361) of study population. Male predominance was 85% 9 (n = 307) of the penetrating and 72% (n = 255) of the blunt group. Blunt trauma had a higher median ISS (29 v/s 17), lower predicted percentage survival (51.5% v/s 98%), lower RTS (4.6 v/s 6.4), higher actual mortality (52.4% v/s 21,6%), higher associated severe chest injuries (50.1% v/s 34.1%), higher associated severe pelvic fractures (16.1% v/s 0%), and a higher associated severe head injury (43.3% v/s 1.3%) than the penetrating injuries. However, blunt trauma had slightly less complex liver injuries (49.6% v/s 51.8%), and less major intra-abdominal vascular injuries (5.38% v/s 21.1%).
Conclusion: Mortality outcomes in blunt liver injuries were poorer than in penetrating injuries. This high mortality in blunt trauma is probably due to the increased associated head, chest and pelvic injuries. Early recognition of associated injuries may impact on mortality.
MORTALITY AND CAUSES OF DEATH IN SWEDISH PATIENTS WITH OPEN TIBIAL FRACTURES - A NATIONWIDE STUDY OF 3 777 PATIENTS
U Tampe, L W Widmer, R J Weiss, K Â Jansson
Department of Molecular Medicine and Surgery, Section of Orthopaedics and Sports Medicine, Karolinska Institutet at Karolinska University Hospital, Stockholm, Sweden
Ethics approval: Needs to be acquired
Background: Open tibial fractures are serious, complicated injuries. Previous work suggested an increased risk of death, however, this has not been studied in large population-based settings. We aimed to describe the mortality after open tibial fractures in Sweden, compare mortality rates with the Swedish population, and determine whether treatment-related or demographic variables were independently associated with death.
Method: We searched the Swedish National Hospital Discharge Register for all patients sustaining an open tibia fracture between 1998 and 2010. We collected the following variables: age, gender, length of stay, mechanism of injury, and treatment rendered. We then cross-referenced the Swedish Cause of Death Register to determine the cause of death, if applicable. We compared mortality in the study population with population-based mortality data from Statistics Sweden, then determined whether variables were independently associated with death using regression analysis.
Results: Of the 3 777 open tibial fractures, 425 (11.3%) patients died. The most common causes of death for elderly patients were cardiovascular and respiratory, whereas, patients aged 15-39 years succumbed to external causes (accidents, suicides or poisoning). Increasing age (OR 25.7, (95% CI 11.8-64.8) p < 0.001), length of hospital stay (HR 1.01, (95% CI 1.009-1.017) p < 0.001), limb amputation (OR 4.8 (95% CI 1.86-11.1) p < 0.001) and cause of the accident were independently associated with an increased mortality.
Conclusion: Patients with open tibial fractures have an increased risk of death compared with the general population. External causes of death are over-represented and indicates a subgroup with a risky behaviour among younger males.
Elderly patients are at risk for cardiovascular and respiratory failure and should be treated with urgency, emphasising the need for specialised geriatric trauma units.
NEGLECTED ANKLE FRACTURES
V Sinevici1,2, S Rose1,2, C Frey1,2
1C H Baragwanath Hospital, South Africa 2 University of Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Every second month we receive a neglected ankle fracture. These fractures are unstable or malunited with talus shift (type B2 and C in Weber-Danis classification and 44B and 44C in AO classification).
There are two main reasons for their neglect: either the fracture was misjudged by the initial attending physician or the patient was not compliant.
Surgical correction is a difficult undertaking in these situations due to tissue contractions and malunited bony fragments. The aim is to achieve intra-operatively anatomical reduction and maintain this reduction.
We present 10 malunited cases. Eight were Weber-Danis type B2 and two were type C. Their initial treatment was plaster of Paris. The referral to our institution was anytime between six weeks and six months after the injury.
The patients were positioned supine with a sand bag under the ipsilateral buttock. Tourniquet was used in all patients. The malunions were taken down through a separate medial and lateral approach. The soft tissues were mobilised until full correction of the talus position was achieved. The talus congruity in the ankle mortise was verified intra-operatively with an image intensifier.
The reduction was maintained with low contact compression plates. We advise for caution in using factory pre-contoured plates which do not buttress sufficiently the joint. The joint cartilage was still in a good condition. We did not have to do primary fusions.
In addition to the internal fixation a below knee full plaster of Paris was applied once the integrity of the skin was assured.
OSTEOSYNTHESIS OF PERIPROSTHETIC FRACTURES AFTER TOTAL HIP AND KNEE ARTHROPLASTY
C Frey, R Greeff
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
The incidence of periprosthetic hip fractures after arthroplasty surgery is rare. Over the passed three years over 1 000 patients underwent hip or knee arthroplasty surgery at our institution. In the same time interval we only admitted 23 (2%) periprosthetic fractures.
All admissions had serious comorbid medical conditions. The ASA physical status classification system was Class 3 with more than one severe systemic disease. The main comorbid risks factors were cardio-pulmonary, electrolytes imbalances and dementia. This delayed time to surgery and prolonged hospital admission. All fracture admissions were related to low impact falls.
Infection was ruled out with baseline bloods and joint aspiration. Intraoperative specimens were routinely sent off. In cases were we were unsure about stability of the implant we had a revision set on stand by.
Of the 23 periprosthetic fracture nine were unstable and needed revision arthroplasty. On the hip we had seven unstable Vancouver Type B and C requiring long stem revision in the knee we had two Rorabeck and Taylor Type 3 requiring revision.
11 periprosthetic fractures were treated with open reduction and internal fixation with an extra medullary locking plate construct with a circlage cable system, one underwent a retrograde intramedullary nai,l and one was treated with a hinged knee brace.
Besides prolonged antibiotics for 72 hours and longer postoperative hospital stay post operative infection risk was high with three superficial and three deep infections.
At our institution we had good results with the new locking plate systems. We advice to have a revision system on stand by in case the implant is loose.
OUTCOMES OF FAILURE OF SELECTIVE NONOPERATIVE MANAGEMENT OF PENETRATING ABDOMINAL TRAUMA
P Navsaria, N Almgla, A Nicol, S Edu, S Sobnach, D McPherson
Groote Schuur Hospital and University of Cape Town, South Africa
Ethics approval: Approved
Background: Selective nonoperative management (NOM) of penetrating abdominal trauma is routinely managed in our trauma center. The purpose of this retrospective observational study is to examine the outcomes of patients who have failed NOM.
Methods: All patients for the period 01 May 2015 -15 June 2016 who presented with a penetrating abdominal injury were prospectively entered into an ethics approved database; Ethrapp and retrospectively reviewed. The patients were categorised into three groups: immediate laparotomy, successful NOM, and failed NOM. Outcomes included postoperative complications, mortality, and length of hospital stay.
Results: A total of 485 patients with penetrating abdominal trauma were managed over the 13 month period. Of these; 219 (45%) were initially selected for NOM and the remaining 266 (55%) patients underwent immediate laparotomy. 26 (12%) failed abdominal observation. Increasing abdominal tenderness and radiological study results were the primary factors used to determine the need for laparotomy in the NOM group. The median delay to laparotomy was 44, 5 (27 - 68) hours. Seven hollow viscus, 13 solid organ, and six diaphragm injuries were found at laparotomy. There were 22 therapeutic, two negative, and one non-therapeutic laparotomy. 90% of the immediate group underwent a therapeutic laparotomy. There was no mortality in the NOM group. Complications are tabulated below and when compared to the immediate group, showed no significant difference (to be presented).
Conclusion: The delayed diagnosis and treatment of failed NOM for penetrating abdominal trauma result in morbidity, mortality, and hospital stay comparable with those who undergo immediate laparotomy.
PAEDIATRIC EYE TRAUMA TREATED AT A TERTIARY HOSPITAL IN CAPE TOWN, SOUTH AFRICA: A 2-YEAR REVIEW
J Jansen van Rensburg1, N Freeman2
1 Tygerberg Hospital, South Africa
2 Red Cross Hospital, South Afica
Ethics approval: Needs to be acquired
Introduction: To assess the epidemiology of paediatric eye trauma treated at Tygerberg Academic Hospital, during a two year period.
Methods: All cases of ocular trauma, excluding corneal abrasions and minor contusions in children less than 16 years old, presenting to the Ophthalmology Department at Tygerberg Academic Hospital between September 2011 and September 2013 were included. All information was obtained retrospectively from medical folders.
Results: 91 cases were identified, with boys being injured 2.5 times more than girls. The average age of trauma was 7.7 years. Numbers were equal for patients from rural referral clinics (51%) and the city (49%). The busiest months were during school holidays (April, July, December), and most trauma occurred at the beginning of each month. Most trauma occurred at home without adult supervision. Blunt trauma occurred in 41% of patients, sharp trauma in 56% and, chemical injuries in 3%. The time delay to get to hospital were equal for rural and city patients, and averaged 2.23 days. The average time delay to surgery was 0.8 days with 87% of patients receiving surgery within 24 hours of being admitted to hospital. 76% of patients required surgery (69 patients), and the most common injuries were corneal lacerations, followed by sclera lacerations and traumatic cataracts. Most sharp trauma was caused by glass, wire, and sticks. Most blunt trauma was caused by stones and BB gun pellets. Left and right eyes were affected equally.
Conclusion: Paediatric eye trauma is prevalent in our unit. It is mostly caused by sharp objects and most frequently involves the cornea, sclera, and lens. Most trauma occurred during school holidays, at home, without adult supervision. Prevention of ocular injuries in children requires a better understanding of the circumstances in which they occur.
PENETRATING CARDIAC INJURIES: A COMPARISON BETWEEN GSW AND STAB INJURIES AT A SINGLE CENTRE IN JOHANNESBURG
C Livhebe, A N Chaane, S R Motilall, S Gyebi, R Jacks, M Morna
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: The higher energy in gunshot injuries (GSW) is likely to result in complex injuries that may result in death at the scene. As a result, fewer GSW to the heart survive to arrive alive at the emergency department, compared to the stab cardiac injuries. Management of all cardiac injuries may be complicated by physiological changes over and above the anatomical injuries sustained. A comparison between these two mechanisms may help us understand these injuries better.
Aim: Evaluate injury patterns and outcomes in patients presenting with cardiac GSW compared to cardiac stab wound at a single Trauma centre.
Method: All penetrating injuries presenting at CMJAH between 01/04/2005 and 30/03/2012. Demographic data, anatomical injuries sustained, physiological scores, haemodynamic status, preferred surgical incision, surgical findings, outcomes, and post-mortem findings were noted. Data was recorded on an Excel spreadsheet, and Statistica V8 was used as a tool for statistical analysis. P value <0.05 was considered statistically significant.
Results: 86 (n = 86) patients were recruited for the study. GSW cardiac injuries were in 11 patients all of whom were male. Only nine of the 75 stab injuries were in female patients. Median age was 29.5 years in GSW compared to 27.5 years, and the median ISS of 29 v/s 25 in stab injuries. 45% of GSW were unstable on arrival compared to 31% of stab wounds. Emergency room thoracotomy was required in about a third in each group due to worsening haemodynamic status. Sternotomy was the most common incision in theatre for stab injuries. Right and left ventricles were commonly involved injuries in both mechanisms. The left atrium was the least involved chamber. Mortality rate from GSW were double those in stab injuries.
Conclusion: Cardiac stab injuries are seen more frequently than GSW. Overall mortality was high, with GSW mortality rate double that of stab injuries.
PHYSIOLOGY CHARACTERISATION AND OUTCOMES OF PATIENTS AFTER EMERGENCY ROOM THORACOTOMY: A RETROSPECTIVE REVIEW
B M Torres, S Motilall, J Goosen, M S Moeng
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Background: An Emergency Room Thoracotomy (ERT) is a resource intensive, high-risk procedure where rapid decision-making is essential. Identification of the group of patients that could achieve the best outcome after an ERT will avoid futile use.
Methods: Retrospective review of data from patients who underwent ERT at a Level 1 Academic Trauma Center, between 1st February 2005 and 31st December 2010.
Results: During the study period 13,279 major trauma cases were treated. 86 (0. 65 %) patients underwent ERT. The overall mortality was high (80.2%), but patients with penetrating chest trauma had better survival rates (32.6%) compared to those with combined thoraco-abdominal or sub-diaphragmatic trauma, irrespective of mechanism. The majority of patients exhibited severe metabolic and physiological derangement at the time when the ERT was performed.
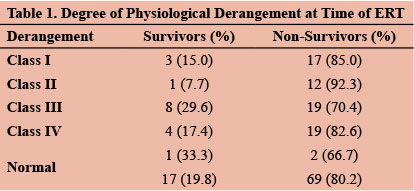
Conclusions: The results of our series seems to support the idea that ERT should be directed at patients with a potential cardiac or pulmonary injury to achieve the best possible outcome.
PHYSIOTHERAPY MANAGEMENT OF PATIENTS WITH MAJOR CHEST WALL TRAUMA: A PILOT SURVEY
H Van Aswegen1, J Reeve2, M F Olsen3, R Parker4, L Beach5
1 Physiotherapy, Faculty of Health Sciences, University of the Witwatersrand, South Africa,
2 Physiotherapy, Auckland University of Technology, New Zealand
3 Physical Therapy, Sahlgrenska University Hospital, Sweden
4 Anaesthesia and Perioperative Medicine, University of Cape Town, South Africa
5 Physiotherapy, The Royal Melbourne Hospital, Australia
Ethics approval: Needs to be acquired
Introduction: The incidence of traumatic injury increases worldwide annually. Thoracic injuries are associated with increased risk for morbidity and mortality. Evidence supporting the role of physiotherapy in the management of patients with chest wall trauma is scant. The aim was to determine feasibility of a survey to describe current physiotherapy practice in the management of adult patients with major chest wall trauma.
Methods: A survey questionnaire was designed and content validated. It was distributed electronically to senior physiotherapists in selected trauma centres in each of the five regions represented by the World Confederation for Physical Therapy. A sample of convenience was used for this pilot survey.
Results: 93% response rate (n = 14/15) was achieved. 50% (n = 7) indicated that they had a dedicated trauma physiotherapist in their hospital. Interventions frequently performed to manage patients' respiratory problems included early mobilisation (100%), positioning for V/Q matching (93%), deep breathing exercises (93%), and active coughing (93%). Interventions never performed included mechanical insufflation-exsufflation (57%), intermittent positive pressure breathing (57%), and ventilator hyperinflation (50%). Interventions frequently used for management of musculoskeletal system were sitting out of bed (100%), early mobilisation (100%), shoulder (86%), and trunk range of motion exercises (71%). Some respondents (43%) never performed cycling on a stationary bicycle with their patients. Responses highlighted ambiguity in some survey questions.
Conclusion: Initial results indicate that early mobilisation activities are mostly used to manage patients with major chest wall trauma which is in line with evidence from the critical care and thoracic surgery literature. The more complex or specific the intervention, the less well utilised these appear to be. Further content validation of survey questions is needed before the survey is distributed to more major trauma centres worldwide.
PNEUMOMEDIASTINUM AND PNEUMOPERICARDIUM AFTER BLUNT TRAUMA
T Hardcastle1,2, D J J Muckart1,2, D L Skinner1,3
1 University of KwaZulu-Natal, South Africa
2 Inkosi Albert Luthuli Central Hospital, South Africa
3 King Edward VIII Hospital, South Africa
Ethics approval: Needs to be acquired
Introduction: Pneumomediastinum may arise from injury to air filled structures within the head and neck, the thorax, or abdomen.
Aim: Review the incidence and consequences of pneumomediastinum and pneumopericardium in patients with blunt trauma admitted to the Trauma ICU at Inkosi Albert Luthuli Central Hospital (IALCH).
Methods: Retrospective review of patients treated between April 2007 and March 2014 using the prospective UKZN-BREC approved (BE207-09) Trauma Registry, including all patients who had undergone computed tomographic imaging. Data collection included age, sex, mechanism of injury, and Injury Severity Score (ISS). Specific injury patterns such as isolated thoracic trauma, flail chest, bilateral injury and the presence of a haemothorax or pneumothorax were assessed for association.
Results: 389 patients formed the study cohort of whom 30 (7.7%) were identified as having pneumomediastinum and/or pneumopericardium. Of these 30 patients pneumomediastinum was identified in 23 (76.7%), combined pneumomediastinum and pneumopericardium in six (20%), and one patient (3.3%) had isolated pneumopericardium. Ages ranged from 2 - 84 years with a mean of 30.1 (SD = 16 95% CI 28.5 - 31.7) and median age of 30 years (IQR = 19 - 40). The median ISS for the entire cohort was 32 (IQR = 24 - 41). Only flail chest was associated significantly with pneumomediastinum or pneumopericardium. Mortality rates were almost identical between the groups. No patient underwent either oesophagoscopy or bronchoscopy for investigation of pneumomediastinum and all deaths were unrelated to a missed injury of the aerodigestive tract.
Conclusions: Our data confirm that the presence of pneumomediastinum or pneumopericardium following blunt thoracic trauma is an incidental benign finding. Increased injury severity in the form of a flail chest is associated with a significant increase in the presence of free gas within the mediastinum. In the absence of complications, no obvious injury to the intrathoracic aerodigestive tract on CT scanning, and no difference in mortality a conservative investigation and management policy is warranted.
PRE-HOSPITAL CERVICAL COLLARS -WHO NEEDS IT?
A Dube1, E Sithole2, M P D Gundani3
'Department of Emergency Medical Services, Emergency Medical Care, Kwekwe
2Department of Medicine, Prestige Clinic; Twin Towers; Bulawayo, Zimbabwe
Department of Sports Science and Coaching, National University of Science and Technology, Bulawayo, Zimbabwe
Introduction: Cervical collars had been used in EMS since in 1960s to date. Cervical spine immobilisation devices are effective despite resulting trauma patient morbidity. The suitability of applying a cervical collar at the scene of an accident and the time at which the patient should be removed from it in the hospital remain questionable. Currently, there is a growing evidence and opinion against the use of collars hence the gap between pre-hospital and hospital researches result may lead to improper handling of trauma patients. Therefore this paper aims at clarifying (1) the purpose of cervical collar in EMS (2) the alleged fear of use of cervical collars by specialist surgeons.
Methods: This is a retrospective study.
Results: The EMS currently immobilise and rescue most if not all patients suffering from seizures, simple falls, minimal-energy motor vehicle collisions to severe trauma with C-collar from the scene of an accident to hospitals. EMTs' syllabus emphasise on proper application of spinal immobilisation and little on determining which trauma patients might need spinal immobilisation or not.
Hospital studies urge that C-spine immobilisation particularly application of rigid C-collars is not a good practice basing on that they: (1) interfere with airway management; (2) increase intracranial pressure; (3) are often tight enough on the neck to restrict venous drainage of the head through the jugular veins; (4) venous outflow is restricted despite arterial blood flowing freely into the cranial vault resulting in increased intracranial pressure; (5) increase spinal motion in high C-spine injuries; in most catastrophic spinal injuries which involve the first (C1) through the fourth (C4) cervical vertebra and atlanto-occipital joint; (6) cause separation of C1 from C2 by stretching the high spinal cord; and (7) develop pain, causing discomfort, tenderness in their C-spine and tissue pressure sores.
Conclusion: Penetrating trauma (head gunshot wound patient/terrorist bombing) patients and children, despite injury severity, do not need C-collar whilst it's questionable for conscious patients whether to immobilise or not. EMS do not use diagnostic imaging for assessment compared to hospital-based care personnel, therefore there is need for reducing trauma patient prior and after effects of their scope of practice.
PRIORITY ONE (P1) GUNSHOT INJURY TRENDS AT JOHANNESBURG TRAUMA UNIT: GOOD NEWS AT LAST?
I M Joubert, S R Motilall, A N Chaane, S Gyebi, K D Boffard, J Goosen
University of the Witwatersrand, South Africa Ethics approval: Needs to be acquired
Introduction: Trauma remains a major challenge to the South African health system. Gunshot injuries (GSW) may cause devastating injuries, leading to significant morbidity and mortality. Implementation of gun control measures has been met with scepticism. The anecdotal forensic data in Johannesburg, suggest that the death related to GSW are decreasing in the past few years.
Aim: Study trends in P1 patients presenting with gunshot injuries to the CMJAH in the past eight years.
Methods: All P1 GSW patients presenting at the CMJAH
from 01/01/2005 till 31/12/2012 were recruited. Retrospective analysis of prospectively collected data was performed. Number of GS injuries per year, were collected to check the trend over the years. Demographics, physiological score, and outcomes were recorded on a spread sheet. Statistica V8 was used as a tool for statistical analysis. P value <0.05 was considered statistically significant.
Results: A total of 2 963 GSW cases were identified. Largest number of GSW were noted in 2006 (n = 524) and the lowest number in 2011 (n = 230). The 21-45year group was the most affected age group. Average ISS was 25 and NISS was 42, with predicted survival rates of 62% based on ISS and 49% on NISS. The overall mortality in GSW was 10.7% with the worst mortality in 2006 at 14.1% and the best mortality in 2012 at 4.7%. There was a general decline in the number of GSW from 2005 till 2012.
Conclusion: GSW injuries seen at CMJAH have declined in the past few years. It is still the potentially economically viable age group that was most affected. The mortality rate was best in 2012. This decline is overall good news tending to favour implementation of gun control measures. More efforts are still required to further lower this trauma load.
PROCALCITONIN AS A MARKER OF SEPSIS IN BURNS PATIENTS
D L Wineberg, D Kruger, R Moore
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: Patients with burn wounds are at high risk of infection. Since sepsis contributes significantly to morbidity and mortality, and early diagnosis is essential. Procalcitonin (PCT) is a biomarker released in response to inflammation and specifically bacterial infection. It may therefore be a useful marker of sepsis in burns.
Aim: To describe the demographics of public and private burns units in Johannesburg, to assess risk factors for bacterial infection, and to correlate PCT with other septic markers to assess its value as a marker of sepsis.
Methods: All adult patients admitted to two Burns Intensive Care Units in Johannesburg were included in a retrospective data review. Data from the preceding three years related to demographics and sepsis were collated.
Results: Records of 180 patients were reviewed. Young black males are most commonly admitted with no significant difference between the public and private sector. The most significant risk factor for sepsis is percentage total body surface area burned (p = 0.0119). Significantly more infections occur in public sector patients with the public sector treating a greater percentage of patients with more severe burns (92.9 vs. 57.9 p = 0.0014). A rise in PCT is a significant marker for bacterial infection early after a burn (p = 0.0304) but not after day eight. PCT shows correlation with CRP as a marker for sepsis, but not with other septic markers.
Discussion: There is progressive loss of the skin's protective layer as the total body surface area involved in the burn increases, resulting in higher rates of sepsis in these patients. This accounts for the increased number of infections in patients in the public sector, as the admission criteria to the Burns Intensive Care Unit are more stringent in this facility, generally admitting patients with burns of more than 20% due to resource constraints. Burn injuries commonly affects the poor who do not have access to private healthcare. The demographic similarity between public and private sector can be attributed to the fact that the private-sector facility is the service provider to some of the mines and a number of the patients admitted are mineworkers with work related injuries. The pathogens cultured from the septic patients are almost identical between both facilities, despite differences in infection control measures. Empiric antibiotic therapy should therefore target these bacteria. There is a significant correlation between an elevated PCT and a positive blood on day four after injury. However, the range of PCT is too wide to define an accurate value of significance. This correlation becomes insignificant a few days after the injury, limiting its value. While PCT shows some correlation with C-Reactive Protein (CRP), there is insufficient data to definitively confirm this correlation and therefore PCT cannot replace CRP as a marker of sepsis. There is, however, no correlation with the other markers included in the American Burns Association consensus and this therefore questions the value of PCT as a marker of sepsis.
Conclusion: While there is some evidence to suggest that PCT may be useful as an adjunct marker of infection in burns patient, this evidence is limited and insufficient to change the current clinical guideline.
QUANTITATIVE FIT ANALYSIS OF ACROMION AND CLAVICLE PLATES IN PLANNING ACROMION OSTEOSYNTHESIS USING ANATOMICAL 3D MODEL RECONSTRUCTIONS
J Charilaou1, S Roche1, S Sivarasu1, R Dey1, R van Staden2, S Maqungo1
1 Groote Schuur Hospital, South Africa
2 TBH
Ethics approval: Needs to be acquired
Background: Scapula fractures are challenging to treat surgically. Bony anatomy, uncommonly used approaches, implant limitations and morphological variance of fracture patterns may lead to difficulty achieving favorable outcomes. Three-dimensional (3D) models can help with a better understanding of fracture patterns and reduction maneuvers required to achieve anatomical congruence.
Methods: We identified 41 patients with scapula fractures on Computed Tomogram (CT) scans from 2012 to 2016. Only blunt trauma as mechanism of injury was included. Scapulae with acromion fractures (n = 15) were converted to real size 3D models using Materialise Mimics. Three categories of fit between plate and model interface was used as a grading system. A quantitative fit analysis of the implants on the reconstructed 3D models was performed. Two separate assessments of each acromion were performed by five different observers.
Results: An inter-observer Intraclass Correlation Coefficient (ICC) of 0,95 was obtained. Clavicle plates had the best overall anatomical fit (n = 13, 86.7%). The 6-hole anterior clavicle plate had the highest cumulative grading (23.2). The 3D models were adequate and anatomically representative.
Conclusion: There is a need for a more anatomical and versatile plating system. Clavicle plates are alternatives to conventional acromion plates. Simulating fracture fixation using 3D models is a reliable preoperative planning tool.
SCREENING FOR AN OCCULT PENETRATING CARDIAC INJURY USING TRANSOESOPHAGEAL ECHCARDIOGRAPHY (TOE): A PROSPECTIVE STUDY
A J Nicol, K Steur, R Bent, A Myburgh, G Sudwarts, F Roodt
University of Cape Town, South Africa
Ethics approval: Approved.
Background: 30% of patients of with a cardiac injury will present with a penetrating chest wound and be haemodynamically stable, the so-called "occult cardiac injury". Current international practice is to screen for occult cardiac injuries using ultrasound (US) of the pericardial sac. If the US confirms the presence of fluid then the patient undergoes a subxiphoid pericardial window (SPW) under general anaesthetic. In our experience US results in a large number of false positives and unneccessary operations. The aim of this study was to determine the accuracy of US for screening and whether transoesophageal echocardiography (TOE) may aid in the diagnosis and prevent unnecessary SPW.
Methods: Prospective study on all haemodynamically stable patients over 28-months with stab wound to the chest in the cardiac zone. Routine work-up comprised a CXR, ECG and an ultrasound. All patients with a positive US underwent a TOE prior to the performance of a SPW. The SPW was considered to be positive if there was blood in the pericardial sac.
Results: 142 patients underwent a SPW over a period of 28 months with a median age of 29 (range 18-59) years. The sensitivity of US for detecting a haemopericardium was 95% but there were 96 false positives. A total of 51 patients
had a TOE prior to the SPW; TOE had a sensitivity of 93%,
specificity of 43%, and a positive predictive value of 38% for detecting a haemopericardium. There were 21 false positives and no false negatives with TOE.
Conclusion: TOE has a very high sensitivity for identifying a haemopericardium, but as with US, there is a problem with false positives. If no pericardial effusion is foundon TOE then the SPW can be avoided. This intervention will decrease the number of unneccessary SPWs.
SCREENING OF THE BABIES STRESS, HEALTH, AND DEVELOPMENT IN PRESCOLAR CONSULTATION AT THE HOSPITAL CENTER OF MONT-AMBA IN KINSHASA
K M John1,2, D Okitundu1,2, M T Sombo1,2, B Ntambwe1,2
1 Département de Neurologie, Unité de Neuropsychologie, Centre Neuro-Psycho-Pathologique de l'Université de Kinshasa, Democratic Republico of the Congo
2 Faculté de Médecine de l'Université de Lubumbashi, Democratic Republico of the Congo
Ethics approval: Needs to be acquired
Background: Stress in pre-school infants is not considered in the Congolese care system. However, its negative role is well known in the health, development, and care of children.
Goal: To screen for stress, and describe its relationship with aspects of the child's health and psychosocial development.
Method: A cross-sectional study was carried out with 30 babies in pre-school consultation at the Mont Amba Hospital Center for a period of three months in 2016. Interest variables were baby stress assessed by the baby distress alarm scale (ADBB). The health status of the child perceived by the mother and the feeding, emotional and social behavior of the baby reported by the mother and the psychomotor development evaluated at the Gensini-Gavito scale. Data wwas collected using a standard protocol and anthropometric parameters were measured for each child. SPSS 20.0 was used to analyse the data.
Results: The age of the children of the children was 8 ± 0.54 months, there were 57.7% of boys 43,3% of the girls. Children were stressed in 30% of cases, 50% had a mild acute, and 40% had a psychomotor developmental quotient, 100 they were described aggressive towards other babies in 23% of cases. The psychomotor development quotient 100 was more associated with overall stress behaviour.
The overall behaviour to reduce body activity (66.7% and p = 0.006) and the relationship of the child to the provider (63.6% and p = 0.052).
The aggressiveness of the baby to other babies was more reported in stressed babies (55, 6% and p = 0.014).
Conclusion: The results of this study tries to demonstrate the link between the behaviour of stress in the baby and, the disruption of his health and his development.
These results can be used in maternal and child health through validation by previous studies.
SPECTRUM OF INTENTIONAL INJURIES IN THE JUVENILE POPULATION TREATED AT AN A LEVEL ONE TRAUMA CENTRE: A SOUTH AFRICAN PERSPECTIVE
M Meijering, S Edu, P Navsaria, H Morad, A Nicol, S Sobnach
University of Cape Town, South Africa
Ethics approval: Approved
Background: South Africa has one of the most violent societies worldwide. The national homicide rate is 34 per 100 000; young males form the majority of this cohort. Comprehensive injury surveillance in low and middle income countries is limited and there is paucity of data describing the epidemiology and outcomes of intentional injuries within the juvenile population. The aim of this study is to describe and analyse the pattern of intentional injuries seen in juvenile patients presenting to a Level 1 trauma centre in South Africa.
Materials & Methods: Ethical approval was obtained for this study. The Electronic Trauma Health Registry (eTHR) Application of the Trauma Centre at Groote Schuur Hospital in Cape Town was interrogated over an 18-month period (April 2014-December 2016) for all patients (aged 15 - 19 years, WHO definition for Juvenile Age Group) treated for non-accidental trauma. The data was then analysed using descriptive statistics.
Results: Over the study period, 2 903 juvenile patients were admitted to the trauma centre. Intentional injuries (n = 1 397, 48.1%) accounted for nearly half of the study cohort. Usable data for this study from eTHR was available for 1 295 patients. Within this cohort 210 (16, 2%) patients claimed to be a victim of gang-related violence. Penetrating injuries were seen in 878 (67, 8%) patients, of whom 401 (45, 7%) sustained knife injuries and 329 patients (37, 5%) sustained gunshot wounds. The most affected body region was the head (n = 388, 30%), followed by the thorax (n = 311, 24%). Permanent disability resulting directly from injury was seen in five cases 1% (n = 66), and the overall mortality was one, 2% (n = 16).
Conclusion: Intentional injuries are common within the juvenile population group in Cape Town. Penetrating injuries and gang-related activities account for a large subset of these patients. Whilst the overall mortality is only 1%, the permanent disability rate is also 1% and is likely to have significant public health and economic ramifications for the South African health care system in the future.
THE EPIDEMIOLOGY AND COST OF YOUTH INTERPERSONAL VIOLENCE AT LOS ANGELES COUNTY HOSPITAL-UNIVERSITY OF SOUTHERN CALIFORNIA
C Foran, D Clark, N Brown, K Inaba, M Schellenberg, D Demetriades
Los Angeles County Hospital- University of Southern California, South Africa
Ethics approval: Needs to be acquired
Objectives: To evaluate the epidemiology, cost, and mortality data of youth interpersonal violence victims presenting to Los Angeles County-USC Medical Center (LAC-USC) to inform the design of a hospital-based violence intervention program.
Methods: This is a retrospective study of 12 549 trauma admissions of youth patients aged 10-30 presenting to an urban, Level 1 trauma center, as the victims of gunshot, stabbing, or assault between the years 1998-2015. Data is collected from the LAC-USC Trauma Database. Logistic regression was conducted to compare patient mortality across demographic characteristics, and p-values 0.05 were considered significant. Among recidivists, only the initial trauma admission was included in the analyses.
Results: The overall crude mortality rate is 8%. When evaluating all admissions between 1998 and 2015, we observed meaningful differences in mortality rate by sex (9% in males vs. 5% in females, p 0.001), race/ethnicity (5% among non-Hispanic white patients vs. 9% among Hispanic patients, p = 0.001), and year of admission (6% in 2010-2015 vs. 10% in 1998-2003, p 0.001). When considering the most recent data (2010-2015), we observed a disparity in mortality between insured and uninsured patients (3% vs. 10%, p 0.001) and meaningful differences in mortality between gunshot victims and victims of assaults and stabbings (13%, 0.3%, and 2%, respectively, p 0.001). A total hospital charge of $393,784,465 was calculated to treat these patients from 1998-2015. The majority of this cost (71%) went to treating gunshot wound victims. 10 zip codes were isolated as having this highest volume of victims of interpersonal violence from 2010-2015. Males make up 92% of admissions. Hispanic patients make up the highest percentage (74%) of admissions in our catchment area when compared to other ethnicities.
Conclusion: LAC-USC continues to treat a high volume of youth interpersonal violence victims at great human and financial cost. While the overall mortality rate is decreasing due to improve trauma care, the mortality rate of gunshot wound victims remains high. Based on the results of this study, further studies must be performed to assess the disparities in mortality for gunshot wound victims, uninsured patients, and Hispanic patients to best inform a hospital based violence intervention programme.
THE INCIDENCE OF VITAMIN D DEFICIENCY IN PATIENTS WITH AN ACUTE TIBIA FRACTURE
I Rhoma, M Mosfeldt, M Held, S Maqungo, G McCalloum, M Laubscher
Ethics approval: Needs to be acquired
Background: Vitamin D is appreciated for its role in bone metabolism. Reports suggest 25% to 50% of patients commonly encountered in clinical practice are deficient in vitamin D, although the incidence in our fracture population is not known. Vitamin D deficiency is thought to play a role in the development of non-unions, but the indications for supplementation in acute fractures are not clear. The primary objective of this study was to determine the incidence of Vitamin D deficiency in a population of tibia fractures.
Methods: We conducted a prospective cohort study at Groote Schuur Hospital, enrolling all adult patients presenting with acute, high energy, extra-articular tibia fractures. Intra-articular and fragility fractures were excluded.
Results: Between May 2016 and February 2017, 36 patients were offered vitamin D testing. Ten patients were excluded due to refusing testing or inadequate blood sampling. 20 (76.9%) patients were males and four (15.38%) females.
19 (73%) patients were isolated injury; seven (7.9%) patients were polytraumatised patients, 16 (16.53%) patients sustained closed fractures; and ten (38.4%) patients had open injuries.
20 (76.9%) patients were vitamin D deficient, five (19.2%) patients were vitamin D insufficient, and one (3.8%) patient was vitamin D sufficient.
Conclusions: We found a very high incidence of Vitamin D insufficiency and deficiency in our study group. Further studies are needed to investigate the incidence in our general population and explore the role of Vitamin D supplementation in fracture union.
THE INFLUENCE OF DIFFERENT CONNECTING ROD CONFIGURATIONS ON THE STABILITY OF THE ILIZAROV FRAME: A BIOMECHANICAL STUDY
G Thiart, C Herbert, S Sivarasu, S Maqungo, S Roche, M Laubscher
University of Cape Town, South Africa
Ethics approval: Needs to be acquired
Background: The Ilizarov external fixator (IEF) is frequently used in trauma and elective orthopaedics. Many of its biomechanical variables (ring size; wire diameter; wire number; half pins versus wires; etc.) and their influence on stability and stiffness have been investigated. There is however a paucity in the literature regarding the influence of the connecting rod numbers and configurations between the rings on IEF stability.
Objectives: Primarily to compare the stability between four and three rod IEF configurations. Secondarily to assess the difference in stability between symmetrical and asymmetrical spacing of the IEF rods.
Methods: A custom jig was designed to facilitate mounting of a basic two ring IEF in a hydraulic press. Controlled centre and off centre (thus simulated bending) axial loading was then applied across the frame. The configurations were loaded up to 4 000 Newtons. The frame deformation was plotted and the data was then analysed and interpreted.
Results: Negligible differences were observed between different four and three rod configurations as long as the applied force at the loading point (LP) was within the area of support (AOS) created by the rods. The different four rod constructs were always more stable than the three rod constructs during bending.
Conclusions: There is comparable stiffness between a four rod and a three rod IEF construct as long as the loading point (LP) is within the area of support (AOS) created by the rods. A four rod IEF is stiffer than a three rod IEF in bending.
THE MANAGEMENT OF ACUTE LATERAL ANKLE SPRAINS: A SURVEY OF SOUTH AFRICAN SURGEONS AND BEST EVIDENCE AVAILABLE
S Wever, G M McCollum
South African Orthopaedic Association, South Africa
Ethics approval: Needs to be acquired
Introduction: Ankle sprains remain the single most frequent injury in modern sports, with increasing evidence that it is not as innocuous as previously thought. Conservative treatment options include various forms of immobilisation such as casts, moonboots and stirrup braces, followed by a rehabilitation period involving different modalities. Despite clinical evidence there seems to be a divergence between research and practice with an increase in acute surgical repair especially with regards to professional athletes.
Design: Descriptive cross-sectional survey analysis.
Aim of the study: To assess the approach on management of acute ankle sprains by orthopaedic surgeons in South Africa.
Methods: A two part study. Firstly, a questionnaire posed to participating orthopaedic surgeons, consisting of eight treatment options for a Grade 3 lateral ankle sprain in a non-professional athlete. Secondly, a literature review to establish the current best practice concerning ankle sprains.
Results: 129 total responses were received out of 719 that were sent out. 24 (19%) offered acute surgical repair. 49 (38%) recommended a six week period of immobilisation in either cast or moonboot. 55 (43%) offered a shorter period of immobilisation. Only 39 (30%) of orthopaedic surgeons chose a short period of immobilisation followed by functional rehabilitation in accordance with the current best evidence available, based on the literature review done.
Conclusion: Despite good clinical evidence there seem to be a lack of consensus in the management of Grade 3 lateral ankle sprains.
THE NECK OF FEMUR FRACTURE IN THE ELDERLY. INTERNAL FIXATION OR ARTHROPLASTY?
C Frey1,2, R Greeff12
Chris Hani Baragwanath Hospital, South Africa University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
The dilemma an Orthopaedic Surgeon is faced with a neck of femur fracture is whether he should advise for internal fixation or replacement. Fixation with open reduction and internal fixation may be the shorter operation with less stress for the patient, but may have adverse outcomes. Non union and failure of fixation are not uncommon. While the replacement is the longer surgery, but may have a more favourable outcome.
Over the past two years we admitted 96 neck of femur fractures (NOF). 58 were female and 38 male. The average age was 66.9 years (range 54 to 92 years). BMI ranged between 17 and 48 with an average of 29.7. The majority, 51 patients, were "walk in's". 45 were referrals from our satellite hospitals. The main referral reason was anesthetic risk due to comorbid medical conditions.
Time to survey ranged from four days to two weeks depending on the comorbid medical conditions and the time of the referral. During that time we optimised electrolyte imbalances and cardiopulmonary function. All patients needed a physician and anaesthetic consult. All required a preoperative cardiac echo. Two required pace maker insertion prior to surgery.
All fractures were AOT classification Type 31B, extra-articular, sub-capital or trans-cervical neck fractures. We had no undisplayed or mildly displaced Garden Type 1 or 2 fractures. Six were Garden Type 3 the rest was Garden Type 4.
11 had a failed internal fixation and were referred for revision surgery. All underwent arthroplasty surgery.
When possible, we prefer spinal anaesthesia. All but 21 patients underwent a spinal anaesthesia. We used two cemented Thompsons implants, 42 uncemented bipolar stems, and 52 uncemented total hip replacements.
During this period we did not find suitable patients for ORIF. The aim of the fracture treatment is to return the patient as quick as possible to their pre-fracture level of function. In our hands this was best achieved with arthroplasty surgery.
THE ROLE OF A REPEATED ABDOMINAL SONOGRAPHY IN BLUNT INJURY
S H Israelit, B Monzon, J Goosen, M S Moeng
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: FAST may enhance clinical examination of stable blunt trauma patients.
Aim: Investigate the accuracy for repeated-delayed FAST, in the subgroup of stable blunt trauma victims, with primary normal FAST.
Methods: Retrospective review of prospectively inserted data (Feb 2005 - Feb 2009), of 482 patients, who sustained fall from a height. Data collected: demographics, GCS, HR, RR, sBP, RTSc, AIS, FAST, repeated-FAST, CT scans and diagnosed injuries.
Results: n = 156 stable patients with GCS 15. Mean age 30 years. Average admission HR, sBP and RR, were 81-b/ min, 127-mmHg and 20-/min respectively. Average RTSc and AIS were seven and five respectively.
90 patients underwent FAST during resuscitation, 80 patients had a negative FAST. Ten patients with positive FAST underwent a CT scan (negative for two patients).
Nine patients underwent repeated-FAST within four to six hours (eight negative) - no further investigation. One patient with positive repeat-FAST had grade-II liver laceration on CT scan. Predictive parameters for repeat FAST: Sensitivity = 78%, Specificity = 99%, PPV = 88%, NPV = 98%, Overall Accuracy = 97%.
Conclusions: FAST is a reliable screening tool for stable blunt injury. Negative repeat FAST is sufficient to rule out significant abdominal injury.
THE USE OF XBOX KINECT™ IN THE PAEDIATRIC BURNS UNIT AT CHRIS HANI BARAGWANATH ACADEMIC HOSPITAL
E Lozano, J Potterton
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Background: Burns are a significant cause of paediatric injuries, particularly in low and middle-income countries, where more than 90% of burn-related paediatric deaths occur. Physiotherapy is an essential, sometimes painful, component of burn rehabilitation therapy. The popularity of the video game use in burns rehabilitation has grown because, in addition to facilitating ROM in an effort to prevent joint contracture formation, the virtual imaging characteristics of these games provides additional benefit of distraction from pain. Video games provide a more efficient, effective and enjoyable method training, and are a helpful adjunct to rehabilitation.
Aim: To investigate the effect of using the Xbox Kinect™ on discharge outcomes of children in the PBU at CHBAH.
Methods: This quasi-experimental time series study consisted of two groups. The control group all received standard physiotherapy rehabilitation and the experimental group received additional Xbox Kinect™. Outcome measures were ROM, ASK©participation and a modified Wong-Baker FACES® enjoyment rating scale.
Results: 70 children were recruited into the study of which the data for 66 were analysed. The majority burns were as a result of hot water attributing to more than 50% of admissions, followed by flame burns (30%), and electrical burns (12%).
The Xbox Kinect™ was shown to be significant in achieving higher active ROM at discharge (p 0.01) and at follow up (p 0.01).We found that TBSA % was a predictor of ASK©p scores (p 0.01). Fun and enjoyment (p 0.01) was found to be significant in this study.
Conclusion: The use of the Xbox Kinect™ as seen in this study has proven to be beneficial and a useful adjunct to burns rehabilitation within in the paediatric burns population.
THIGH COMPARTMENT SYNDROME AND COMPARTMENT PRESSURE ASSESSMENT IN A PATIENT WITH A FEMORAL SHAFT FRACTURE
J du Plessis
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Acute compartment syndrome results from a rise in the pressure within a fixed osteofascial compartment, resulting is a decrease in capillary perfusion and tissue ischaemia with the most common underlying cause being a result of trauma. Thigh compartment syndrome is a rare event comprising just 3% of all compartment syndromes and thus needs a high index of suspicion for early diagnosis and management. Although the diagnosis is predominantly clinical, measurement of compartment pressures may aid in the diagnosis when clinical findings are equivocal and suspicion remains high.
I present a case of acute compartment syndrome of the thigh following a low velocity firearm injury with associated femoral shaft fracture. The patient presented with a tense swelling of the thigh but otherwise seemed comfortable at rest, only having pain if being examined. Due to clinical suspicion the patient was booked for fixation and fasciotomy. Compartment pressures were measured prior to anaesthesia using a standard arterial line and a 16G IV cannula. The measurements of all three compartments confirmed the raised intracompartmental pressures which were within 30 mmHg of the diastolic blood pressure, thus confirming the need for fasciotomy of all three compartments.
Intramedullary nailing along with medial and lateral fasciotomies were done releasing all three thigh compartments. The patient went for relook and delayed primary wound closure after three days and was discharged with no neurological or functional deficits.
This case highlights the need for a high index of suspicion in all cases of compartment syndrome, especially in the rare event of a thigh compartment syndrome. Although the diagnosis remains a clinical one, intracompartmental pressure assessment using standard hospital equipment is possible and may assist in the diagnosis in equivocal cases.
TRAUMA CARE IN BOTSWANA - TOWARD SYSTEM DESIGN: THE BURDEN OF DISEASE
T Hardcastle1,2, Michael Mwandri1
1 University of KwaZulu-Natal, South Africa
2 Inkosi Albert Luthuli Central Hospital, South Africa
Ethics approval: Needs to be acquired
Introduction: Botswana is ranked among the highest countries for road traffic collisions (RTC), and similar to many Low-Middle-Income Countries (LMICs) it lacks trauma systems. The World Health Organisation (WHO) recommends 'Essential Trauma Care' in countries with no formal trauma systems. The current burden of trauma and the process of care in Botswana's main hospitals were investigated to gain an overview to design a LMICs trauma system.
Method: The study included blunt and penetrating trauma patients; burden, patient characteristic,s and the care-process indicators, comparing between pediatric and adult patients. Descriptive statistical analysis is used to present the data.
Results: The proportion of trauma patients ranged between 6- 10%, pediatric patients constituted 19%). Overall male proportion was higher at 59%. The median age was 28 [IQR 17-39] and eight years [IQR 4-11] for adults and pediatric patients respectively. The leading causes of injuries were violence, falls, and RTC, while the leading diagnoses were soft-tissue, long-bone fracture, and head injuries. The public inter-hospital vehicles transported up to 77% while the Emergency-Medical-Service transported 9-22% of patients. Median waiting time for emergency treatment was 194 minutes [IQR 114 -402] for pediatric and 206 minutes [IQR 97 -374] for adults. Most patients were none-acute (65-69%), and up to 84% were discharged on the same day as admission.
Conclusion: There is a significant burden of injuries with similar patient characteristics and process of care challenges between pediatric and adults, offering opportunity for designing similar interventions. The wide inter-hospital transport network may form an effective local prehospital system, while the process of care variables may be used for monitoring.
TRAUMATIC HEMIPELVECTOMY - THREE CASES AND LITERATURE REVIEW
T Hardcastle1,2, M P Faurie1,2, S Naidoo1,2, D James1,2, J Muckart1,2
1 University of KwaZulu-Natal, South Africa
2 Inkosi Albert Luthuli Central Hospital, South Africa
Ethics approval: Needs to be acquired
Introduction: Traumatic hemipelvectomy is rare and deadly, mainly due to haemorrhage early or sepsis later on.
Methods: Case presentation of three cases of traumatic hemipelvectomy in children / adolescents treated at IALCH and an overview of management in light of the existing literature.
Results: Three patients (two less than 10 years of age one aged 15 years) are presented and the literature is used to discuss the management of these technically challenging injuries.
Conclusions: These injuries require a good system and rapid regular access to theatre to ensure successful wound care. Prosthetic access is a challenge with limited possibility of success.
TRICEPS TENDON SPLITTING APPROACH FOR SUPRACONDYLAR INTERCONDYLAR FRACTURES IN ADULTS
V Sinevici1,2, S Rose1,2, C Frey1,2
1 CH Baragwanath Hospital, South Africa
2 University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Supra-condylar/inter-condylar fractures are not so common in adults. Treatment of bi-column and Y-type fractures can be rather challenging. Exposure of such fractures are often achieved with an olecranon osteotomy.
The olecranon osteotomy exposes the joint very well, but prolongs surgery, requires additional internal fixation an may present additional complications.
Over the past three years we treated 52 supra- and inter-condylar fractures. Five were AO Type 13-A, seven were uni-condylar AO Type 13-B and 40 were complete articular AO Type 13-C.
All patients were positioned laterally with the injured arm on a supporting padded pole. Our standard approach was the posterior midline incision. The triceps tendon was split in the same direction as the skin. The distal part of the triceps tendon was elevated off the olecranon. The distal apophyseal tendon fibers were kept intact on the olecranon.
We found that the joint was visible and accessible. The ulnar nerve was elevated off the bone for plate placement. We had no iatrogenic nerve palsy. All but the uni-condylar fractures had two column fixation with two pre-contoured locking plates in two planes. Closure was done by re-adaptation of the tendon fibers with absorbable sutures. Post operatively the elbow was immobilised in collar and cuff.
We found this approach an elegant, safe, and time saving way to operate the supra-and inter-condylar fractures of the humerus.
UNDERSTANDING THE BURDEN OF TRAUMA AT A JOHANNESBURG TRAUMA UNIT IN THE OVER EIGHT YEARS: A PARADIGM SHIFT
C Livhebe, S Motilall, S Gyebi, R Jacks, S Max, J Goosen
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: Trauma remains a major pandemic in South Africa. Unfortunately we still do not have a comprehensive National Trauma Registry that can allow us to evaluate the extent of the trauma disease burden. The emphasis on mortality figures as a measure of this disease is only a tip of the iceberg.
The Charlotte Maxeke Johannesburg Hospital Trauma unit (Johannesburg Trauma unit) participated in the development and implementation of the Medibank: an electronic trauma data collection system. This was implemented since January 2005, initially capturing only Priority 1 (severe trauma patients).
Aim: Evaluate epidemiological data of severe trauma patients (P1) entered into the Medibank at the Johannesburg Trauma Unit.
Method: All severe patients who presented to the Johannesburg Trauma Unit and were entered in the Medibank from January 2005 till December 2012 were included in the study. The demographics (age, sex, mechanism of injury), injury patterns, ISS, NISS, and mortality outcomes were evaluated. Comparisons were made between the different years to observe any trends. Statistical analysis was performed and a p value of <0.05 was considered significant.
Results: The 21-45 year old's were the most affected by trauma than any other age group. Overall, blunt trauma accounted for 50.28% of injuries, penetrating trauma 48.64% of the cases, and burns 1.08%. Stab injuries were the highest isolated cause of injury. The highest average ISS score was noted in burns group, followed by blunt trauma, with the lowest ISS score noted in the stab injuries. Blunt Trauma had the highest NISS score and again stabs had the lowest score. Predicted mortality was worst in blunt trauma group.
Conclusion: Blunt trauma is the most common mechanism, and is also associated with the high mortality. Medibank simplifies analysis of patterns of injury, which adds value in unpacking challenges to the health system. More effort is required to reduce the burden of trauma disease. A national Trauma Data System is urgently required to optimiSe our prevention strategy.
USE OF THE CPAX TOOL IN A SOUTH AFRICAN INTENSIVE CARE UNIT: CLINICAL OUTCOMES AND PHYSIOTHERAPISTS' PERCEPTIONS
M Whelan, H van Aswegen
Department of Physiotherapy, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
Ethics approval: Ethics approval: University of the Witwatersrand Human Research Ethics (Medical) Committee (M150726), South Africa.
Introduction: Research on the use of outcome measures in intensive care units (ICU) in South Africa is limited. The Chelsea Critical Care Physical Assessment (CPAx) tool measures morbidity related to physical function through assessment of respiratory function and functional abilities of patients with critical illness. The aims of this study are to determine whether the CPAx tool has an influence on clinical outcomes in critically ill patients and to determine physiotherapists' perceptions towards the use of the tool.
Methods: The study was performed in a South African public health care sector hospital. Part one was a quasi-experimental design with matched historical control group. Part two was a survey-based design. Participants in the experimental group received assessment with the CPAx tool on alternate weekdays during their ICU stay and their rehabilitation goals were modified according to CPAx scores obtained. Control participants were matched with participants in the experimental group for age, gender, diagnosis ,and acute physiology and chronic health evaluation (APACHE) II scores. A questionnaire was developed and was completed by physiotherapists who administered the CPAx tool.
Results: Participants in both groups (n = 26 respectively) were comparable with regards to demographics, diagnoses and APACHE II scores. Mean SOFA scores were significantly higher for control group (4.15 ±2.6) than experimental group (2.42 ±1.79) participants at ICU admission (p = 0.03) and at ICU discharge (control 2.87±1.81, experimental 1.8±0.42; p = 0.05). Mean initial CPAx score for the experimental group was 29.73 points (±14.81) and mean CPAx score at ICU discharge was 36.15 (±8.33). Mean CPAx scores changed by 9.45 points between ICU admission and discharge for experimental group participants who underwent surgical procedures and by 3.9 points for those who sustained traumatic injuries. No significant differences were found in ICU LOS (control 4.56 (±5.25) days, experimental 5.84 (±7.43) days; p = 0.54) or hospital LOS (control 19.31 (±15.79) days, experimental 17.43 (±16.68) days, p = 0.8) between the groups. Initial SOFA scores had a significant negative correlation with initial CPAx scores (r = -0.45; p = 0.02; n = 26). CPAx scores at ICU discharge had significant positive correlation with SOFA scores at discharge (r = 0.8; p = 0.05; n = 10). Physiotherapists (n = 2) reported positive perceptions of the CPAx tool.
Conclusion: CPAx did not influence ICU or hospital LOS in participants who underwent surgery or sustained traumatic injury. CPAx was more responsive to change when used with patients recovering from surgical procedures. Future work may include a multi-centre trial to evaluate the effect of CPAx on 24 hour LOS its effect on duration of mechanical ventilation. Raising awareness of this tool among South African ICU physiotherapists may enhance the use of outcome measures in clinical practice.
VIDEO-ASSISTED THORACOSCOPIC SURGERY VERSUS TUBE THORACOSTOMY RE-INSERTION FOR RETAINED TRAUMATIC HAEMOTHORAX:RESULTS UPDATE OF A RANDOMISED PROSPECTIVE STUDY
S Edu, A Nicol, P Navsaria
University of Cape Town, South Africa
Ethics approval: UCT(HREC 119/2013)
Introduction: The management of retained haemothoraces varies between institutions.
Aim: To compare the outcomes of Video-Assisted Thoracoscopic Surgery (VATS) and re-insertion of Tube Thoracostomy (TT) for retained haemothoraces.
Methods: A prospective randomised study of VATS versus TT for retained traumatic haemothoraces is being conducted at Groote Schuur Hospital, UCT(HREC 119/2013). All stable patients (aged 18-60 years) with a retained haemothorax were included. Exclusion criteria included haemodynamic instability, polytrauma, and underlying chronic lung disease. Demographics, type of procedure, hospital stay, and complications were documented. Statistical analyses were performed using the Chi-squared, Fisher exact, and Mann-Whitney-Wilcoxon rank sum test, a P-Value of 0.05 was considered statistically significant.
Results: The initial sample comprised 49 patients, seven patients were excluded, three postrandomisation and four pre. Data from 42 (20 VATS, 22 TT) patients was analysed. Hospital stay was similar in both groups. The complication rate was significantly higher in the TT group than the VATS group (45.5% vs. 10%, P = 0.011). Clinical follow up was 63.6% in the TT arm and 75% in the VATS arm.
Conclusion: VATS for retained traumatic haemothoraces is associated with lower morbidity than tube thoracostomy.
ARTHRODIASTASIS IN THE MANAGEMENT OF CHRONIC POST TRAUMATIC HIP DISLOCATION IN A YOUNG ADULT
D Naicker, M Karera, N Iqbal, M Ramokgopa
University of the Witwatersrand, Department of Orthopaedic Surgery, South Africa
Ethics approval: Needs to be acquired
Introduction: Dislocation of the hip joint requires emergency reduction in order to restore joint congruity. If the dislocation goes unreduced, reduction becomes increasingly difficult and the risk of associated complications such as Avascular necrosis and Secondary Osteo-arthritis increases.
We would like to present a case report of a 33 year old male who presented to our unit with an 11 month history of Right Traumatic Hip Dislocation. We would like to demonstrate the use of arthrodiastasis as part of our management of a chronic hip dislocation with significant soft tissue contractures and proximal migration of the femoral head.
Methods: Case report of a 33 year old male who was involved in motor vehicle accident with Right Hip Dislocation in December 2015. He was initially treated with skeletal traction for four months in Zimbabwe and discharged. He still complained of a right leg length discrepancy and foot drop and subsequently presented to our unit in October 2016 where he was found to still have a right hip dislocation with a leg length discrepancy of 6 cm and an associated sciatic nerve injury. Our initial concern was the significant incongruity of the hip joint that would be a challenge to hip arthrodesis or arthroplasty. Our plan was to attempt arthrodiastasis, with the use of an external fixator applied across the hip joint to assist in restoration of joint congruity to facilitate further management.
Results: Gradual distraction was achieved with the external fixator over a period of two months with the restoration of joint congruity as part of our first stage in the management of this chronic hip dislocation without complications.
Conclusion: Arthrodiastasis may provide a valuable role in the assisting with the reduction of proximal femoral migration associated with chronic hip dislocation.
MANAGEMENT OF NEGLECTED PATELLA FRACTURES
D Naicker, M Karera, N Iqbal, M Ramokgopa
University of the Witwatersrand, Department of Orthopaedic Surgery, South Africa
Ethics approval: Needs to be acquired
Introduction: Neglected patella fractures refer to fractures of the patella with delayed presentation to health services, usually more than three months post injury. These injuries often pose a challenge to management with regards to the need for surgical intervention; the choice of surgical procedure; and the ability to restore range of motion at the knee. The aim of our study was to review the management of these injuries in our unit as compared to available literature.
Methods: A retrospective case series was conducted at Chris Hani Baragwanath Academic Hospital, from November 2016 to April 2017. During this period five patients presented to our unit with neglected patella fractures, with an average time from injury to presentation of nine months (4-18 months). All five patients had sustained displaced transverse patella fracture with disruption of the extensor mechanism.
Results: All five patients underwent surgical intervention with open reduction and internal fixation by means of Tension Band Wire and Circlage. No pre-operative traction or intraoperative quadriceps lengthening were required. Adequate reduction was achieved in all five cases both clinically and radiologically.
Patients had protected weight bearing for two weeks post op in above knee backslabs and then initiated on physical therapy. All patients reported improvement in pain and ease of ambulation. On follow up all patients showed evidence of clinical and radiological union as well as restoration of the extensor mechanism.
One patient developed early superficial surgical site infection which was treated with intravenous antibiotics and resolved.
On follow up all five patients, are still attending outpatient physical therapy, with three of the five patients still demonstrating limited knee flexion between 70-90 degrees.
Conclusion: Neglected patella fractures may be managed in various ways in order to achieve fracture union and restoration of the extensor mechanism, however there is still significant difficultly in the restoration of normal range of motion of the knee.
THE BURDEN OF KNEE LIGAMENTOUS INJURIES AT CHRIS HANI BARAGWANATH ACADEMIC HOSPITAL
T Ncube, S K Magobotha, M T Ramokgopa
Department of Orthopaedics, University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: In busy trauma centres soft tissue knee injuries are often overlooked and more emphasis is paid to bony injuries. This is because they are of less dramatic presentation compared to fractures in the acute setting. However, they lead to loss of function and may complicate with articular surface degeneration.
Aims: To determine the profile of patients and the nature of ligamentous injuries sustained by patients at Chris Hani Baragwanath Hospital.
Methods: Retrospective review of patients with knee traumatic injuries treated with elective arthroscopic surgery.
Results: A total of 188 patients (190 knees) of which 50.5% were male. Males were on average younger than females (30.5 vs 37.5 years, p = 0.0001). The most prevalent mechanism of injury were road traffic accidents (25.8%), low energy falls (26.3%), and sports (23.2%). Cruciate, collateral, and posterolateral corner injuries (PLC) were mostly from traffic accidents whereas meniscal injuries were from low energy falls and sports. Intraoperatively males had a higher prevalence of ACL (50% vs 28.7% p = 0.04), medial meniscus (22.9% vs 11.7% p = 0.079), lateral meniscus (30.2% vs 16% p = 0.034) and multiligamentous injuries (22.9% vs 11.7% p = 0.041) compared to females. Intraoperatively diagnosed multiligamentous injuries outnumber known knee dislocations by three times (17.4% vs 5.3% overall prevalence in cohort). Peroneal nerve and vascular injuries had a low prevalence of 1% and 0.5% respectively.
Discussion: Despite this being a "Sports Unit" most ligamentous injuries are traffic accident related and the cohort is relatively young. Males have a predilection to high energy injuries (contact sports and traffic accidents) compared to females who have low energy fall injuries which in most cases were related to high BMI. The fact that there are much more multiligament injuries diagnosed intraoperatively compared to the known knee dislocations points to a high likelihood of missed diagnosis of spontaneously reduced dislocations.
Conclusion: Most knee ligamentous injuries are sustained by young patients and are predominantly caused by traffic accidents. There is a high likelihood of many knee dislocations that have reduced spontaneously and are missed at presentation.
SUCCESSFUL ENDOVASCULAR TREATMENT OF A TRAUMATIC CAROTID CAVERNOUS FISTULA PRESENTING WITH TORRENTIAL EPISTAXIS
T Ncube1, E Ncube2, S Moeng3, V Mngomezulu1
1 Department of Orthopaedics, University of the Witwatersrand, South Africa
2 Department of Diagnostic Radiology, University of the Witwatersrand, South Africa
3 Department of Trauma Surgery, Charlotte Maxeke Johannesburg Academic Hospital, South Africa
Ethics approval: Needs to be acquired
Introduction: Traumatic Carotid Cavernous Fistulae (CCF) is a rare pathology presenting in various ways including severe epistaxis. We present a polytrauma 38 year old male unrestrained driver involved in a high velocity collision with a concrete wall. He was admitted in the trauma intensive care unit with severe facial fractures and int chemosis on the left side. On the second week of admission, his stay was complicated by two episodes of severe torrential epistaxis managed emergently with nasal Foley's catheter tamponade, packing and blood transfusion. Computerised tomography angiograms revealed an established cerebral infarct and a left sided traumatic carotid cavernous fistula. Arteriography confirmed a left sided CCF, demonstrated some collateral flow. Embolisation of the carvenous sinus was not successful and we proceeded with endovascular coiling of the left internal carotid artery. Ocular symptoms resolved and there was no recurrence of epistaxis.racranial haemorrhages. He had marked periorbital swelling and
Discussion: CCFs are abnormal communication between the carvenous sinus and carotid arterial system. They are divided into traumatic and atraumatic types with the former arising from skull base and craniofacial fractures. The incidence of traumatic CCFs is quoted as 3.8%. CCFs may present with proptosis, chemosis, pulsatile exomphthalmos, diplopia, orbital pain and decreased vision. In the unconscious patient clinicians have to be astute to make a diagnosis. CCFs may complicate with subarachnoid and intracerebral haemorrhage, epistaxis and otorrhagia. Prompt resuscitation followed by appropriate imaging is essential. Once diagnosis is established, urgent definitive treatment is required because bleeding may be severe or life-threatening. Surgical ligation of the external or internal carotid arteries has been a traditional modality used by neurosurgeons. It is, however, now being superseded by less invasive endovascular techniques of balloon occlusion and coiling. Preservation of the patency of the internal carotid artery is key but may not always be possible especially if embolisation does not arrest abnormal blood flow. In this case, the internal carotid artery may be sacrificed. Our case already had established cerebral infarct and had evidence of collateral flow.
Conclusion: Our case highlights the potential complications that arise from severe skull base and craniofacial trauma. The clinician should have a high index of suspicion when faced with the typical physical signs, taking advantage of the latent period the CCF gives before manifesting its complications. Traumatic CCF should be recognised as a differential for severe epistaxis. Endovascular coiling can successfully be used to treat traumatic CCFs.
THE TRUELOK TRAUMA CIRCULAR FIXATOR, A VIABLE AND COST EFFECTIVE ALTERNATIVE TO MONOLATERAL FIXATORS
S Smith, R Paterson, S van Deventer
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: Open fractures of the tibia are common injuries seen in high-energy trauma events. Options for external fixation in our circuit include monolateral and Circular fixators.
The Majority of the Truelok system can be reused in many ways, e.g. in complex fractures, deformity corrections, Ilizerov constructs and lengthening, making it a cost effective device for state hospitals.
Despite these benefits, circular fixation is never used as a primary external fixator in our circuit. Monolateral fixators still remain the primary choice for the management of acute open fractures.
Methodology: A prospective trial was conducted to assess why circular fixation is overlooked and to introduce the Truelok trauma fixator (a device never used before in the circuit). This was done using questionnaires, video demonstrations and a dry bone workshop. Surgeons were randomly divided into groups and assigned a fractured bone with which to apply their external fixator of choice. Constructs were priced, timed, and graded for stability. Questionnaires assessed reasoning behind the surgeons preference for fixation and thoughts on circular fixation.
Results: 100% percent of participants elected to use a monolateral device with the majority (83%) of participants opting to use the Orthofix Procallus. The four most common reasons given for not selecting a circular fixator included: complexity, cost, time, and lack of experience.
Comparative costing of the constructs revealed no significant difference in price or time of application. However, ring fixation resulted in a significantly more stable construct.
After a video demonstration of a Truelok trauma frame, 90-95% of participants indicated they would be comfortable and interested in using the device, and agreed that it could play a primary role in the management of open fractures.
Conclusion: The Truelok trauma system can be a viable and cost effective option for the treatment of open fractures.
A PILOT STUDY, TRUELOK TRAUMA CIRCULAR FIXATOR IN THE INITIAL MANAGEMENT OF OPEN TIBIA FRACTURES
S Smith, R Paterson, S van Deventer
University of the Witwatersrand, South Africa
Ethics approval: Needs to be acquired
Introduction: In a non-clinical setting, an earlier trial showed the Truelok trauma ring external fixator to be no more expensive, time consuming, or complex than the standard monolateral systems being used in the the treatment of open Tibial shaft fractures. (See abstract submission titled the Truelok trauma circular fixator, a viable and cost effective alternative to Monolateral fixators.)
The Truelok system was significantly more stable, with better wound exposure. Accurate corrections could be done in the ward, without the need for re-manipulations in theatre. This, coupled with the system's ability to be reused for multiple applications, makes it an even more cost-effective option in our state hospitals.
Purpose: This pilot trial was used to determine if the results from our non-clinical trial would translate into clinical practice, and to see how easily orthopaedic residents would adapt to using a circular fixator they had no experience with.
Methodology: Five patients who had sustained open tibia fractures were recruited to the study.
Junior registrars applied the system and gave feedback regarding their impression of the system.
All procedures were timed and reductions documented. Poorly reduced fractures were corrected using the TL-Hex software in the ward. These patients were then monitored for complications, and/or loss of reduction and/or failure of the device, until union occurred.
Results: Registrars were comfortable with the device, found it no more complicated than a monolateral system, and indicated that reduction was easier with this system.
All fixatos were applied in under an hour, with all reductions being within acceptable limits.
Two border line reductions were converted to a TL-Hex (allowing for out of theatre manipulation). Both patients reductions were easily improved in the ward with minimal discomfort experienced by the patient.
All patients were full weight bearing within two weeks, and achieved union with no loss of reduction.
Conclusion: This pilot study has shown that the Truelok Trauma Circular Fixator, is a cost effective alternative to monolateral external fixation in Tibial shaft fractures, and can be used safely and effectively.
On this basis a larger randomized control trial will begin comparing this system to a popular monolateral system.
ORTHOPAEDIC TERROR MEDICINE: ARE WE READY TO DEAL WITH THE INJURIES SUSTAINED FROM AN INTENTIONAL MASS CASUALTY INCIDENT IN SOUTH AFRICA?
A Hirschmann1, B Gelbart1,2, C Frey1,3
1 University of the Witwatersrand, South Africa
2 Charlotte Maxeke Johannesburg Academic Hospital
(CMJAH), South Africa
3 Chris Hani Baragwanath Academic Hospital, South Africa
Ethics approval: Needs to be acquired
Introduction: Terror Medicine is an evolving specialty which incorporates multiple disciplines of which Orthopaedics has a significant role to play. Five of the world's leading ten countries with the highest number of terror attack fatalities are on the African continent. Studies have shown that prior preparation can significantly reduce the impact of the event on routine functioning of the health care system and improve patient care. The outcome depends on four major phases: Pre-hospital response, patient transport, hospital triage, and definitive care.
Methods: We conducted an extensive literature review and developed a model action plan. We then assessed the perceived and actual readiness of integral components of our hospital, the largest in the Southern Hemisphere, via a simple survey. We analysed the responses.
Results: The literature highlights that prior planning can improve patient outcomes and mitigate the additional stress on the hospital system.
An evaluation of the current plan for dealing with a terrorist attack at CHBAH was made.
Findings indicate the need for pre-hospital (EMS), nursing-care, and administrative preparation as well as developing a state of readiness to rapidly provide definitive care to terror-attack casualties.
Discussion: Understanding the injury patterns seen in terror attacks are crucial in the development of a hospital specific response plan. This model plan involves the intimate coordination between multiple parastatal departments, medical, and surgical disciplines.
The Orthopaedic Surgeon has a major role to play in these events as studies have shown that the majority of injuries sustained (up to 70%) are extremity related injuries. These injuries are the major reason for surgical management.
Conclusion: South African hospitals are relatively well-prepared for significant trauma cases due to a high incidence of violent crime. Despite this invaluable experience, we are not adequately prepared to deal with the magnitude and scope of terror-related injuries in a holistic way.
The increasing number of terrorist attacks forces us to develop an attack response protocol, which will empower our healthcare professionals to lead with confidence during a high-stress scenario and enable us to save more lives.
SEVERE PEDIATRIC TRAUMA IN KWAZULU NATAL, EPIDEMIOLOGY AND RESOURCE UTILISATION
D den Hollander1, D Muckart2
1 University of KwaZulu Natal, Traunma Unit, South Africa
2 Inkosi Albert Luthuli Central Hospital, Trauma Unit, South Africa
Ethics approval: Needs to be acquired
Objectives: To review the epidemiology, resource utilisation and outcomes of a group of seriously injured children admitted to a Level 1 Trauma Center in a Middle-Income Country (LMIC).
Methods: Review of the database of the pediatric entries (children under 18 years) to the Level 1 Trauma Unit at the Inkosi Albert Luthuli Central Hospital between 2007 and 2012. The following information was gathered: demographics, mechanism of injury, type of injuries, resource utiliSation (imaging, operative procedures, average ventilator days, and ICU stay) and outcome (Glasgow Outcome Scale).
Results: 79 children were six years or younger; 61 were of school age (7-12), and 27 were teenagers (13-18 years). Female, male ratio was 1:1.06. The majority (80.9%) of injuries were transport related, with 53.1% being pedestrian collisions. Assaults accounted for 10.5% of injuries, with 9.6% being penetrating injuries. Imaging procedures were performed in 70.7%, with Pan-CT angiograms performed in 61.8%. Head injuries occurred in 60.5% of children, chest injuries in 52.5% (lung contusions in 36,1%), abdominal injuries in 56.2%, and fractures and / or dislocations in 46.5%. The most commonly associated injuries in head-injured patients were lung contusions (46%) and femur fractures (31%); for patients with chest trauma severe head injuries (69%), femur fractures (38%) and liver injuries (32%); for patients with abdominal injuries lung contusions (38.5%) and femur fractures (36%). 67% of children underwent surgery, half of which (50.8%) were neurosurgical procedures, followed by abdominal procedures (20.4%), and orthopedic procedures (19.1%). Mortality was 16.7%, while 38.9% made a full recovery; 14.2 had minor disabilities and 30.3 had serious disabilities at the time of discharge.
Conclusions: This study reflects the high prevalence of traffic-related injuries in children and the poor outcomes in this group (GOS < 3:47%) in an LMIC.
THE LAUTENBACH SUCTION-INSTILLATION SYSTEM AS AN INTERNAL SUCTION DRESSING AND INFECTION PROPHYLA
R Kyte1,2, F Snyman3
1 University of the Witwatersrand, Donald Gordon Medical Centre, South Africa
2 Union & Clinton Hospitals, South Africa
3 Wilgeheuwel Hospital, South Africa
Ethics approval: Needs to be acquired
The benefits of the Lautenbach Suction-Instillation System have been recognised as an adjunct for the eradication of bone and joint infection. With the wide acceptance of external vacuum dressings as a means of accelerating wound healing and facilitating evacuation of exudation, the advantages of a system, which provides these benefits for deep cavities, together with the direct infusion of antibiotics with markedly increased local tissue concentrations, may be considered of logical benefit. This was deemed particularly useful in complex trauma orthopaedic cases with associated tissue loss (e.g.: Gustilo & Anderson Type IIIB&C). These clinical situations are associated with a reported incidence of infection of as high as 44%. The Lautenbach suction-instillation system was prospectively utilised in 161 such patients over a 13 year period (2004-2016). Immediate soft tissue cover was achieved in some instances but delayed for several weeks in others. Six deep infections were noted (3.7%) at an average 3.6 year follow-up. These were all successfully eradicated with a secondary debridement and Lautenbach suction-instillation. Our results are encouraging for the use of this system in minimising infection under these challenging clinical circumstances.
PROFILE OF SPINAL CORD INJURIES IN KWAZULU-NATAL: IMPLICATIONS FOR VOCATIONAL REHABILITATION
N Pefile1, S Naidoo2, J D Mothabeng3
1 Division of Physiotherapy, School of Health Sciences, University of KwaZulu-Natal, South Africa
2 Discipline of Occupational Health Medicine, School of Public Health and Nursing, University of KwaZulu-Natal, South Africa
3 Discipline of Physiotherapy, School of Health Sciences, University of Pretoria, South Africa
Ethics approval: Needs to be acquired
Objectives: To describe the demographic and socio-economic profiles, and injury related characteristics of people who sustain SCIs in KZN.
Materials and Methods: King Dinizulu Hospital Spinal Unit (KDHSU), this being the biggest provider of acute care for people who sustain SCI in KwaZulu-Natal and the Eastern Cape Provinces, South Africa. Medical files of individuals who sustained SCI between 2009 and 2012 were perused. Key information from the files were extracted using a tool developed using literature and international spinal cord injury core data set.
Results: 1 049 medical files were perused and 188 met the inclusion criteria. The average annual incidence rate was 12.3 per 100 000 population. The male to female ratio was 6:4 with the mean age of 36.69 years, ranging from 16-64. Out of those employed (34%), 72% were working fulltime, in mostly in the service industry (31%) and 59% were classified as labourers. The majority (61%) of the participants completed high school. The major cause of SCI was non-traumatic (54%) and 66% were classified as incomplete (ASIA) and 80% were paraplegia. The mean LOS was 42.9 days, ranging from 1-764 days, influenced by level of injury, completeness and classification of injury and surgical intervention.
Conclusion: The profile of SCI in KwaZulu-Natal is slightly different when compared to other provinces in South Africa and the rest of Africa. There is a need to use epidemiological information (including factors that influence employment) to develop rehabilitation models to guide employment outcomes amongst people living with spinal cord injuries in KZN.














