Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Surgery
versión On-line ISSN 2078-5151
versión impresa ISSN 0038-2361
S. Afr. j. surg. vol.55 no.1 Cape Town mar. 2017
CASE REPORT
Primary fusobacterium osteomyelitis and pyomyositis of the thigh in an immunocompetent young adult
G F VlesI; R MagampaII; A BoutallIII; S MaqungoIV
IRegistrar, Department of orthopaedic surgery, Maastricht University Medical Centre, Maastricht, the Netherlands
IIRegistrar, Orthopaedic Trauma Service, Division of Orthopaedic Surgery, Groote Schuur Hospital, Cape Town, South Africa
IIIConsultant, Department of General Surgery, Groote Schuur Hospital, Cape Town, South Africa
IVConsultant, Orthopaedic Trauma Service, Division of Orthopaedic Surgery, Groote Schuur Hospital, Cape Town, South Africa
ABSTRACT
An unusual case of an immunocompetent young adult with osteomyelitis and pyomyositis of his right thigh is presented. Despite the absence of typical clinical signs, a high index of suspicion and 16S RNA PCR led to an early diagnosis of Fusobacterium infection and subsequent successful multidisciplinary treatment
Introduction
Treatment of osteomyelitis (OM) consists of optimizing host factors, surgical debridement, and antibiotic treatment which initially is empirical, but should be reviewed after cultures are obtained. In adults, the organism most commonly found is Staphylococcus aureus.1 Anaerobic, Gram-negative organisms are very seldom encountered, but the predominant types are Bacteroides, Peptostreptococcus, Clostridium spp, P. acnes, and Fusobacterium spp.2 Human infection with the latter is a very rare but well-known clinical entity, which in its most classical form is known as Lemierre's syndrome.3,4 It usually involves healthy young adults who develop a fulminant post-anginal septicemic infection with internal jugular vein thrombophlebitis and septic emboli to distant sites.5 OM caused by hematogenous spread is seen in less than 3 percent and treatment usually commences after Lemierre's syndrome's typical clinical presentation has lead to the diagnosis of Fusobacterium infection.4,6 However, several clinical subtypes of Fusobacterium infection with far less characteristic presentations exist and one such case is described below.
Case summary
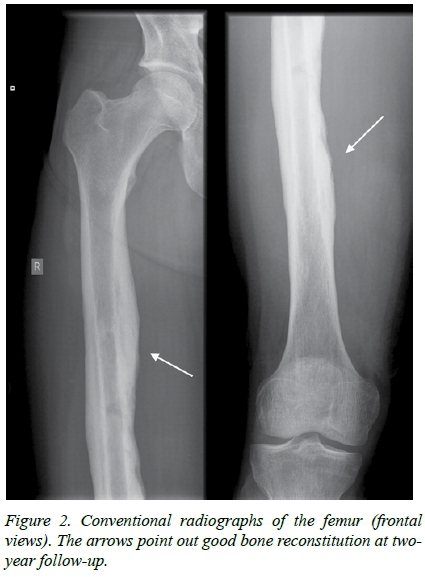
A 23-year-old medical student, with an unremarkable medical history presented with a complaint of low back pain radiating down his right thigh for 2 weeks. He arrived in the ward having severe rigors, a body temperature of 39 degrees Celsius, and exquisite pain on palpating his mid right thigh. A mild fusiform swelling in this region was appreciated, but his compartments were soft and his limb neurovascularly intact. Thorough taking of history and physical examination did not reveal any other abnormalities; in particular no cervical lymphadenopathy or signs of internal jugular vein trombophlebitis could be appreciated, auscultation of his lungs was normal, and he did not recall any episode of oropharyngeal infection. Blood results showed C-Reactive Protein 395 mg/L, White Cell Count 1.9*10A9/L, neutrophils 1.24*10A9/L, leukocytes 0.46*10A9/L, pro-calcitonin > 10 ng/mL. Plain radiographs of the spine, right hip and right femur were normal as were MRI scans of the lumbar spine and pelvis. An MRI scan of the right thigh, however, revealed extensive periosteal and bone marrow edema, multilocular small periosteal-based fluid-collections throughout the femoral shaft, and extensive edematous changes in the soft tissues of the thigh, predominantly in the vastus medialis and biceps femoris muscles (Figure 1). Intravenous Cloxacillin and Ceftriaxone were commenced and the patient was taken to theatre for drainage of muscle abscesses and performing a drill hole in the femur which released foul smelling pus. Samples taken for histology demonstrated partially necrotic bony fragments with proof of inflammation, and no overt signs of a neoplasm. No bacteria grew on initial cultures, but the Gram-stain showed a high count of neutrophils. Blood cultures were repeatedly negative as were tests for HIV, EBV, TBC, and a cardiac ultrasound demonstrated no signs of vegetation on valves. In the meantime, the patient's clinical condition continued to worsen and a second MRI of his thigh showed a deterioration of the area of myositis with large abscesses in the adductor and vastus medialis muscles. He was taken for a repeat incision and drainage and this time tissue samples were sent for 16S RNA PCR which showed Fusobacterium spp. Antibiotic treatment was switched to Clindamycin, after which he showed a dramatic improvement. At the 2-year follow-up, he remained symptom free and radiographs showed good bone reconstitution (Figure 2).
Discussion
Most patients with OM caused by anaerobic organisms have an anaerobic infection elsewhere in their body which is the source of the hematogenous spread.2 With regard to Fusobacterium infection there is usually an antecedent oropharyngeal infection with subsequent severe illness.4 In the case described above, thorough taking of history and physical examination did not reveal any sign of other infectious foci; however, there were also no clues towards extension from infected tissues nearby or direct inoculation into the bone. This phenomenon has been described by Brocar and Guibe who noted that a single shower of bacteremia during an orophyrangeal infection could lead to metastatic manifestations, e.g. lung or liver abscesses, or septic arthritis, weeks or months later.7 Also, Eykyn reported on three patients with bone or joint infection without prior oropharyngeal infection.8
Besides the variable clinical features of Fusobacterium infection, other factors can cause delay in diagnosis and therefore appropriate treatment. Firstly, human Fusobacterium infection is extremely rare and most specialists will not see it during their medical career.9 Secondly, the metastatic manifestations can lead to erroneous diagnoses and in that regard cause initial presentation to a wide variety of specialties. Thirdly, as like many other anaerobic organisms, identification of Fusobacterium can be complicated and time consuming.
Also, the identification of other (aerobic) organisms is quite common and does not exclude Fusobacterium infection.
Nevertheless, prompt diagnosis is essential as mortality rates as high as 29% have been reported.10 Therefore, a high index of suspicion is key. In the case described above, certain clues towards the involvement of an anaerobic organism, in particular Fusobacterium spp, were appreciated. Firstly, the adjacent pyomyositis is seen in almost half of the patients with an anaerobic OM.11 Secondly, the foul odour after making a drill hole in the femur, which has been described by Allston as overripe Camembert cheese, is also present in half of the patients.12 Thirdly, the clinical deterioration of the patient despite surgical debridement and penicillin treatment was an important tip-off, as a significant proportion of Fusobacterium isolates are β-lactamase positive.13 As expected, dramatic improvement was observed after commencement of Clindamycin.
The definitive diagnosis was made using 16S RNA PCR. Routinely, one relies on Gram-staining, bacterial cultures and analysis of biochemical patterns for identification of bacteria. However, cultivating anaerobic organisms poses multiple technical difficulties which could lead to failed or delayed identification.14 Aliya et al. reported on a 27-year-old male with typical Lemierre's syndrome in whom cultures were negative but PCR was able to show Fusobacterium spp.15 Both Kroon et al. and Baills et al. reported on a case of OM of the hip caused by Fusobacterium in which cultures stayed negative and PCR was positive.16,17 Besides a higher yield PCR also has the advantage that previous antibiotic treatment will not interfere with the diagnosis, as is the case with conventional culture methods.1518 Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) is another helpful method for identifying bacteria that are difficult to culture.14
In conclusion, an unusual case of OM with adjacent pyomyositis caused by Fusobacterium spp was presented. Despite the absence of typical clinical signs, a high index of suspicion and 16S RNA PCR led to an early diagnosis of Fusobacterium infection and subsequent successful multi-disciplinary treatment.
Acknowledgements
None
Conflict of interests
The authors declare that there is no conflict of interest regarding the publication of this paper.
Approval by the Research Ethics Committee
NA
Requirements of authorship
All authors contributed substantially to the drafting and critical revision of this case report, and all approved the version to be published.
REFERENCES
1. Lazzarini L, Mader JT, Calhoun JH. Osteomyelitis in Long Bones. J Bone Joint Surg Am. 2004;86:2305--18. Available from: http://dx.doi.org/10.1007/s11908-002-0012-4. PMID: 15466746. [ Links ]
2. Brook I. Microbiology and management of joint and bone infections due to anaerobic bacteria. J Orthop Sci. 2008;13(2):160-9. Available from: http://dx.doi.org/10.1007/s00776-007-1207-1. PMID: 18392922. [ Links ]
3. Lemierre A. On certain septicaemias due to anaerobic organisms. Lancet. 1936(ii);701--3. Available from: http://dx.doi.org/10.1016/S0140-6736(00)57035-4 [ Links ]
4. Riordan T. Human infection with Fusobacterium necrophorum (Necrobacillosis), with a focus on Lemierre's syndrome. Clin Microbiol Rev. 2007;20(4):622--59. Available from: http://dx.doi.org/10.1128/CMR.00011-07. PMID: 17934077. [ Links ]
5. Kuppalli K, Livorsi D, Talati NJ, Osborn M. Lemierre's syndrome due to Fusobacterium necrophorum. Lancet Infect Dis. 2012;12(10):808--15. Available from: http://dx.doi.org/10.1128/CMR.00011-07. PMID: 22633566. [ Links ]
6. Holm K, Svensson PJ, Rasmussen M. Invasive Fusobacterium necrophorum infections and Lemierre's syndrome: the role of trombophilia and EBV. Eur J Clin Microbiol Infect Dis. 2015;34(11):2199--207. Available from: http://dx.doi.org/10.1007/s10096-015-2469-8. PMID: 26272176. [ Links ]
7. Brocard H, Guibe C. Les septice'mies a Bacillus funduliformis. Rev Praticien. 1957;7:1285-300. PMID: 13442380. [ Links ]
8. Eykyn SJ. The therapeutic use of metronidazole in anaerobic infection: six years' experience in a London hospital. Surgery. 1983;93:209-14. PMID: 6849207. [ Links ]
9. Hagelskjaer KL, Prag J. Lemierre's syndrome and other disseminated Fusobacterium necrophorum infections in Denmark: a prospective epidemiological and clinical survey. Eur J Clin Microbiol Infect Dis. 2008;27(9):779--89. Available from: http://dx.doi.org/10.1007/s10096-008-0496-4. PMID: 8330604. [ Links ]
10. Pett E, Saeed K, Dryden M. Fusobacterium species infections: clinical spectrum and outcomes at a district general hospital. Infection. 2014;42(2):363-70. Available from; http://dx.doi.org/10.1007/s15010-013-0564-2. PMID: 2432698. [ Links ]
11. Lewis RP, Sutter VL, Finegold SM. Bone infections involving anaerobic bacteria. Medicine (Baltimore). 1978;57(4):279-305. PMID: 207946. [ Links ]
12. Alston JM. Necrobacillosis in Great Britain. Br Med J. 1955;1524-8. PMID: 13269907. [ Links ]
13. Syed MI, Baring D, Addidle M, Murray C, Adams C. Lemierre syndrome: two cases and a review. Laryngoscope. 2007;117(9):1605--10. Available from: http://dx.doi.org/10.1097/MLG.0b013e318093ee0e. PMID: 17762792. [ Links ]
14. Biswas S, Rolain JM. Use of MALDI-TOF mass spectometry for identification of bacteria that are difficult to culture. J Microbiol Methods. 2013;92(1):14--24. Available from: http://dx.doi.org/10.1016/j.mimet.2012.10.014. PMID: 23154044. [ Links ]
15. Aliyu SH, Yong PF, Newport MJ, et al. Molecular diagnosis of Fusobacterium necrophorum infection (Lemierre's syndrome). Eur J Clin Microbiol Infect Dis. 2005;24(3):226-9. Available from: http://dx.doi.org/10.1007/s10096-005-1298-6. PMID:15776252. [ Links ]
16. Kroon E, Arents NA, Halbertsma FJ. Septic arthritis and osteomyelitis in a 10-year old boy, caused by Fusobacterium nucleatum, diagnosed with PCR/16S ribosomal bacterial DNA amplification. BMJ Case rep. 2012. Available from: http://dx.doi.org/10.1136/bcr.12.2011.5335. PMID: 22605875. [ Links ]
17. Baills M, Freydière AM, Floret D. Septic osteomyelitis of the hip after Fusobacterium necrophorum pharyngitis. Med Mal Infect. 2010;40(9):544--7. Available from: http://dx.doi.org/10.1016/j.medmal.2009.08.024. PMID: 19959308. [ Links ]
18. Patel M. 16S rDNA PCR in diagnosis of Lemierre's syndrome. Lancet Infect Dis. 2013;13(3):197. Available from: http://dx.doi.org/10.1016/S1473-3099(13)70029-X. PMID: 23427889. [ Links ]
 Correspondence:
Correspondence:
Dr Sithombo Maqungo
sithombo@msn.com














