Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.55 no.4 Cape Town Nov. 2017
TRAUMA
Barriers to accessing ATLS provider course for junior doctors at a major university hospital in South Africa
J J Odendaal; V Y Kong; T Liu; Y Liu; B Sartorius; G V Oosthuizen; D L Clarke
Pietermaritzburg Metropolitan Trauma Service, Department of Surgery, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
ABSTRACT
BACKGROUND: Advanced trauma life support (ATLS) is the international standard of care and forms the basis of trauma training in South Africa. Previous local studies demonstrated a low completion rate among junior doctors (JD). This study was designed to determine the reasons and identify possible barriers of JDs to accessing the ATLS course at a major university hospital.
METHODS: This was a prospective study utilising a structured survey that included all JDs who were undertaking their internship training.
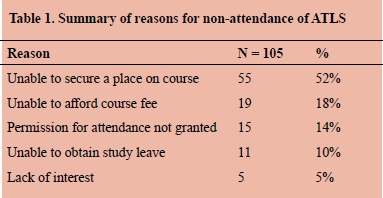
RESULTS: A total of 105 JDs completed the survey. Sixty-two percent were female (65/105) and the mean age was 25 years. Forty-eight percent (50/105) of all JDs were post graduate year 1 (PGY 1) and the remaining 52% were post graduate year 2 (PGY 2) JDs. Sixty-two percent (65/105) of all respondents had completed their mandatory rotation in surgery. The reasons for non-attendance of ATLS were: unable to secure a place on course (52%), unable to afford course fee (18%), permission for attendance not granted (14%), unable to obtain study leave (10%) and lack of interest (5%). Subgroup analysis comparing the reasons for PGY1s vs PGY2s demonstrated that not being able to secure a place on course was more common among PGY2s [19% vs 33%, p < 0.001] while financial reasons were more common among PGY1s [18% vs 0%, p < 0.001.
CONCLUSIONS: The primary barriers for JDs to attending ATLS training is difficulty in accessing the course due to oversubscription, financial reasons, followed by difficulty in obtaining professional development leave due to staff shortage. There is an urgent need to improve access to the ATLS training course for JDs in our environment.
Introduction
Advanced trauma life support (ATLS) is the current international standard for the management of trauma patients.1 In South Africa, the course has been enthusiastically endorsed over the last two decades and continues to form the basis of the curriculum for trauma training at both undergraduate and postgraduate level.2 There is evidence to suggest that the ATLS programme improves patient outcome.39 A previous study from our institution demonstrated an improvement in the anatomical knowledge of junior doctors (JDs) in various key trauma procedures following successful completion of ATLS.10 However, it was noted that only 15% of all JDs had completed the ATLS course at the time of study.10 There is currently no literature focusing specifically on reasons for such low completion rate in our developing world setting. The aims of this study were to determine the reasons and identify possible barriers to JDs accessing the ATLS course at a major university hospital in South Africa.
Methods
Clinical Setting
This was a prospective, observational study performed in January 2015 at the Pietermaritzburg Metropolitan Trauma Service (PMTS) in South Africa. Ethics approval to conduct this study was formally granted by the Biomedical Research Ethics Committee (BREC) and the University of KwaZulu Natal (reference number: BE083/14). The city of Pietermaritzburg is the capital of the KwaZulu Natal province and the PMTS provides definitive trauma care that covers the western part of the province. It also serves as the referral centre for 19 other district hospitals and covers a total catchment population of over three million. Our trauma service manages approximately 3 000 cases per annum, with over 40% penetrating trauma. This is a direct reflection of the high incidence of interpersonal violence and serious crime experienced throughout the region.11
ATLS programme
The ATLS programme in South Africa is administered under the auspices of the Trauma Society of South Africa (TSSA). Each of the provinces where the ATLS course is provided is overseen by a director of training for the province. Any qualified doctors (both local and international medical graduates) are eligible to enrol for the programme. The course is almost always oversubscribed and it is common for potential applicants to be placed on a waiting list.
Internship Training
The Department of Surgery is an academic department under the auspices of the University of KwaZulu Natal and is responsible for both undergraduate and postgraduate training in general surgery. It is a Health Professions Council of South Africa (HPCSA) accredited institution for internship training. Internship training in South Africa lasts a period of 24 months, which spans two postgraduate years after medical school. JDs are defined as those in their first (PGY 1) or second (PGY 2) postgraduate years. License for full registration is only granted after satisfactory completion of the total of 24 months training, of which 4 months mandatory training in general surgery, including a compulsory rotation in trauma surgery, is required. At present, completion of ATLS is not a mandatory requirement for internship training.
The Study
All JDs who at the time were undertaking their internship training at the PMTS and had not completed or enrolled on an ATLS provider course were eligible for inclusion. A structured survey was issued to each JD to complete. Basic demographic detail collected included the age, gender, postgraduate year level and whether their surgical rotations had been completed. Participants were specifically asked regarding the reason for not having attended the ATLS course during their internship training at our institution to date. Data from the survey were anonymized.
Data analysis
Data were analysed using Stata 13.0 (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP). Frequency tables were used to summarise categorical variables. Association between reasons for non-attendance and PGY level of JDs were assessed using the Fishers exact test as certain expected cell counts contained fewer than 5 observations. A p-value of < 0.05 was considered statistically significant.
Results
Demographics
A total of 105 JDs were available at the time of study. Sixty-two percent were female (65/105) and the mean age was 25 years. Forty-eight percent (50/105) of all JDs were PGY 1s and the remaining 52% were PGY 2s. Sixty-two percent (65/105) of all respondents had completed their mandatory rotation in surgery.
Reason for non-attendance:
The reasons for non-attendance are summarised in Table 1 below.
PGY1s vs PGY2s
A direct comparison of reasons for non-attendance was made between the PGY 1s and PGY 2s, and is summarised in Table 2. A highly significant difference in the distribution of reasons for non-attendance by PGY (Fishers exact p-value < 0.001) was noted.
Internship Training
Among the total of 105 JDs, 90% (95/105), were of the opinion that ATLS should be compulsory for internship training. Seventy-one percent (75/105) of JDs had been encouraged to attend ATLS during their internship training. Forty-three percent (45/105) stated that they had encountered one or more occasions during their on call duty where senior doctors assumed they had completed ATLS. Sixty-two per cent (65/105) believed that on one or more occasions, their patient outcome would likely have improved if they had undergone ATLS training.
Discussion
Globally, ATLS remains the gold standard for trauma care and has been adopted in both developed and developing countries.1 Since its inception, several studies have shown that adoption of the ATLS protocols translates into a reduction of mortality and improved outcome in trauma patients. Ariyanayagam et al. in Trinidad and Tobago were amongst the first to report the reduction in mortality after application of ATLS.3 Hedges et al. from the United States also demonstrated an increase in survival rate among the most severely injured patients specifically in the rural setting.4 Navarro et al. from Spain further noted that preventable or potentially preventable mortality among trauma patients was substantially reduced as a direct result of ATLS implementation.5 A systematic review by Mohammad et al., shows that there is now level I evidence suggesting that ATLS significantly improves the knowledge, clinical skills, organization and priority approaches in the management of trauma patients.6 A study from our own institution demonstrated ATLS also improves the anatomical knowledge of JDs in various key trauma procedures, but only a small proportion of JDs had completed the ATLS course during their internship training.10
Trauma in South Africa has been described as a malignant epidemic, and the resources allocated to trauma care are perennially insufficient.11,12 Although ATLS in South Africa has been promulgated extensively and is enthusiastically endorsed by the trauma community,1,13 limited resources in terms of instructors and facilities restricts the number of courses available. Currently, over 40 courses are held annually in South Africa. The total number of doctors completing medical school is approximately 1 600 annually.14,15 If one assumes that each provider course accommodates 20 candidates, at least 80 courses are required to accommodate this number alone, which does not include doctors who are PGY 2 or above. There is no evidence that the demand for ATLS training is decreasing. Our current study suggested that the primary barriers to accessing ATLS training in our environment is in fact the lack of availability of courses at both regional and national level. Over half of all JDs were unable to secure a place. Doctors working in the emergency department in our setting are often the most junior doctors who have limited experience in trauma. Paradoxically, access to ATLS training for this group of doctors is also the most difficult. We have also shown that financial reasons represent another significant barrier. The current course fee is set at R 4 500 (excluding accommodation and travel expenses). Financial support for professional development training for staff in the public sector is almost non-existent and is often left to the discretion of individual departments. This is further compounded by the chronic staff shortage and major pressure on service provision, which often creates great difficulties in obtaining the appropriate professional development leave. It was clear, though, that the vast majority of JDs were aware of the importance of ATLS and its relevance to their training. Although our study is limited to a single centre experience, the challenges facing JDs are likely to be similar in other units throughout the country. Further studies from other centres, including JDs posted in rural hospitals are likely to provide a better view of the current situation.
While there is controversy regarding the extent of influence of ATLS in the overall survival of patients in different settings,6 the importance of ATLS training is undisputed and is unlikely to diminish in the future. While the reason for the low completion rate of ATLS is likely to be multifactorial, there is an urgent need to improve access to ATLS training courses for JDs in our environment.
Conclusions
The primary barriers for JDs to attending ATLS training are difficulty in accessing the course due to oversubscription, financial reasons, followed by difficulty in obtaining professional development leave due to staff shortage. There is an urgent need to improve access to ATLS training courses for JDs in our environment.
Disclaimer
VY Kong, GV Oosthuizen and DL Clarke are ATLS instructors.
REFERENCES
1. Advanced Trauma Life Support for Doctors. Student Manual. 9th ed. American College of Surgeons Committee on Trauma. Chicago. [ Links ]
2. Degiannis E, Oettle GJ, Smith MD, et al. Surgical education in South Africa. World J Surg. February 2009;33(2):170-3. [ Links ]
3. Ariyanayagam DC, Naraynsingh V, Maraj I. The impact of the ATLS course on traffic accident mortality in Trinidad and Tobago. West Indian Med J. 1992;41:72-4. [ Links ]
4. Hedges JR, Adams AL, Gunnels MD. ATLS practices and survival at rural level III trauma hospitals, 1995-1999. Prehosp Emerg Care. 2002;6:299-305 [ Links ]
5. Navarro S, Montmany S, Rebasa P, Colilles C, Pallisera A. Impact of ATLS training on preventable and potentially preventable deaths. World J Surg. September 2014;38(9):2273-8. [ Links ]
6. Mohammad A, Branicki F, Abu-Zidan FM. Educational and clinical impact of Advanced Trauma Life Support (ATLS) courses: a systematic review. World J Surg. February 2014;38(2):322-9. [ Links ]
7. Ali J, Adam R, Butler AK, et al. Trauma outcome improves following the Advanced Trauma Life Support Program in a developing country. J Trauma. 1993; 34:890-9. [ Links ]
8. Van Olden GD, Meeuwis JD, Bolhuis HW, et al. Advanced trauma life support study: quality of diagnostic and therapeutic procedures. J Trauma. 2004;57:381-4. [ Links ]
9. Hashmi ZG, Haider AH, Zafar SN, et al. Hospital-based trauma quality improvement initiatives: first step toward improving trauma outcomes in the developing world. J Trauma Acute Care Surg. 2013;75:60-8. [ Links ]
10. Kong VY, Oosthuizen GV, Sartorius B, Keene CM, Clarke DL. Correlation between ATLS training and junior doctors' anatomical knowledge of intercostal chest drain insertion. J Surg Educ. July-August 2015;72(4):600-5. [ Links ]
11. Kong VY, Sartorius B, Clarke DL. The selective conservative management of penetrating thoracic trauma is still appropriate in the current era. Injury. January 2015;46(1):49-53. [ Links ]
12. Clarke DL, Thomson SR, Madiba TE, Muckart DJ. Selective conservatism in trauma management: a South African contribution. World J Surg. August 2005;29(8):962-5. [ Links ]
13. Goosen J, Veller M. Trauma and emergency surgery: South African model. World J Surg. August 2008;32(8):1622-5. [ Links ]
14. Bateman C. Doctor shortages: Unpacking the 'Cuban solution'. S Afr Med J. 2013;103(9):603-5. [ Links ]
15. Bezuidenhout MM, Joubert G, Hiemstra LA, et al. Reasons for doctor migration from South Africa. SA Fam Pract. 2009;51(3):211-5. [ Links ]
 Correspondence:
Correspondence:
Victor Yeewai Kong
victorywkong@yahoo.com














