Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.55 no.4 Cape Town Nov. 2017
TRAUMA
Laparoscopy or clinical follow-up to detect occult diaphragm injuries following left-sided thoracoabdominal stab wounds: A pilot randomized controlled trial
G F Malherbe; P H Navsaria; A J Nicol; S Edu; S Chowdhury
Trauma Centre, Groote Schuur Hospital, University of Cape Town, Cape Town, South Africa
ABSTRACT
BACKGROUND: The purpose of this study was to determine whether patients with left-sided thoracoabdominal (TA) stab wounds can be safely treated with clinical and chest X-ray follow up.
METHOD: A prospective, randomized control study was conducted at Groote Schuur Hospital from September 2009 through to November 2014. Patients with asymptomatic left TA stab wounds included in the trial were randomized into two groups. Group A underwent diagnostic laparoscopy and Group B underwent clinical and radiological follow-up.
RESULTS: Twenty-seven patients were randomized to Group A (N=27) and thirty-one to Group B (N=31). All patients were young males with a median age of 26 years (range 18 to 48). The incidence of occult diaphragm injury in Group A was 29%. All diaphragm injuries found at laparoscopy were repaired. The mean hospital stay for the patients in Group A was 5 days (SD 1.3), compared to a mean hospital stay of 2.9 days (SD, 1.5), in Group B (p < 0.001). All patients in Group B had normal chest X-rays at their last visit. The mean follow-up time was 24 months (median: 24; interquartile range: 1-40). There was no morbidity or mortality in Group B.
CONCLUSIONS: Clinical and radiological follow-up are feasible and appear to be safe, in the short term, in patients who harbour occult diaphragm injuries after left TA stab wounds. Until studies showing the natural history of diaphragm injury in humans are available, laparoscopy should remain the gold standard in treatment.
Introduction
Selective non-operative management (NOM) of abdominal stab wounds has become the standard of care around the world.1 The problem with the NOM of patients with thoracoabdominal (TA) stab wounds without peritoneal signs is that these asymptomatic patients may harbor isolated diaphragm injuries that may go undetected, and later develop a diaphragm hernia. To overcome this, it was initially proposed by Stylianos et al.2 that all left side TA stab wounds should undergo a laparotomy to rule out a diaphragm injury. During the mid 1990s, when videoscopy was introduced and popularized in other areas of surgery, numerous studies confirmed that both laparoscopy and thoracoscopy are very sensitive and specific in detecting a diaphragm injury.3-7 Even today with the modern multidetector CT (MDCT) imaging, direct vision of the diaphragm with laparoscopy and thoracoscopy remains the gold standard of diagnosing an occult diaphragm injury.8 Current international guidelines, including those of the Eastern Association for the Surgery of Trauma (EAST), recommend that all patients with left-sided penetrating thoracoabdominal trauma undergo routine diagnostic laparoscopy under general anesthesia to exclude a diaphragm injury.9 The purpose of this study was to establish the incidence of occult diaphragm injury in our local trauma population and to establish if close initial observation and subsequent follow up is a safe and feasible practice for this group of patients.
Patients and methods
Study design
The study was a single center, parallel-group trial with equal randomization conducted at the Trauma Centre at the Groote Schuur Hospital from 01 September 2009 through to01 November 2014. Study inclusion criteria were age between 18 and 60 years, asymptomatic left TA stab wounds (bounded by the nipple line over the anterior and posterior chest, superiorly, the left costal margin inferiorly and, the tip of the scapula and the sternum, medially), passed 24-hour period of abdominal observations and signed informed consent. Study exclusion criteria were signs of diaphragm injury, either radiological or clinical, hemodynamically unstable patients, previous penetrating injury to the left TA area, patients requiring early surgical exploration for injuries other than diaphragm injuries, and a positive pregnancy test. The study was approved by the Faculty of Health Sciences Research Ethics Committee of the University of Cape Town and registered at ClinicalTrials.gov NCT01044550.
Management protocol
All patients with left TA stab wounds and suspected occult diaphragm injury were subjected to a 24-hour period of serial abdominal observations to identify patients who required laparotomy for associated intra-abdominal injury. The site of injury was recorded on a visual torso map and divided into lateral, anterior and posterior stab wounds. The lateral region is between the anterior and posterior axillary lines, the anterior territory is anterior to the anterior axillary line and the posterior territory is posterior to the posterior axillary line. Patients with a pneumo- and/or hemothorax were managed with a tube thoracostomy. During the observation period, patients were kept nil per os and maintained on intravenous fluids. Analgesia alone with no antibiotics was administered. The patients were clinically reassessed every 6 hours. Patients who did not develop foregut symptoms (nausea and vomiting) or signs of peritonism after 24 hours were considered eligible for the trial. After informed consent was taken, the patients were randomized into a treatment Group A and follow-up Group B.
Group A underwent a diagnostic laparoscopy, with repair to an injured diaphragm when detected. The local incidence of diaphragm injury in this subset of trauma patients was thus determined. Group B underwent no treatment except suturing of wounds and drainage of a hemo- / pneumothorax when present. Participants in Group A were requested to attend a follow-up clinic in 2 weeks. Participants in Group B were requested to attend a follow-up clinic at 2 weeks, 4 weeks, 3 months, 6 months, 12 months and yearly intervals. During follow up a detailed history was taken and a chest X-ray performed.
Randomization process
A computerized number generator was used to create a random number table with the numbers 1 (laparoscopy) and 2 (clinical follow-up). These numbers were placed in a sealed envelope. If a patient was considered eligible to participate in the trial, informed consent was taken and the envelope was opened to reveal the group into which the patient fell.
Endpoints of study
The primary endpoints were the demonstration of a diaphragmatic laceration at laparoscopy or any evidence of a diaphragmatic hernia during follow-up. Secondary end points were the duration of hospital stay and complications.
Statistical methods
Using a two-sided binomial test, a sample size of 100 achieves 83% power to detect a difference of 0.15 with a significance level of 0.035.10-13 Continuous variables were compared with the use of the /-test. Chi-square analysis and the Fisher exact test were used for the analysis of the categorical variables where appropriate. Confidence intervals were based on the normal approximation to the binomial distribution. P values of less than 0.05 were considered to be significant.
Results
We identified 64 potentially eligible patients of which 62 met inclusion criteria. Five patients were excluded, two did not meet the inclusion criteria and three declined to participate by refusing consent. The final sample group, therefore, consisted of 59 patients. After providing informed consent, they were subsequently randomized to 28 in Group A and 31 in Group B. We discontinued enrollment before reaching our sample size goal of 100 patients due to slow patient accrual. There were no protocol violations and one patient was excluded after randomization in Group A due to failed laparoscopy and laparotomy because of extensive adhesions (frozen abdomen) after a previous laparotomy. Therefore, 27 patients were analyzed in Group A and 31 in Group B. The enrollment and outcomes are presented in Figure 1 according to the Consort 2010 flow diagram.14
Patient characteristics
The 59 patients selected for the study were all hemodynamically stable on arrival. The baseline characteristics of the 2 groups were comparable in respect of age, mean arterial pressure, respiratory rate, hemoglobin level, and revised trauma score (Table 1).
Area of injury
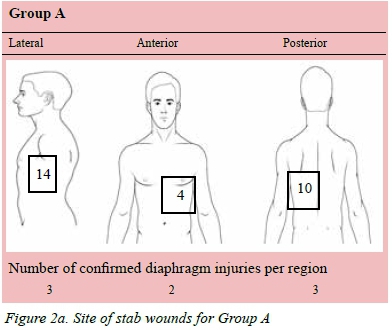
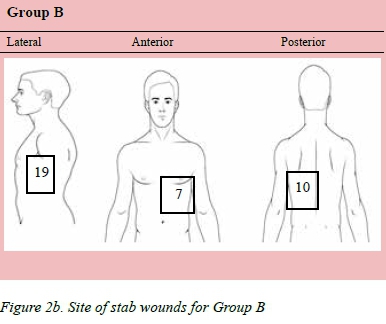
The site of injury was recorded on a visual torso map and divided into lateral, anterior and posterior stab wounds. The lateral region is between the anterior and posterior axillary lines, the anterior territory is anterior to the anterior axillary line and the posterior territory is posterior to the posterior axillary line. Some patients presented with multiple stabs. The findings are represented in Figure 2a and Figure 2b.
Laparoscopy group (n = 27)
The stab wounds penetrated the chest at various TA locations with no specific level associated with an increased likelihood of diaphragm injury. All the patients were subjected to initial laparoscopy under general anesthesia, two patients were converted to laparotomy and one patient to thoracotomy. The decision to convert was left to the discretion of the operating surgeon and was done more often because of difficulty in visualizing or repairing the diaphragm. Three patients were converted to an open procedure, all of whom had a diaphragm injury. Eight (29%) of 27 patients in Group A had a diaphragm laceration. All the lacerations were smaller than 2 cm in length. One patient had omentum herniating through the diaphragm injury. Seventeen (62%) patients had an associated hemo/pneumothorax managed with pleural drainage.
Follow up group (n = 31)
The mean follow-up of patients allocated to Group B was 24 months (median: 24; interquartile range: 1-40). Twenty-three (74%) patients had a pleural drain inserted for a hemo/pneumothorax. At the last follow-up, all chest X-rays were normal and all patients had a normal clinical examination with no abdominal or thoracic symptoms. The X-rays were reviewed by a single, senior consultant (author two) in the trauma center. Five patients (16%) had no follow-up and four (12%) patients had limited follow-up ranging from 1-9 months before they were lost to follow-up.
Morbidity and Mortality
No patients died as a result of injuries sustained during the initial hospitalization. Three patients had postoperative complications in Group A. The complications were superficial surgical site sepsis, pneumonia and prolonged postoperative paralytic ileus. The patient with surgical site sepsis was managed with suture removal and antibiotics. The patient who developed pneumonia was a patient converted to laparotomy and was managed with antibiotics, physiotherapy and mobilization. The patient with the prolonged ileus was managed conservatively, and the ileus resolved four days post-operatively. These complications were classified as grade II complications, according to the Clavien-Dindo classification of surgical complications.15 There was no morbidity in Group B.
Hospital Stay
The mean hospital stay in the patients who underwent laparoscopy was 5 days (SD 1.3), compared to a mean hospital stay of 2.9 days (SD 1.5), resulting in a statistically significant difference of p < 0.001. In the authors opinion the laparoscopy group had a longer hospital stay because of reasons related to theatre access. They were a stable group of patients and often had to wait for theatre access after more urgent cases.
Discussion
Current EAST guidelines9 strongly recommend diagnostic laparoscopy in all patients with penetrating trauma to the left TA area who have no other indications for laparotomy to diagnose and repair diaphragm injuries. The main purpose of repairing diaphragm injuries is to prevent delayed diaphragm herniation which is reported to have a high associated mortality rate. Most papers quote the high mortality of 36% in patients presenting with delayed herniation of abdominal contents into the chest as reported by Madden et al.16 Degiannis et al.17 described a 25% mortality rate in a group of patients who presented with delayed diaphragm hernias over a 7-year period. Not all data support this high mortality initially reported by Madden and Degiannis. Reber et al.18 reported on the outcome of 10 patients with late presentations of traumatic diaphragmatic hernias during a 16-year period. Only one patient died (10% mortality), and three (30%) sustained postoperative complications. Feliciano et al.19 did a 9-year review of patients who presented at one trauma center. Seven patients presented with delayed diaphragm hernias. No patients died, but 5 out of 7 patients had postoperative complications. It is twenty-five years since the article by Madden et al. was published and, with modern critical care practices, the high mortality rate associated with delayed diaphragm hernia reported by Madden is not observed anymore. More recently, studies have reported lower mortality in patients presenting with delayed diaphragm hernia.20,21
The results from animal studies are listed in Table 2. From this data, it is clear that in animal studies more than 90% of diaphragm injuries heal spontaneously,2225 in 6-40 weeks, but it is difficult to extrapolate this data directly to humans because the natural history of diaphragm injuries in humans has not been adequately studied. However, it must be true that a large percentage of diaphragm injuries in humans heal, or at least never become clinically apparent because studies done to detect an occult left diaphragm injury reported rates of 26% to 63% of diaphragm injuries in patients who sustained left sided TA stab wounds.32627 The rate of delayed diaphragm herniation reported in the literature varies from 2.7-4%.1928 This large difference in the rate of injury compared to the rate of delayed diaphragm herniation can only be true if most of these injuries heal or never become clinically apparent.
As discussed previously from the available evidence, mortality of delayed diaphragm injury is overestimated and the incidence of delayed herniation is low, therefore many patients will undergo unnecessary surgery to detect and repair diaphragm injuries that would never have resulted in a diaphragm hernia. This has significant cost implications in a resource-limited environment as patients who undergo surgery have a significantly longer hospital stay, 5 vs 2.9 days p = < 0.001, as well as the added procedural cost.
We are of the opinion that patients who present with a delayed diaphragm hernia most likely had a missed initial diaphragm injury that occurred within the first six weeks post injury. The initial injury presented late and if these patients were subjected to close follow-up these injuries would have been detected earlier. We, therefore, suggest that the herniation is an early event, and strangulation/complication is a delayed event because, in patients who present with late complications, there are always signs of a 'chronic' hernia at surgery. Established adhesions between the hernia sac and the diaphragm are a common finding at surgery pointing towards a chronic process.
We undertook this randomized study to firstly establish the incidence of occult diaphragm injury in our patient population and to follow up a control group of patients who should have a similar incidence of occult diaphragm injuries. The patients were followed up to establish the incidence of delayed diaphragm herniation in a truly asymptomatic group of patients and, if a hernia was detected, to establish the morbidity of early intervention. The incidence of diaphragm injury was 29% and it can, therefore, be assumed that the incidence of a diaphragm injury in Group B would be similar because the two groups were comparable in terms of patient characteristics. During the follow-up period, no delayed diaphragm hernias occurred, neither did any patient report any significant symptoms.
Limitations of study
Firstly, the study never recruited the intended sample size, which impacts negatively on the conclusions that can be made. This can possibly be overcome by repeating a larger multicentre trial. Secondly, a major limitation of this study was the number of patients lost to follow-up, especially in Group B. Five patients (16%) had no follow-up and four patients (12%) had limited follow-up ranging from 1-9 months before they were lost to follow-up. According to Leukhardt et al.29 lower income, higher poverty rates, and lower education were significantly associated with failure to follow up. The patients included in this study meet the above criteria and that would account for the high rate in the failure of follow-up despite efforts made to make contact with the patients who failed to attend follow-up appointments. Even if a larger multicentre trial is undertaken, this problem is likely to persist. Thirdly, the radiological imaging was limited to serial chest X-rays. The sensitivity of plain chest x-rays is 94% in the presence of herniation, but it can be as low as 30-62% in the absence of a hernia with a small diaphragmatic laceration. Despite this low sensitivity, chest X-ray is still the initial imaging modality of choice with MDCT, with magnetic resonance imaging being recommended if diagnostic doubt exits.30,31
Conclusion
The incidence of occult diaphragm injury in left sided TA stab wounds is high. In a highly selected group of asymptomatic patients who have undergone a period of abdominal observation, it is safe to discharge these patients provided that they are followed up with clinical examination and serial chest X-rays. The optimal period of follow-up is still uncertain and could not be reliably established in this trial due to the slow rate of patient accrual, the high rate of patients lost to follow-up and the short follow-up time. If patients are treated conservatively, they should be made well aware that should any abdominal symptoms develop, even if years later, to report to a health facility immediately stating that they sustained a left TA stab in the past, alerting the treating physician to the possibility of the patient having a delayed diaphragm hernia. Because of the limitations of this trial, a larger multicentre, randomized trial to confirm these findings and to prove long-term safety of clinical and radiological follow-up is recommended. A study documenting the findings of a diagnostic laparoscopy 3-6 months after the initial injury would clarify the unanswered question relating to the natural history of left sided penetrating TA injuries in humans. Until the natural history of penetrating left sided diaphragm injury in humans is documented patients should continue to undergo diagnostic laparoscopy as the gold standard treatment.
Conflicts of interest and sources of funding:
PHN received a self-initiated grant from the Medical Research Council of South Africa.
REFERENCES
1. Robin AP, Andrews JR, Lange DA, Roberts RR, et al. Selective management of anterior abdominal stab wounds. J Trauma-Injury, Infection, and Critical Care. 1989;29(12):16849. [ Links ]
2. Stylianos S, King TC. Occult diaphragm injuries at celiotomy for left chest stab wounds. Am Surg. Jun 1992;58(6):364-8. [ Links ]
3. Mjoli M, Oosthuizen G, Clarke D, Madiba T. Laparoscopy in the diagnosis and repair of diaphragmatic injuries in left-sided penetrating thoracoabdominal trauma. Surg Endosc. 2014;1-6. [ Links ]
4. Bagheri R, Tavassoli A, Sadrizadeh A, Mashhadi M, et al. The role of thoracoscopy for the diagnosis of hidden diaphragmatic injuries in penetrating thoracoabdominal trauma. Interact Cardiovasc Thorac Surg. 2009;9(2):195-98. [ Links ]
5. Opasanon S, Akaraviputh T, Keorochana K, Somcharit L. The role of laparoscopic management in suspected traumatic diaphragmatic injury patients: a tertiary care center experience. Medical Journal of the Medical Association of Thailand. 2009;92(7):903. [ Links ]
6. Powell BS, Magnotti LJ, Schroeppel TJ, Finnell C, et al. Diagnostic laparoscopy for the evaluation of occult diaphragmatic injury following penetrating thoracoabdominal trauma. Injury. 2008;39(5):530-4. [ Links ]
7. Paci M, Ferrari G, Annessi V, de Franco S, et al. The role of diagnostic VATS in penetrating thoracic injuries. World J Emerg Surg. 2006;1:30. [ Links ]
8. Stein DM, York GB, Boswell S, Shanmuganathan K, et al. Accuracy of computed tomography (CT) scan in the detection of penetrating diaphragm injury. J Trauma 2007;63(3):538-43. [ Links ]
9. Como JJ, Bokhari F, Chiu WC, et al. Practice Management Guidelines for Selective Nonoperative Management of Penetrating Abdominal Trauma. J Trauma. 2010;68(3):721-33. [ Links ]
10. Fleiss JL, Levin B, Cho Paik M. Statistical Methods for Rates and Proportions. 3rd ed. New York: John Wiley & Sons; 2003. [ Links ]
11. Lachin, John M. Biostatistical Methods. New York: John Wiley & Sons; [ Links ]
12. Machin D, Campbell M, Fayers P, Pinol A. Sample Size Tables for Clinical Studies, 2nd ed. Malden, Mass: Blackwell Science; [ Links ]
13. Zar JH. Biostatistical Analysis (Second Edition). Englewood Cliffs,New Jersey: Prentice-Hall; [ Links ]
14. Schultz KF, Altman DG, Moher D. CONSORT 210 statement: updated guidelines for reporting parallel group randomized trials. BMJ (Clinical research Ed.) 2010;340:c332. [ Links ]
15. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, et al. The Clavien-Dindo classification of surgical complications. Ann Surg. 2009;250:187-96. [ Links ]
16. Madden MR, Paull DE, Finkelstein JL, Goodwin C, et al. Occult diaphragmatic injury from stab wounds to the lower chest and abdomen. J Trauma Acute Care Surg. 1989;29(3):292-8. [ Links ]
17. Degiannis E, Levy R, Sofianos C, Potokar T, et al. Diaphragmatic herniation after penetrating trauma. Br J Surg. 1996;83(1):88-91. [ Links ]
18. Reber P, Schmied B, Seiler C, Baer HU, et al. Missed diaphragmatic injuries and their long-term sequelae. J Trauma Acute Care Surg. 1998;44(1):183-8. [ Links ]
19. Feliciano DV, Cruse PA, Mattox KL, Bitonda C, et al. Delayed diagnosis of injuries of the diaphragm after penetrating wounds. J Trauma. 1988;28:1135-43. [ Links ]
20. Alimoglu O, Eryilmaz R, Sahin M, Oszoy MS. Delayed traumatic diaphragmatic hernias presenting with strangulation. Hernia. 2004;8:393-6. [ Links ]
21. Clarke D, Greatorex B, Oosthuizen G, Muckart D. The spectrum of diaphragmatic injury in a busy metropolitan surgical service. Injury. 2009;40(9):932-7. [ Links ]
22. Shatney CH, Sensaki K, Morgan L. The natural history of stab wounds of the diaphragm: implications for a new management scheme for patients with penetrating thoracoabdominal trauma. Am Surg. Jun 2003;69(6):508-13. [ Links ]
23. Perlingeiro JA, Saad Jr R, Lancelotti CL, Rasslam S, et al. Natural course of penetrating diaphragmatic injury: an experimental study in rats. Int Surg. Jan-Feb 2007;92(1):1-9. [ Links ]
24. Gamblin TC, Wall Jr CE, Morgan JH, Erickson DJ, et al. The natural history of untreated penetrating diaphragm injury: an animal model. J Trauma-Injury, Infection, and Critical Care. 2004;57(5):989-92. [ Links ]
25. Zierold D, Perlstein J, Weidman ER, Wiedeman E. Penetrating trauma to the diaphragm: natural history and ultrasonographic characteristics of untreated injury in a pig model. Arch Surg. 2001;136(1):32-7. [ Links ]
26. Murray JA, Demetriades D, Cornwell EE, Asensio JA, et al. Occult injuries to the diaphragm: prospective evaluation of laparoscopy in penetrating injuries to the left lower chest. J Am Coll Surg. 1998;187(6):626-30. [ Links ]
27. Morales CH, Villegas MI, Angel W, Vásquez JJ. Value of digital exploration for diagnosing injuries to the left side of the diaphragm caused by stab wounds. Arch Surg. 2001;136(10):1131-5. [ Links ]
28. Leppâniemi A, Haapiainen R. Occult diaphragmatic injuries caused by stab wounds. J Trauma-Injury, Infection, and Critical Care. 2003;55(4):646-50 [ Links ]
29. Leukhardt WH, Golob JF, McCoy AM, Fadlalla AM, et al. Follow-up disparities after trauma: a real problem for outcomes research. Am J Surg. 2010;199: 348-53. [ Links ]
30. Payne JH, Yellin AE. Traumatic diaphragmatic hernia. Arch Surg.1980;20:587-91. [ Links ]
31. Hanmuganathan K, Killeen K, Mirvis SE, White CS. Imaging of Diaphragmatic Injuries. J Thorac Imaging. 2000;15(2): 104-11. [ Links ]
 Correspondence:
Correspondence:
Pradeep H Navsaria
pradeep.navsaria@uct.ac.za














