Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Surgery
versão On-line ISSN 2078-5151
versão impressa ISSN 0038-2361
S. Afr. j. surg. vol.55 no.3 Cape Town Set. 2017
VASCULAR SURGERY
Pattern and distribution of peripheral arterial disease in diabetic patients with critical limb ischemia (rutherford clinical category 4-6)
M J Motsumi; N G Naidoo
Vascular Surgery Unit, Groote Schuur Hospital, University of Cape Town, Cape Town, South Africa
ABSTRACT
BACKGROUND: This study investigated the pattern and distribution of peripheral arterial disease in diabetic patients with critical limb ischaemia (CLI) and to stratify the findings according to the patients' risk factor profile, gender and age group.
METHODS: We conducted a one-year prospective descriptive study (January 2014 to December 2014) at Groote Schuur Hospital, University of Cape Town. The research protocol and the informed consent were approved by the Institutional Review Board, and all subjects included in this study gave an informed consent. We included all diabetic patients over the age of 18 years with critical limb ischemia who had pre and post-intervention vascular imaging. The calculated minimum sample size was 63 limbs. We hypothesize that the proportions of arterial segment patency categories and the arterial foot arch status varies according to gender, age group and risk factor combinations in diabetic patients. The Null hypothesis (N0) assumes that the proportions of arterial segment patency categories and arch status are the same in diabetic patients irrespective of gender, age group and risk factor combination. The equality of distribution was analysed using the One Sample Chi-square test. Three risk factor combination groups were analysed: Group 1 (diabetes mellitus, hypertension, dyslipidemia), Group 2 (diabetes mellitus, hypertension, dyslipidemia, ex-smoker) and Group 3 (diabetes mellitus, hypertension, dyslipidemia, smoker.
RESULTS: Seventy-one patients were analysed (38 females and 33 males). We recorded the patency grades (ranging from normal to occlusion) of arteries in all 3 lower extremity arterial segments (aortoiliac; femoropopliteal and tibioperoneal segments). Altogether the patency grades of 820 lower extremity arteries were recorded. Diabetics, collectively, were found to have more severe occlusive disease in the tibioperoneal segment (P < .001). Group 3 patients however, had more severe occlusive disease in the femoropopliteal segment compared to the other subgroups (P < .001). Group 1 and Group 2 patients had more severe occlusive disease in the tibioperoneal segment (P < .001). Females were more likely to have complete foot arches (22/37; P = .004) while males tended to have more incomplete foot arches (17/32; P = .048).
CONCLUSION: Diabetic patients collectively have severe tibioperoneal occlusive disease. However, Group 3 patients tend to have disproportionately more occlusive disease in the femoropopliteal segment (P < .001). Diabetic female patients with CLI are more likely to have a complete arterial foot arch than males (P = .004).
Introduction
The literature tends to support the finding that diabetic patients typically suffer from tibio-peroneal artery occlusive disease 1,2,5,7,9,10 with relative sparing of the foot arteries.1 A few studies dispute these findings in all diabetic patients. 2,3 Some studies have looked at the impact of the integrity of the arterial foot arch and the angiosome concept on below knee bypass outcomes as well as foot ulcer healing rate.4 The findings were statistically significant showing association between rate of foot ulcer healing and the integrity of the arterial foot arch.4 The impression from the literature review is that there is a paucity of information associating the quality of the arterial foot arch and the amputation-free survival or graft patency rates. It is relevant to stratify diabetic patients according to their risk factor profile, age group and gender when assessing the pattern and distribution of peripheral arterial occlusive disease (PAD). We hypothesize that the proportions of arterial segment patency categories and the arterial foot arch status varies according to gender, age group and risk factor combinations in diabetic patients. The Null hypothesis (N0) assumes that the proportions of arterial segment patency categories and arch status are the same in diabetic patients irrespective of gender, age group and risk factor combination. The equality of distribution was analysed using the One Sample Chi-square test.
Methods
We performed a one-year prospective descriptive study (January 2014 to December 2014). The research protocol and the informed consent were approved by the Institutional Review Board, and all subjects included in this study gave an informed consent. The following patients were included in this study: all diabetic patients over the age of 18 years with critical limb ischemia (Rutherford clinical category 4 - 6); all diabetic patients who had baseline vascular imaging. Ethical approval for the study was obtained from both the Departmental and Human Research Ethics Review Committees.
Data were collected into a Microsoft Access database which is password protected and stored on a dedicated computer. The database was custom designed to maintain consistent and good quality data structure.
The segmental classification of lower extremity arterial occlusive disease was observed. Four arteries were identified in each segment: Aortoiliac segment (infrarenal aorta, common iliac artery, external iliac artery and internal iliac artery); Femoropopliteal segment (common femoral artery, profunda femoris artery, superficial femoral artery and popliteal artery); Tibioperoneal segment (tibioperoneal trunk, posterior tibial artery, anterior tibial artery and peroneal artery).
All 12 main arteries on the symptomatic side extending from the infrarenal aorta to the crural arteries had their patencies graded and recorded using a very simple patency grading system.
Patency level grading system for aortoiliac to tibioperoneal arterial segments:
Category 1: Widely patent normal vessel (angiographic image with clean pristine edges).
Category 2: Diffusely diseased but patent (shaggy edges but no dominant stenotic areas).
Category 3: Haemodynamically insignificant occlusive lesions (< 50% stenosis).
Category 4: Haemodynamically significant occlusive lesions (> 50% stenosis).
Category 5: Arterial occlusion.
The arterial foot arch was assessed on pre-interventional digital subtraction angiograms (DSA) and post-interventional DSA after the inflow into the arterial foot arch had been improved. The arterial foot arch is formed when the lateral plantar artery runs across the bases of the metatarsal bones and anastomoses with the dorsalis pedis artery through the deep plantar artery. The foot arch status was assessed as complete if the anastomosis between the lateral plantar artery and the dorsalis pedis artery was intact filling the metatarsal and digital arteries; incomplete if only one artery constituting the plantar arch was observed and absent if no plantar arch vessels were visualised.
The patency grades of arterial segments and the arterial foot arch status were then each stratified according to gender, age groups (< 40 years; 40-54 years and > 55 years) and risk factor combinations of diabetic patients. Three diabetic groups were analysed based on risk factor combinations: Groupl = (diabetes mellitus (DM), hypertension (HPT), dyslipidemia); Group 2= (DM, HPT, dyslipidemia, ex-smoker) and Group 3 = (DM, HPT, dyslipidemia, smoker).
These three groups formed the vast majority of our study group (79%). The remaining diabetic patients were a heterogenous group of risk factors that precluded them from being analysed as a separate group because the numbers were small.
The sample size was calculated using PASS 11 software. The calculated minimum sample size of 63 limbs (756 arteries) was needed to achieve a power of 80% with a target significance level of 0.05. The distribution of lower limb arterial patency categories was analysed using the One Sample Chi-square test (SPSS 22) with our Null hypothesis (N0) assuming that these patency categories occur with equal proportions.
Results
Seventy-six consecutive diabetic patients were enrolled into this study and five were excluded from the study for not having any vascular imaging (these patients were not candidates for revascularization). Therefore seventy-one patients (71 limbs) were analysed (38 females and 33 males). Only one patient was younger than 40 years (female), 16 patients were 40-55 years old and 54 (76%) patients were 55 years or older.
Pattern and distribution of PAD in all diabetic patients
The distribution of patency categories across the three arterial segments is shown on Table 1 and Figure A.
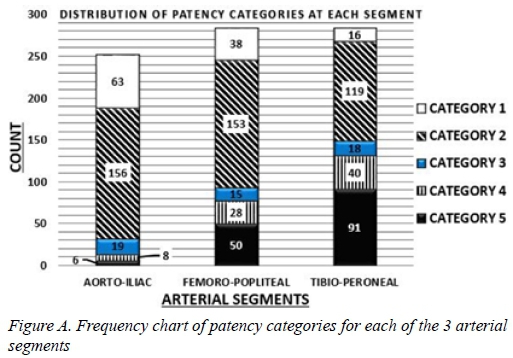
Our observations suggest that the severity of peripheral arterial occlusive disease increases from proximal arterial segments to distal arterial segments (Figure A). Category 3 patency grading is equally distributed across all three lower limb arterial segments emphasising the diffuse nature of PAD in diabetic patients. The distal predominance of category 4 and 5 patency grading is statistically significant (P < .001). The proximal predominance of category 1 and 2 patency grading is also statistically significant (P < .001 and P = 0.05 respectively). Significance levels are shown in Table 1 as asymptotic significance level of chi square test.
Age group stratified pattern and distribution of PAD
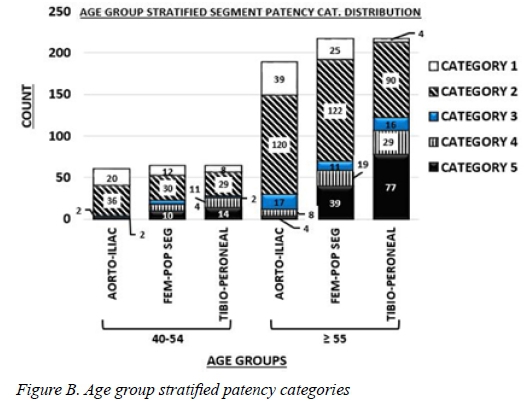
Only one patient was younger than 40 years. There were 12 patency categories recorded for the < 40 years age group, 188 patency categories for the 40-54 age group and 620 patency categories for the > 55 age group.
Figure B shows the distribution of the patency categories across the arterial segments in a bar chart form for the 4054 and > 55 age groups. There is a relative predominance of category 4 and 5 patency levels in the tibioperoneal segment. The observed disproportionate distribution for categories 4 and 5 was statistically significant (P < .001 and P = .003 respectively for the > 55 years age group; P = .013 and P = .019 for the age group of 40-54 (Table 2).
Gender stratified pattern and distribution of PAD
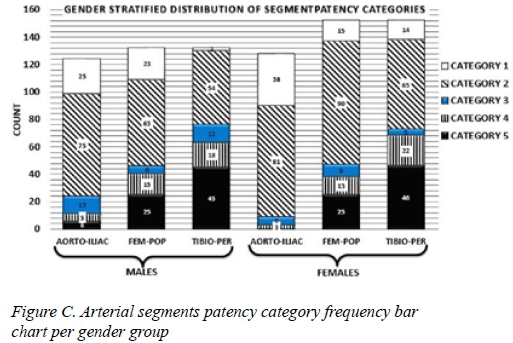
Thirty-eight (38) females and thirty-three (33) males were analysed. The distribution of recorded patency categories according to gender groups was recorded (a total of 388 patency categories were analysed for males and a total of 432 patency categories were analysed for females). Figure C shows the distribution of these patency categories across the three arterial segments in both gender groups. The frequency of category 5 and category 4 increases from proximal to distal segments with predominance in tibioperoneal segments (P < .001, P = .001 respectively for females and P < .001, P = .026 respectively for males). Likewise the widely patent arteries (category 1) are predominantly found in the aortoiliac segment (P < .001 for both females and males). It is worth noting that, though there were more females than males in this study, females had no category 5 lesions (occlusions) in the aortoiliac segment compared to males who had six category 5 lesions in this segment (Figure C.)
Risk factor stratified pattern and distribution of PAD
Three risk factor combinations form the bulk of our patients: Group 1(DM, HPT, Dyslipidemia); Group 2(DM, HPT, dyslipidemia, ex-smoker) and Group 3(DM, HPT, dyslipidemia, smoker). These risk factor combinations accounted for 79% of our patients. The remaining 21% are almost equally distributed amongst the other 4 risk factor combinations and were too small for meaningful statistical analysis. A total of 656 patency categories were described for Groups 1, 2 and 3. Table 3 shows the distribution of patency categories across the arterial segments for the three common risk factor combination diabetic groups. Asymptotic significance levels (P value equivalence) are shown in Table 4. Group 1 and Group 2 displayed the classic observation of significant occlusive disease in the distal arterial segment (Figure D). For Group 1 and 2 patients, category 5 disease (occlusions) dominates the tibioperoneal segment (P < .001).
In contrast Group 3 had a different distribution of category 5 (occlusions) disease (P < .001) with more occlusions noted in the femoropopliteal segment than in the tibioperoneal segment. The other patency grades in Group 3 are almost equally distributed (P > .05) as shown in Figure D.
Arterial foot arch status analysis
The arterial foot arch status was assessed onpre-interventional digital subtraction angiograms (DSA) and post-interventional DSA after the inflow into the arterial foot arch had been improved. The arterial foot arch is formed when the lateral plantar artery runs across the bases of the metatarsal bones and anastomosis with the dorsalis pedis artery through the deep plantar artery. The plantar foot arch was described as complete, incomplete or absent based on vascular imaging studies.
In all diabetic patients in this study, the arterial foot arch was complete in 31 patients; incomplete in 28 patients; absent (occluded) in 10 patients; inconclusive due to sub-optimum imaging of the arterial foot arch (unclassified) in 2 patients.
Disproportionate distribution of the three arterial foot arch patency levels was statistically significant (P = .004). Although the majority of patients had a complete arterial foot arch, the difference between numbers of patients with complete versus incomplete arterial foot arch was not statistically significant. On the other hand, there were significantly fewer patients with absent arterial foot arch (almost three times less compared to the other groups) and this could not be explained by chance alone (P = .004).
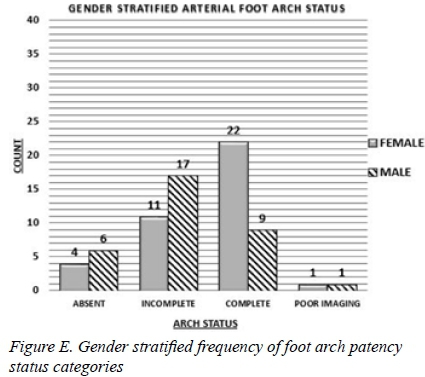
Gender stratification of arch status
On stratifying the foot arch vessels according to gender, we observed that a good proportion of female patients, 22/38 (58%) compared to 9/33 (27%) males, have a complete arterial foot arch. We also observed that more male patients, 6/33 (18%) compared to females 4/38(11%), had absent arterial foot arch. The majority of male patients, 17/33(58%), had an incomplete arterial foot arch. For both females and males there was disproportionate distribution of the arterial foot arch status categories (P = 0.004 females and P = 0.048 males) (Figure E). This disproportionate distribution cannot be explained by chance alone.
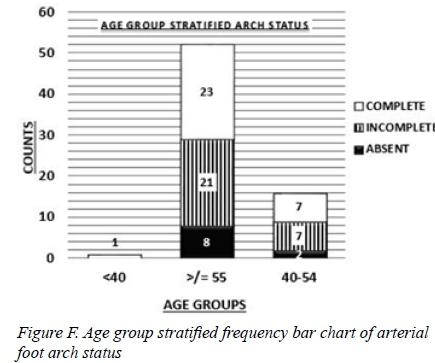
Age group stratified arterial foot arch status
Fifty-three patients were > 55 years of age. In this age group the distribution of the arterial foot arch status patency categories was significantly disproportionate (P = 0.028). Twenty-three patients had a complete foot arch; 21 patients had an incomplete foot arch and 8 patients had an absent arterial foot arch.
Sixteen patients were in the 40-54 year age group. Only 2 patients had absent foot arches and the remaining 14 patients were equally divided between the complete and incomplete arterial foot arch categories.
Only one patient was younger than 40 years and she was noted to have a compete arterial foot arch (Figure F).
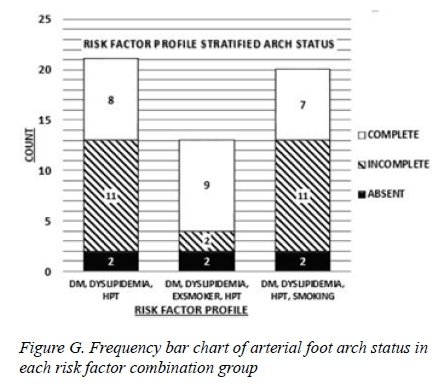
Risk factor profile stratified arch status
The status of the foot arch was analysed according to the three groups of diabetic patients defined previously.
The majority of Group 2 patients (9/13) had complete foot arches ( = .01). The remaining 4 patients were equally distributed between incomplete and absent foot arches. For Group 1 and Group 3 patients the foot arch status showed a predominance of incomplete arterial foot arches, followed by complete foot arches and few absent arterial foot arches (P = .05 and P = .047 respectively) as shown in the Table 4 and Figure G.
Discussion
Research focussing on the pattern and distribution of peripheral arterial disease in diabetic patients attracted much attention with the advent of digital subtraction angiography.1,2 A number of studies reported findings that diabetic patients with peripheral artery occlusive disease have significant occlusive disease of the tibioperoneal segment 1,2,5,7,9,10 and relative sparing of the arterial foot arch.1 However, some studies disagreed with this notion of severe distal arterial segment involvement in diabetic patients 3 and the arterial foot arch sparing.2,3
Analysing the variability of the pattern and distributions of PAD according to risk factor profile, gender and age group would add an additional dimension to our understanding of these observations.
Our study highlighted key findings which are worth mentioning here. In general, we can confirm that we found that diabetic patients have severe occlusive disease involving the tibioperoneal segment. We can also confirm the diffuse nature of atherosclerotic peripheral arterial disease in diabetic patients in general. However, we found that Group 3 patients (DM, HPT, Dyslipidaemia, Smoker) also have quite significant occlusive disease of the femoropopliteal arterial segment. Interestingly, Group 2 patients who have similar risk factor combinations to Group 3 patients, except that they were ex-smokers have less affliction of femoropopliteal segment. This observation seems to suggest that smoking increases the severity of arterial occlusive disease in the femoropopliteal segment or more proximal arterial segments. A study by Diehm et al.9 reported that smoking had a higher relative risk ratio for severe affliction of the aortoiliac segment. An interesting finding in our study was that aortoiliac involvement in female diabetic patients was uncommon, irrespective of risk factor grouping. In analysing the arterial foot arch status, we found that female diabetic patients, significantly, had relative sparing of the arterial foot arch compared to their male counterparts. Male diabetic patients were more likely in our study to have an incomplete foot arch on vascular imaging.
We acknowledge that we have a few shortcomings in our study. We could not make statistically significant conclusions in all age groups analysed mainly because we lacked numbers in the younger age groups. We encountered similar problems when analysing risk factor profile groupings. A common problem highlighted in previous similar studies7 is the lack of standardised reporting criteria for the infra-genicular arterial lesions and foot arch assessment. This is a real problem particularly when trying to compare results during the literature review or when doing a retrospective study on reported infra-genicular vascular imaging.
Future research perspectives should focus on prospectively studying a similar but larger diabetic patient population to enable the analysis of the less common categories such as the younger diabetic patients with critical limb ischaemia and other rare risk factor combination groups. An intriguing question for future research would be, what is it that protects diabetic female patients from significant foot arch involvement?
Conclusion
Diabetic patients in general have severe tibioperoneal occlusive disease. This finding was consistent in both genders, in all patients aged 40 years and older and in the dominant risk factor groupings. Group 3 patients have a different pattern and distribution of peripheral arterial disease, with more severe occlusive disease in the femoropopliteal segment followed by tibioperoneal segment. This seems to suggest that smoking increases the severity of arterial occlusive disease in proximal segments. Female diabetics tends to have a complete arterial foot arch as opposed to male patients who have predominantly incomplete arches. The Group 2 patients have predominantly complete arterial foot arches while Group 1 and Group 3 patients have predominantly incomplete arterial foot arches.
Acknowledgments
The author acknowledges the mentorship of Dr N Naidoo (Head of the Vascular Department at Groote Schuur Hospital, University of Cape Town). He played an important role in supervising the authorship of this paper. To Prof D Kahn, the Head of the Surgical Division, your support is acknowledged.
REFERENCES
1. Karacagil S, Almgren B, Lörelius LE. Angiographic runoff patterns in patients undergoing lower limb revascularization. Acta Chir Scand. 1989;155:19-24. [ Links ]
2. Ciavarella A, Silletti A, Mustacchio A. Angiographic evaluation of the anatomic pattern of arterial obstructions in diabetic patients with critical limb ischaemia. Diabete Metab. 1993;19(6):586-9. [ Links ]
3. Hilfiker M, Vock P, Stirnemann P. Morphological changes of the lower leg arteries and the plantar arch in diabetic and nondiabetic patients with chronic critical ischemia of the leg. Rofo. 1993;158:225-9. [ Links ]
4. Hisham R, Hani S, Hany Z, Dean YH, Jason W, David RE, et al. The impact of arterial pedal arch quality and angiosome revascularization on foot tissue loss healing and infrapopliteal bypass outcome. J Vasc Surg. 2013;57:1219-1226. [ Links ]
5. Karacagil S, Almgren B, Bergqvist D. Patterns of atherosclerotic occlusive disease of lower leg and pedal arteries in hypertensive patients undergoing infrainguinal bypass procedures. Int Angiol. 1996;15:57-60. [ Links ]
6. Kröger K, Buss C, Renzing-Köhler K, Santosa F, Rudofsky G. Segmental manifestation of peripheral atherosclerosis and its association to risk factors. Vasa. 2000;29:199-203. [ Links ]
7. Graziani L, Silvestro A, Bertone V, Manara E, Andreini R, Sigala A, et al. Vascular Involvement in Diabetic Subjects with Ischemic Foot Ulcer. A New Morphologic Categorization of Disease Severity. Eur J Vasc Endovasc Surg. 2007;33:453-460. [ Links ]
8. Margaret EH, James RV, Donald DM, Stuart IM, Arun C, Patrick GC. Age-related differences in the distribution of peripheral atherosclerosis. When is atherosclerosis truly premature? Surg. 1993;118:834-839. [ Links ]
9. Diehm N, Shang A, Silvestro A, Dick F, Schmidli J, Mahler F, et al. Association of Cardiovascular Risk Factors with Pattern of Lower Limb Atherosclerosis in 2659 Patients Undergoing Angioplasty. Eur J Vasc Endovasc Surg. 2006;31:59-63. [ Links ]
10. van der Feen C, Neijens FS, Kanters SD, Mali WP, Stolk RP, Banga JD. Angiographic distribution of lower extremity atherosclerosis in patients with and without diabetes. Eur J Vasc Endovasc Surg. 2000;19:366-70. [ Links ]
 Correspondence:
Correspondence:
Mpapho Joseph Motsumi
josephmotsumi@yahoo.com














